Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(4); 2012 > Article
-
Original Article
Comparison of Diagnostic Cytomorphology of Atypical Squamous Cells in Liquid-Based Preparations and Conventional Smears - Jung Dal Lee1,2, Young-Ha Oh1, Seong Ok Lee2, Jong Yull Kim3
-
Korean Journal of Pathology 2012;46(4):365-369.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.4.365
Published online: August 23, 2012
1Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
2Department of Pathology, Seoul Song-Do Hospital, Seoul, Korea.
3Cell and Tech Bio Corporation, Seoul, Korea.
- Corresponding Author: Jung Dal Lee, M.D. Department of Pathology, Seoul Song-Do Hostpital, 72 Dasan-ro, Jung-gu, Seoul 100-830, Korea. Tel: +82-2-2237-7049, Fax: +82-2-2234-7243, mdljd@hanmail.net
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background
- The aims of this study were to compare the cytomorphologic features diagnostic of atypical squamous cells (ASC) in liquid-based preparations (LBPs) and conventional Pap (CP) smears and to cytomorphologically assess the performance of the Cell Scan 1500™ in cervical cytology practice.
-
Methods
- Cervicovaginal smears were obtained from 938 women. Two smears were obtained simultaneously from each individual, one for an LBP and the other for a CP smear; the smears were independently examined. ASC was diagnosed in 24 patients, and their samples were cytomorphologically and semiquantitatively analyzed.
-
Results
- A total of 24 of the 938 women (2.6%) were diagnosed with ASC by one or both methods. Results from LBPs and CP smears were in agreement in 13 of 24 cases of ASC diagnosis (absolute direct agreement, 54.2%; k<0.20; p-value from chi-square test=0.085). Diagnostic features of ASC in the LBPs included squamous cell atypia and atypical squamous metaplasia.
-
Conclusions
- The cellular features diagnostic of ASC present in one preparation can manifest themselves differently in the other. Changes in individual cells, particularly nuclear changes, are the most reliable features for diagnosing ASC. The Cell Scan 1500™ processor is more effective at detecting ASC than are CP smears.
- Subjects
- A total of 938 women enrolled in an early cervical cancer detection program were subjected to cervicovaginal cytology. All were apparently healthy and had no gynecologic problems during the study period. The mean age was 47.0±10.5 and the age range was 23-84 years.
- Sample preparation
- Two cervical smears were simultaneously prepared from each enrollee, one of which was processed as a CP smear and the other used for an LBP. The samples for the LBP were obtained with a specially designed cytobrush supplied by the manufacturer of the Cell Scan 1500™ (Cell and Tech Bio Corp., Seoul, Korea), an LBP system. After performing the cervical smear, the cytobrush was rinsed and the sample was collected in a proprietary preservative vial (patent obtained). Batched samples were then placed on the preparation workstation. Then a series of preparation steps was automatically performed, including cellular dispersion by agitation, epithelial cell enrichment by filtration, cell transfer to glass slides, and staining.
- Analysis
- To assess the feasibility of using the Cell Scan 1500™ system, the preservation, cellularity, and stain quality of epithelial cells were compared to those of matched conventional samples. Paired LBPs and CP smears were screened separately by two competent cytotechnologists, in a double-blind manner. Smears with a screening diagnosis of ASC were reviewed, cytomorphologic criteria for ASC diagnosis were compiled and semiquantitatively analyzed, and the diagnosis of ASC was checked by a supervisory cytopathologist. ASC interpretations in the two methods were compared and the correlation between matched pairs of LBPs and CP smears was evaluated. Statistical analysis was performed using the chi-square test.15
- Cases of ASC-US were followed up with a second cervical smear and ASC-H cases with a colposcopy/biopsy within 2 weeks. The follow-up results were compared with the initial interpretations.
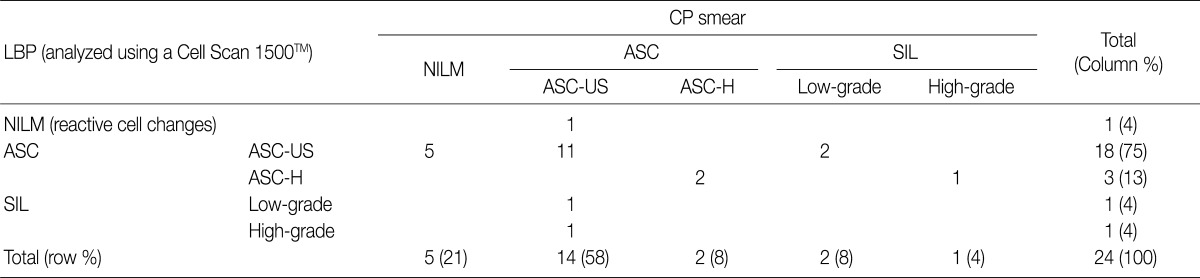
MATERIALS AND METHODS
- Twenty-four cases of ASC were diagnosed in one or both smears (2.56%) from the 938 women. Diagnoses of ASC by LBP accounted for 21 cases (2.24%) and diagnoses by CP smear for 16 cases (1.70%). SILs were diagnosed in 13 smears during the study period (ASC/SIL ratio=1.85:1). There was direct diagnostic agreement between the two methods in 13 of the 24 cases of ASC (absolute direct agreement, 54.2%; k<0.20; p-value from chi-square test=0.085). Five ASC interpretations in the LBPs were initially screened as negative for intraepithelial lesions and malignancy (NILM) in the corresponding CP smears (Table 1).
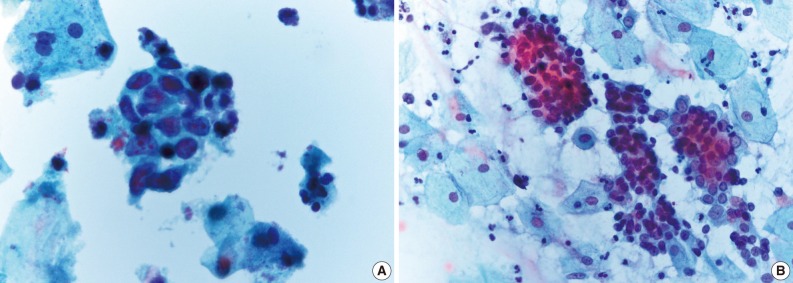
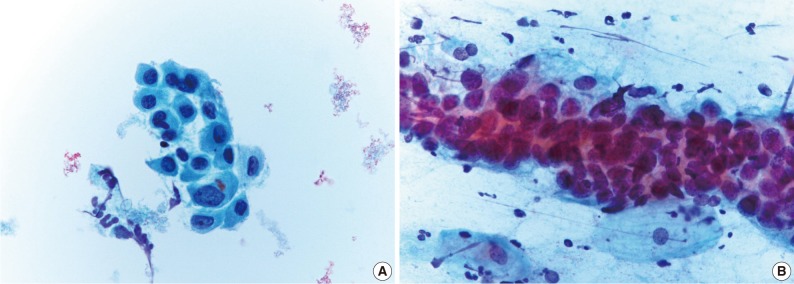
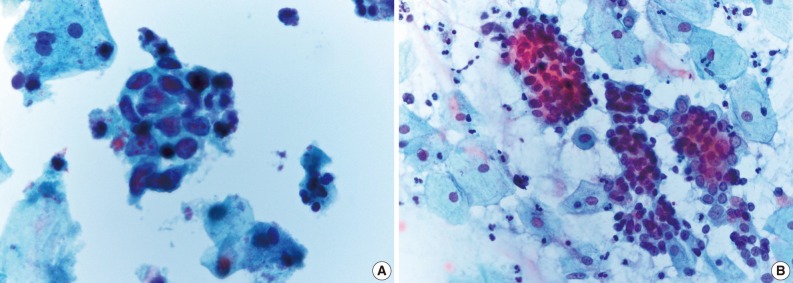
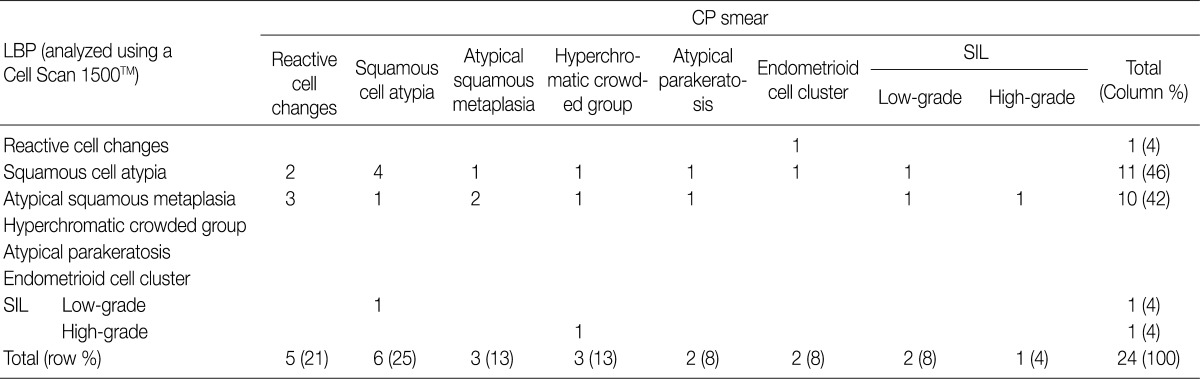
- Table 2 shows the diagnostic cytomorphologic features present in the 24 ASC cases. The diagnostic features common to LBPs and CP smears included squamous cell atypia (Fig. 1) and atypical squamous metaplasia (Fig. 2). These were the two most common cytologic features representative of ASC in LBPs. In contrast, CP smears showed a variety of diagnostic features including hyperchromatic crowded cell groups (Fig. 2B), atypical parakeratosis, and endometrioid cell clusters (Fig. 1B), in addition to the features seen in LBPs. Squamous cell atypia (two cases) and atypical squamous metaplasia (three cases) in the LBPs were initially interpreted as reactive cellular changes in the corresponding CP smears (Table 2).
- Comparison of the performance of the Cell Scan 1500™ with that of conventional smears showed that this system is vastly superior in terms of the preservation of epithelial cells, staining quality, and the elimination of obscuring artifacts. Likely reasons for this superior performance include the fact that Cell Scan 1500™ preparations are made up of uniformly dispersed cells, with backgrounds free of red blood cells, mucus, and overlapping artifacts. However, in the Cell Scan 1500™, the presence of epithelial cells of smaller size and rounded shape and of condensed chromatin and segregated clusters with spiculated margins could be disadvantageous.
RESULTS
- The diagnosis of ASC has a significant clinical impact as approximately 40% of ASC cases are found to be SILs after biopsy, and therefore warrant ongoing follow-up.16,17 Since the introduction of the term "ASCUS" into the 1988 TBS, the cytomorphologic criteria for ASC/ASCUS categorization have been well-documented in many studies and their diagnostic accuracy precisely evaluated.14,18
- Comparative studies of ASC cytomorphology in matched smears obtained from the same individual are rare, and we could find no estimate of the agreement between simultaneously sampled LBPs and CP smears in the literature. Interestingly, our study revealed a difference in ASC detection rates between LBPs (2.24%) and CP smears (1.7%). The low estimate of agreement between the two methods is also significant (absolute direct agreement, 54.2%; k<0.20, poor concordance rate).
- The discrepancy between detection rates is consistent with previous studies, which also found a higher ASC detection rate in LBPs than in CP smears.5,19 The authors of these studies insisted that the majority of discrepancies between screening results and diagnoses based on subsequent biopsies resulted from the inherent problem of sampling error.20 The sampling problems associated with CP smears can be eliminated by using LBPs.21,22 The discrepancies between LBPs and CP smears might be caused by differences in preparation procedures, which could distort cytomorphology in different ways.22 For example, in LBPs, cell clusters are segregated into isolated dispersed cells, whereas in the CP smear procedure, non-random direct smears result in overlapping cell clusters.23 Consistent with this view, the cellular features in CP smears sometimes manifest themselves as different features in LBPs.
- Another explanation for the lower ASC detection rates in CP smears is that this method is susceptible to air-drying artifacts that make cellular features difficult to interpret, whereas this problem is largely eliminated in LBPs.24 In addition, a previous study found that in LBPs, cells were better preserved, but shrinkage and condensation of nuclear details were overinterpreted as ASC. In addition, single dispersed cells originating from hyperchromatic cell clusters due to reserve cell hyperplasia or repair processes could be classified as ASC.25 These could all be factors contributing to the higher ASC detection rates that are observed in LBPs.
- The other reason for the disparity between the two methods is that the diagnostic criteria for ASC have not been well defined.14,17 Because of this, features identified by one method that might actually be diagnostic of ASC are misclassified as negative, whereas the identification of different features by the other method could lead to a positive diagnosis. In our study, hyperchromatic crowded cell groups, which were the most common feature leading to ASC diagnosis in CP smears, were rarely found in the corresponding LBPs. Instead, squamous cell atypia with a dispersed cell pattern was more prevalent in LBPs. For example, atypical squamous metaplasias in LBPs appeared as cytologic mimics in CP smears, and were classified as negative (NILM). These types of artifacts in CP smears could impair correct interpretation and might lead to a false-negative ASC diagnosis. This could explain why higher rates of NILM have been found in CP smears26 and why underdiagnosis rates are lower in LBPs compared to CP smears.
- The LBPs analyzed by the Cell Scan 1500™ system were consistently free of obscuring features. The cells were adequately preserved and evenly dispersed with few overlapping clusters. Consequently, the Cell Scan 1500™ samples were superior to CP smears in detecting ASC based on cervical cytology. The performance of the Cell Scan 1500™ system was comparable to that of monolayer devices from other manufacturers.23 However, we did note cytomorphologic alterations in LBPs that should be taken into consideration to avoid erroneous diagnoses. In LBPs, all of the cells were smaller, chromatin detail was attenuated, and nucleoli were more prominent than in CP smears. These features could lead to misdiagnosis of NILM as ASC.16
DISCUSSION
- 1. The 1988 Bethesda System for reporting cervical/vaginal cytological diagnoses. National Cancer Institute Workshop. JAMA 1989; 262: 931-934. ArticlePubMed
- 2. Solomon D, Davey D, Kurman R, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA 2002; 287: 2114-2119. ArticlePubMed
- 3. Ettler HC, Joseph MG, Downing PA, Suskin NG, Wright VC. Atypical squamous cells of undetermined significance: a cytohistological study in a colposcopy clinic. Diagn Cytopathol 1999; 21: 211-216. ArticlePubMed
- 4. Kim HS, Kim BM, Kim YJ, Kim HS. Qualification of atypical squamous cells of undetermined significance: "ASCUS, R/O HSIL". Cytologic features and histologic correlation. Korean J Cytopathol 2002; 13: 14-20. Article
- 5. Lerma E, Quintana MJ, Quilez M, et al. Effectiveness of liquid-based cytology and papanicolaou tests in a low risk population. Acta Cytol 2007; 51: 399-406. ArticlePubMed
- 6. Jeon YK, Kim OR, Park KW, Kang SB, Park IA. Liquid-based cytology using MonoPrep 2(TM) system in cervicovaginal cytology: comparative study with conventional pap smear and histology. Korean J Cytopathol 2004; 15: 33-39. Article
- 7. Abulafia O, Pezzullo JC, Sherer DM. Performance of ThinPrep liquid-based cervical cytology in comparison with conventionally prepared Papanicolaou smears: a quantitative survey. Gynecol Oncol 2003; 90: 137-144. ArticlePubMed
- 8. Williams ML, Rimm DL, Pedigo MA, Frable WJ. Atypical squamous cells of undetermined significance: correlative histologic and follow-up studies from an academic medical center. Diagn Cytopathol 1997; 16: 1-7. ArticlePubMed
- 9. Bishop JW, Kaufman RH, Taylor DA. Multicenter comparison of manual and automated screening of AutoCyte gynecologic preparations. Acta Cytol 1999; 43: 34-38. ArticlePubMed
- 10. Baker JJ. Conventional and liquid-based cervicovaginal cytology: a comparison study with clinical and histologic follow-up. Diagn Cytopathol 2002; 27: 185-188. ArticlePubMed
- 11. Davey DD, Naryshkin S, Nielsen ML, Kline TS. Atypical squamous cells of undetermined significance: interlaboratory comparison and quality assurance monitors. Diagn Cytopathol 1994; 11: 390-396. ArticlePubMed
- 12. Stoler MH, Schiffman M. Atypical Squamous Cells of Undetermined Significance-Low-grade Squamous Intraepithelial Lesion Triage Study (ALTS) Group. Interobserver reproducibility of cervical cytologic and histologic interpretations: realistic estimates from the ASCUS-LSIL Triage Study. JAMA 2001; 285: 1500-1505. ArticlePubMed
- 13. Ferenczy A, Robitaille J, Franco E, Arseneau J, Richart RM, Wright TC. Conventional cervical cytologic smears vs. ThinPrep smears: a paired comparison study on cervical cytology. Acta Cytol 1996; 40: 1136-1142. ArticlePubMed
- 14. Alli PM, Ali SZ. Atypical squamous cells of undetermined significance: rule out high-grade squamous intraepithelial lesion: cytopathologic characteristics and clinical correlates. Diagn Cytopathol 2003; 28: 308-312. ArticlePubMed
- 15. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159-174. ArticlePubMed
- 16. Lousuebsakul V, Knutsen SM, Gram IT, Akin MR. Clinical impact of atypical squamous cells of undetermined significance: a cytohistologic comparison. Acta Cytol 2000; 44: 23-30. ArticlePubMed
- 17. Gatscha RM, Abadi M, Babore S, Chhieng D, Miller MJ, Saigo PE. Smears diagnosed as ASCUS: interobserver variation and follow-up. Diagn Cytopathol 2001; 25: 138-140. ArticlePubMed
- 18. Morin C, Bairati I, Bouchard C, et al. Cytologic predictors of cervical intraepithelial neoplasia in women with an ASCUS Pap smear. Acta Cytol 2000; 44: 576-586. ArticlePubMed
- 19. Lee KC, Jung CK, Lee A, et al. A comparison of Surepath(TM) liquid-based smear with a conventional smear for cervicovaginal cytology with reference to a histological diagnosis. Korean J Cytopathol 2007; 18: 20-28. Article
- 20. Joste NE, Crum CP, Cibas ES. Cytologic/histologic correlation for quality control in cervicovaginal cytology: experience with 1,582 paired cases. Am J Clin Pathol 1995; 103: 32-34. ArticlePubMed
- 21. Crum CP, Genest DR, Krane JF, et al. Subclassifying atypical squamous cells in Thin-Prep cervical cytology correlates with detection of high-risk human papillomavirus DNA. Am J Clin Pathol 1999; 112: 384-390. ArticlePubMed
- 22. Stoler MH. Advances in cervical screening technology. Mod Pathol 2000; 13: 275-284. ArticlePubMed
- 23. Park J, Jung EH, Kim C, Choi YH. Direct-to-vial comparison of a new liquid-based cytology system, liqui-PREP versus the conventional pap smear. Diagn Cytopathol 2007; 35: 488-492. ArticlePubMed
- 24. Sprenger E, Schwarzmann P, Kirkpatrick M, et al. The false negative rate in cervical cytology: comparison of monolayers to conventional smears. Acta Cytol 1996; 40: 81-89. ArticlePubMed
- 25. Boman F, Farré I, Farine MO, et al. Why we prefer the thin layer technique to conventional Pap smears. A double-blind study of 473 specimens. Clin Exp Pathol 1999; 47: 81-87. ArticlePubMed
- 26. Dvorak KA, Finnemore M, Maksem JA. Histology correlation with atypical squamous cells of undetermined significance (ASCUS) and low-grade squamous intraepithelial lesion (LSIL) cytology diagnoses: an argument to ensure ASCUS follow-up that is as aggressive as that for LSIL. Diagn Cytopathol 1999; 21: 292-295. ArticlePubMed
REFERENCES

ASC, atypical squamous cells; CP, conventional Pap; LBP, liquid-based preparations; NILM, negative for intraepithelial lesion and malignancy; ASC-US, atypical squamous cells of undetermined significance; ASC-H, atypical squamous cells cannot exclude high grade squamous intraepithelial lesion; SIL, squamous intraepithelial lesion.
Figure & Data
References
Citations

- Risikobewertung von Zytologiebefunden im Zervixkarzinom-Screening
Katrin Marquardt, Peter Ziemke, Konrad Neumann, Wolfgang Kühn
Der Gynäkologe.2019; 52(12): 937. CrossRef - Nationwide cervical cancer screening in Korea: data from the National Health Insurance Service Cancer Screening Program and National Cancer Screening Program, 2009–2014
Seung-Hyuk Shim, Hyeongsu Kim, In-Sook Sohn, Han-Sung Hwang, Han-Sung Kwon, Sun Joo Lee, Ji Young Lee, Soo-Nyung Kim, Kunsei Lee, Sounghoon Chang
Journal of Gynecologic Oncology.2017;[Epub] CrossRef - Morphologic Analysis of Cytomegalovirus Infected Cells in Bronchial Washing Cytology: Comparison of Liquid-Based Preparation and Conventional Smear
Jae Yeon Seok, Jungsuk An, Seung Yeon Ha, Dong Hae Chung, Sangho Lee, Hyunchul Kim
Journal of Pathology and Translational Medicine.2016; 50(2): 147. CrossRef


Fig. 1
Fig. 2
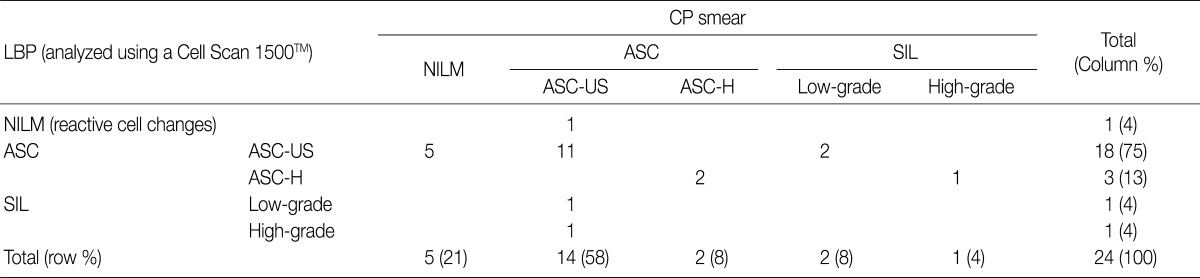
ASC, atypical squamous cells; CP, conventional Pap; LBP, liquid-based preparations; NILM, negative for intraepithelial lesion and malignancy; ASC-US, atypical squamous cells of undetermined significance; ASC-H, atypical squamous cells cannot exclude high grade squamous intraepithelial lesion; SIL, squamous intraepithelial lesion.
ASC, atypical squamous cells; CP, conventional Pap; LBP, liquid-based preparation; SIL, squamous intraepithelial lesion.

 E-submission
E-submission

 PubReader
PubReader Cite this Article
Cite this Article