Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(4); 2014 > Article
-
Brief Case Report
Dedifferentiated Endometrioid Adenocarcinoma of the Uterus: Highly Aggressive and Poor Prognostic Tumor - Shin Young Park, Moon Hyang Park, Hyoung Suk Ko, Eun Jung Cha, Jang Sihn Sohn, Un Suk Jung1, Chul Jung Kim1, Jin Suk Kim2
-
Korean Journal of Pathology 2014;48(4):327-330.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.4.327
Published online: August 26, 2014
Department of Pathology, Konyang University College of Medicine, Daejeon, Korea.
1Department of Obstetrics and Gynecology, Konyang University College of Medicine, Daejeon, Korea.
2Department of Nuclear Medicine, Konyang University College of Medicine, Daejeon, Korea.
- Corresponding Author: Moon Hyang Park, M.D. Department of Pathology, Konyang University Hospital, Konyang University College of Medicine, 158 Gwanjeodong-ro, Seo-gu, Daejeon 302-718, Korea. Tel: +82-42-600-9280, Fax: +82-42-600-9280, parkmh@hanyang.ac.kr
• Received: July 26, 2013 • Revised: September 27, 2013 • Accepted: September 27, 2013
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- A 55-year-old Korean woman was admitted to our hospital because of vaginal bleeding that had lasted eight months. She was well except for a history of left salpingo-oophorectomy for benign ovarian cyst seven years ago. Ultrasonography revealed a thickened endometrium. An endometrial biopsy revealed well-differentiated endometrioid adenocarcinoma. She underwent total hysterectomy with right salpingo-oophorectomy and pelvic lymphadenectomy.
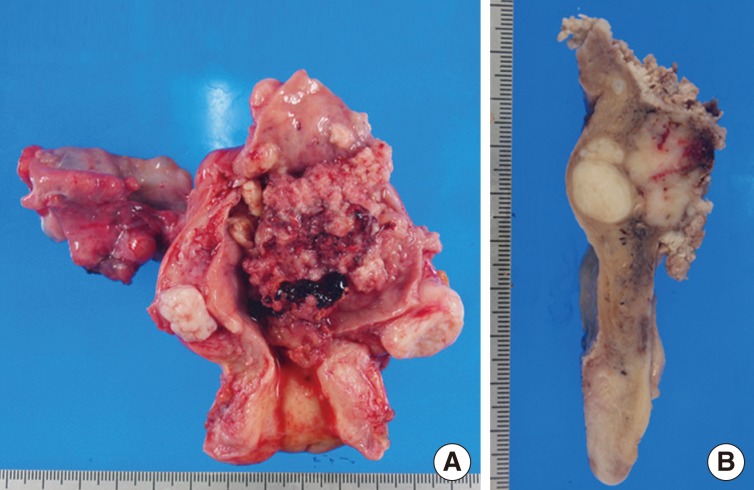
- The uterus measured 8×6×4 cm. Right adnexa was grossly unremarkable. A 7×7×1-cm-sized protruding mass was found in the endometrial cavity. The mass was infiltrating into the myometrium and there were leiomyomas beneath the tumor mass (Fig. 1A, B).
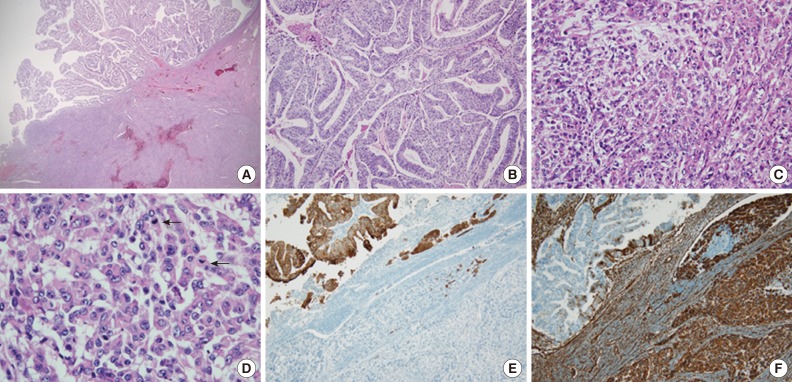
- Microscopically, the tumor consisted of a low-grade endometrioid adenocarcinoma (40% of the tumor volume) on the surface and underlying undifferentiated carcinoma (60%) with a sharp border between the two components (Fig. 2A, B). The undifferentiated component exhibited a solid growth of monomorphic dyscohesive cells, lacking any differentiating features (Fig. 2C). The tumor cells were round with prominent nucleoli and frequent mitosis, and rhabdoid cells with eosinoophilic cytoplasm and eccentric nuclei were noted in myxoid background (Fig. 2D). Numerous vascular and endolymphatic tumor emboli were present. Immunohistochemiscally, cytokeratin (CK), epithelial membrane antigen (EMA), estrogen receptor (ER), and progesterone receptor (PR) were diffusely expressed in the well-differentiated component. The undifferentiated cells were diffusely positive for vimentin and focally positive for CK and EMA (Fig. 2E, F). ER, PR, smooth muscle actin and neuroendocrine markers including chromogranin, synaptophysin, and CD56 were all negative. No metastasis was present in 24 pelvic lymph nodes. According to the International Federation of Gynecology and Obstetrics (FIGO) system, this case was FIGO stage IB.
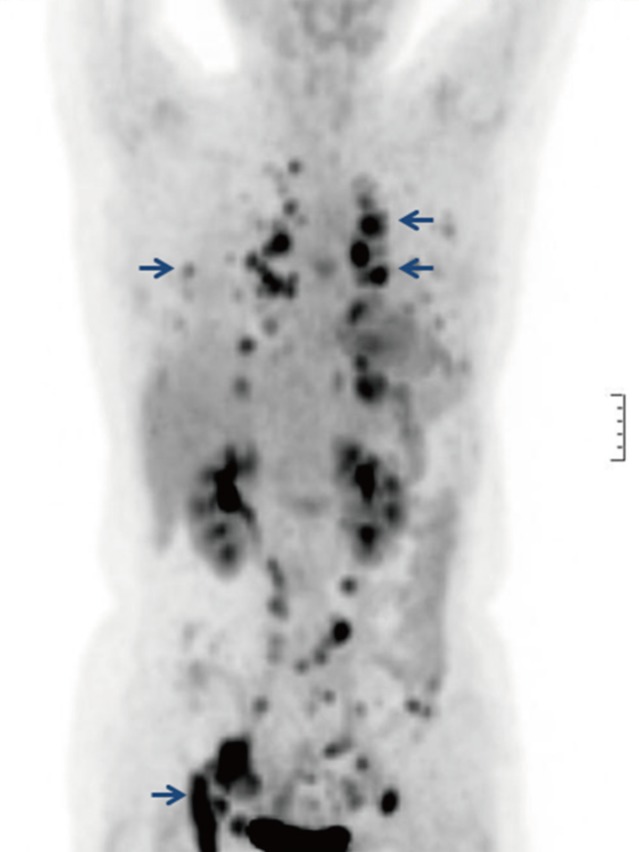
- After surgery, the patient received vaginal radiation. Two months later, she complained of hip pain. A follow-up positron emission tomography-computed tomography revealed multiple pulmonary, peritoneal, pelvic bone, and mediastinal lymph node metastases (Fig. 3). A brain computed tomography revealed multiple metastatic nodules. Although the patient underwent three cycles of chemotherapy, including pacitaxel, cisplatin, and doxorubicin, she died seven months after the diagnosis of DEAC.
CASE REPORT
- Undifferentiated carcinoma of the endometrium is a poorly defined neoplasm. The World Health Organization (WHO) classification defines endometrial undifferentiated carcinoma as a malignant tumor with an epithelial structure that is too poorly differentiated to be placed in any other category of carcinomas.4 The MD Anderson group reviewed 633 cases of endometrial adenocarcinomas and found that cases of undifferentiated carcinoma of the endometrium represent 9% of endometrial carcinomas.2,3 In their series, 71% of cases of undifferentiated carcinoma were admixed with low-grade endometrioid adenocarcinoma referred to as DEAC.2,3 They suggested that the undifferentiated carcinoma originated secondary to the transformation or the dedifferentiation of the low-grade endometrioid adenocarcinoma.2 A recent study suggests that undifferentiated carcinoma is associated with a defect in the DNA mismatch repair pathway, as in Lynch syndrome.5
- Dedifferentiation refers to the progression of cells toward a less differentiated state in which the original line of differentiation is no longer evident.5 Dedifferentiation was first proposed by Dahlin and Beabout in 19716 when they described dedifferentiated chondrosarcoma as a distinct clinicopathological entity characterized by a low-grade chondrosarcoma juxtaposed to a histologically different high-grade sarcoma.6 Lately, dedifferentiation has been recognized in a variety of epithelial malignancies, including those affecting salivary gland, kidneys, and thyroid.7
- DEAC is part of the spectrum of undifferentiated carcinomas of the endometrium. The biological behavior of DEAC is determined by the undifferentiated component. The presence of even a small undifferentiated component appears to be associated with poor clinical outcomes.2
- Patients with undifferentiated carcinoma often present with advanced stage disease, and more than 60% of these patients die from the disease within five years of being diagnosed.8
- Taraif et al.9 reported that 80% of patients died within 12 months of diagnosis. In our case, the pathological stage was low at the time of the surgery. However, despite postoperative chemoradiation therapy, the patient died seven months after the diagnosis due to extensive tumor metastasis.
- The undifferentiated component of DEAC can be misdiagnosed as the solid component of a FIGO grade 3 endometrioid adenocarcinoma. FIGO grade 3 endometrioid adenocarcinoma always exhibits a solid growth pattern, with focal glandular differentiation.3 The nuclear features of tumor cells in both the glandular and the solid areas tend to be cytologically similar.1 In contrast, the solid areas in DEAC are characterized by dyshesive cells which grow in a sheet-like sarcomatoid pattern. The cytological features of the undifferentiated and differentiated components are distinct. Usually, the differentiated components tend to be superficial, whereas the undifferentiated components are deep and invade the myometrium.10 These two components often display an abrupt transition which resembles a collision tumor. As in this case, the immunohistochemical expression of CK and EMA are diffusely positive in FIGO grade 3 endometrioid adenocarcinoma, whereas the expression of CK and EMA is focal (<10%) in the solid area of DEAC.
- The undifferentiated component of DEAC can be confused with other tumors, including carcinosarcoma, undifferentiated endometrial sarcoma, poorly differentiated neuroendocrine carcinoma, and lymphoma. DEAC can be misdiagnosed as carcinosarcoma due to its biphasic appearance. The sarcomatous component of a carcinosarcoma is usually composed of spindle cells, and the epithelial component usually consists of high grade tumor cells.10 Undifferentiated endometrial sarcomas are frequently much more pleomorphic and at least focally spindled.10 Neuroendocrine carcinomas and lymphomas can be differentiated on the basis of their immunohistochemistry.
- In summary, DEAC is an uncommon, highly aggressive, and frequently misdiagnosed tumor. The recognition of the undifferentiated component associated with low-grade endometrioid adenocarcinoma is very important. A range of differentials needs to be considered and ruled out on the basis of the clinical profile, morphology, and immunohistochemical features of this tumor.
DISCUSSION
- 1. Shen Y, Wang Y, Shi Y, Liu J, Liu Y. Clinicopathologic study of endometrial dedifferentiated endometrioid adenocarcinoma: a case report. Int J Clin Exp Pathol 2012; 5: 77-82. PubMedPMC
- 2. Silva EG, Deavers MT, Bodurka DC, Malpica A. Association of low-grade endometrioid carcinoma of the uterus and ovary with undifferentiated carcinoma: a new type of dedifferentiated carcinoma? Int J Gynecol Pathol 2006; 25: 52-58. ArticlePubMed
- 3. Altrabulsi B, Malpica A, Deavers MT, Bodurka DC, Broaddus R, Silva EG. Undifferentiated carcinoma of the endometrium. Am J Surg Pathol 2005; 29: 1316-1321. ArticlePubMed
- 4. Silverberg SG, Mutter GL, Kurman RJ, Kubik-Huch RA, Nogales FF, Tavassoli FA. Tumours of the uterine corpus. Epithelial tumours and related lesions. In: Tavassoli FA, Debelee P, eds. World Health Organization classification of tumors. Pathology and genetics. Tumors of the breast and female genital organs. Tumors of the uterine corpus. Lyon: IARC Press, 2003; 277.
- 5. Katoh M, Shaw C, Xu Q, et al. An orderly retreat: Dedifferentiation is a regulated process. Proc Natl Acad Sci U S A 2004; 101: 7005-7010. ArticlePubMedPMC
- 6. Dahlin DC, Beabout JW. Dedifferentiation of low-grade chondrosarcomas. Cancer 1971; 28: 461-466. ArticlePubMed
- 7. Vita G, Borgia L, Di Giovannantonio L, Bisceglia M. Dedifferentiated endometrioid adenocarcinoma of the uterus: a clinicopathologic study of a case. Int J Surg Pathol 2011; 19: 649-652. ArticlePubMedPDF
- 8. Silva EG, Deavers MT, Malpica A. Undifferentiated carcinoma of the endometrium: a review. Pathology 2007; 39: 134-138. ArticlePubMed
- 9. Taraif SH, Deavers MT, Malpica A, Silva EG. The significance of neuroendocrine expression in undifferentiated carcinoma of the endometrium. Int J Gynecol Pathol 2009; 28: 142-147. ArticlePubMed
- 10. Tafe LJ, Garg K, Chew I, Tornos C, Soslow RA. Endometrial and ovarian carcinomas with undifferentiated components: clinically aggressive and frequently underrecognized neoplasms. Mod Pathol 2010; 23: 781-789. ArticlePubMedPDF
REFERENCES
Fig. 1Gross photographs of dedifferentiated endometrioid adenocarcinoma. The uterine corpus is occupied by a huge polypoid mass that fills the endometrial cavity (A), and an underlying solid mass infiltrates less than one half of the myometrium with two underlying leiomyomas (B).
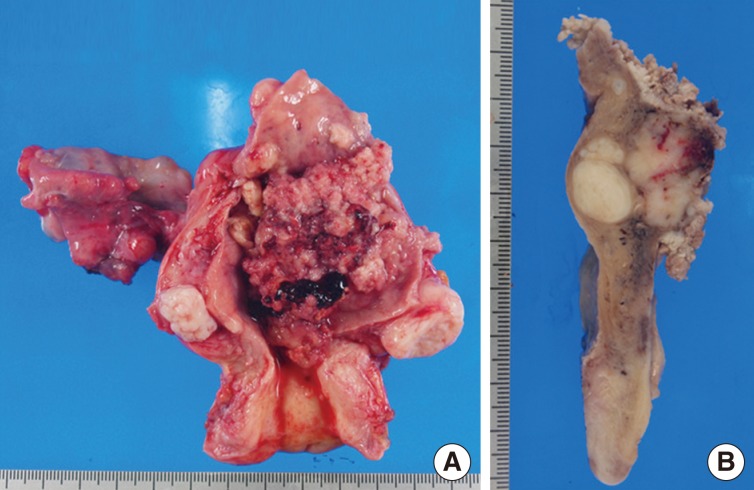
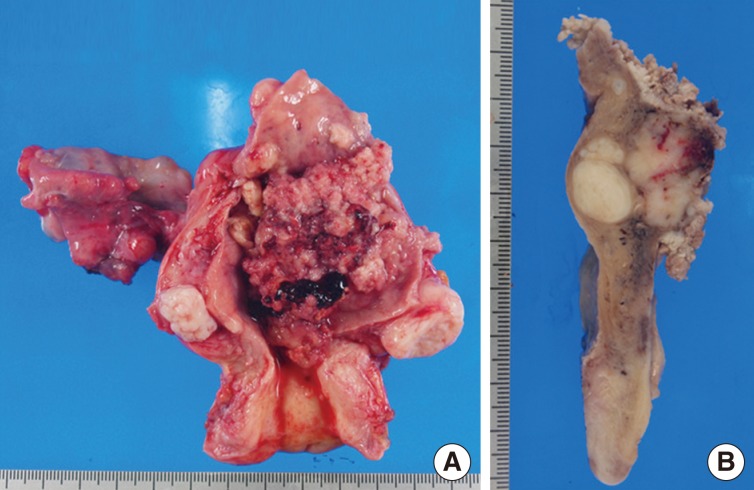
Fig. 2Dedifferentiated endometrial adenocarcinoma (A-D). (A) The transition between low grade endometrioid adenocarcinoma and undifferentiated carcinoma is abrupt with a sharp border. Superficial area is composed of low-grade endometrioid adenocarcinoma (B), and deep undifferentiated area consists of monotonous undifferentiated cells, forming a solid sheet without a specific pattern (C). (D) The undifferentiated carcinoma shows dyshesive round cells with rhabdoid features, prominent nucleoli, and numerous mitotic figures (arrows). The differentiated component is diffusely positive for cytokeratin (E) and focally positive for vimentin (F). On the contrary, tumor cells in the undifferentiated area are focally positive for cytokeratin and diffusely positive for vimentin.
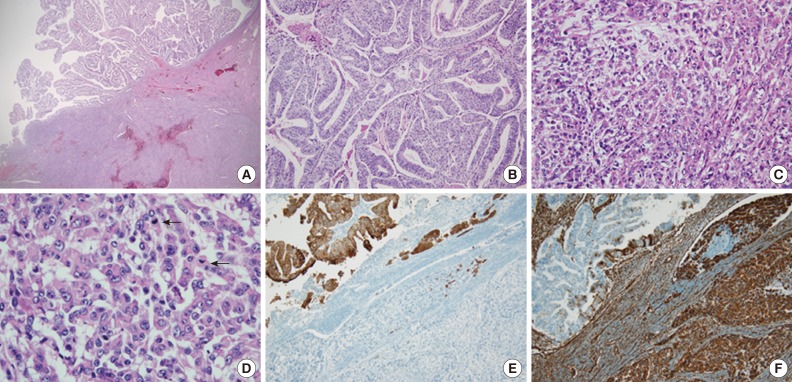
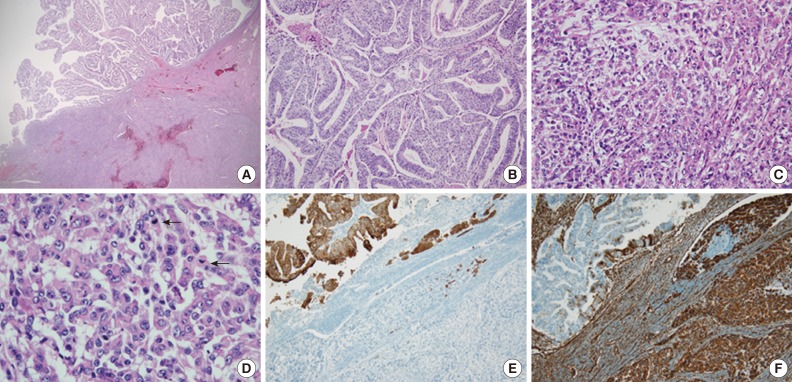
Figure & Data
References
Citations
Citations to this article as recorded by 

- Treatment and outcomes in undifferentiated and dedifferentiated endometrial carcinoma
Sarah Nicole Hamilton, Anna V. Tinker, Janice Kwon, Peter Lim, Iwa Kong, Sona Sihra, Martin Koebel, Cheng Han Lee
Journal of Gynecologic Oncology.2022;[Epub] CrossRef - Cytological aspects of an endometrial dedifferentiated carcinoma that was associated with a highly aggressive clinical course
Takako WAKAHARA, Sumiyo ADACHI, Kyota HANAMI, Takayoshi KOYASU, Yoshimitsu RYO, Kazunori FUGO, Kazuto YAMAZAKI
The Journal of the Japanese Society of Clinical Cytology.2022; 61(6): 385. CrossRef - Cytologic features of undifferentiated and dedifferentiated carcinomas of the endometrium
Amir‐Hossein Akbari, Lu Wang, Robert A. Soslow, Rajmohan Murali
Cancer Cytopathology.2021; 129(2): 121. CrossRef - Magnetic resonance imaging findings in 11 cases of dedifferentiated endometrial carcinoma of the uterus
Nao Kikkawa, Kimiteru Ito, Hiroshi Yoshida, Mayumi Kobayashi Kato, Yuko Kubo, Yasuyuki Onishi, Haruto Sugawara, Tomoyasu Kato, Masahiko Kusumoto
Japanese Journal of Radiology.2021; 39(5): 477. CrossRef - High-grade Endometrial Carcinomas: Morphologic and Immunohistochemical Features, Diagnostic Challenges and Recommendations
Rajmohan Murali, Ben Davidson, Oluwole Fadare, Joseph A. Carlson, Christopher P. Crum, C. Blake Gilks, Julie A. Irving, Anais Malpica, Xavier Matias-Guiu, W. Glenn McCluggage, Khush Mittal, Esther Oliva, Vinita Parkash, Joanne K. L. Rutgers, Paul N. Staat
International Journal of Gynecological Pathology.2019; 38(Supplement): S40. CrossRef - Dedifferentiated endometrial adenocarcinoma with neuroendocrine differentiation and ballooning-cell features: Report of a rare entity with an unusual histology
Sara Makhdoum, M. Ruhul Quddus, Michele M. Lomme, Katrine Hansen, W. Dwayne Lawrence
Human Pathology: Case Reports.2019; 15: 92. CrossRef - Unique Molecular Features in High-Risk Histology Endometrial Cancers
Pooja Pandita, Xiyin Wang, Devin E. Jones, Kaitlyn Collins, Shannon M. Hawkins
Cancers.2019; 11(11): 1665. CrossRef - Dedifferentiated endometrioid adenocarcinoma with trophoblastic components and elevated serum alfa-fetoprotein
He Cai, Rong Zhou, Wanying Liang, Jianliu Wang
Medicine.2018; 97(17): e0551. CrossRef - Dedifferentiated endometrioid carcinoma of the uterus : report of four cases and review of literature
Jiheun Han, Eun Young Ki, Sung Eun Rha, SooYoung Hur, Ahwon Lee
World Journal of Surgical Oncology.2017;[Epub] CrossRef - Spontaneous Tumor Lysis Syndrome in a Patient with a Dedifferentiated Endometrial Adenocarcinoma
Shinichi Harada, Keiki Nagaharu, Youichirou Baba, Tetsuya Murata, Toshiro Mizuno, Keiki Kawakami
Case Reports in Oncological Medicine.2017; 2017: 1. CrossRef - Ampullary carcinosarcoma with osteosarcomatous, small cell neuroendocrine carcinoma and conventional adenocarcinoma components; First report
Pallavi Rao, Sadiq S. Sikora, Srikanth Narayanaswamy, Nandita Ghosal, Dinesh Kini
Pathology - Research and Practice.2016; 212(11): 1071. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Dedifferentiated Endometrioid Adenocarcinoma of the Uterus: Highly Aggressive and Poor Prognostic Tumor



Fig. 1 Gross photographs of dedifferentiated endometrioid adenocarcinoma. The uterine corpus is occupied by a huge polypoid mass that fills the endometrial cavity (A), and an underlying solid mass infiltrates less than one half of the myometrium with two underlying leiomyomas (B).
Fig. 2 Dedifferentiated endometrial adenocarcinoma (A-D). (A) The transition between low grade endometrioid adenocarcinoma and undifferentiated carcinoma is abrupt with a sharp border. Superficial area is composed of low-grade endometrioid adenocarcinoma (B), and deep undifferentiated area consists of monotonous undifferentiated cells, forming a solid sheet without a specific pattern (C). (D) The undifferentiated carcinoma shows dyshesive round cells with rhabdoid features, prominent nucleoli, and numerous mitotic figures (arrows). The differentiated component is diffusely positive for cytokeratin (E) and focally positive for vimentin (F). On the contrary, tumor cells in the undifferentiated area are focally positive for cytokeratin and diffusely positive for vimentin.
Fig. 3 Follow-up positron emission tomography-computed tomography. Multiple pulmonary and pelvic bone metastases, peritoneal seeding, and mediastinal lymph node metastases are shown (arrows).
Fig. 1
Fig. 2
Fig. 3
Dedifferentiated Endometrioid Adenocarcinoma of the Uterus: Highly Aggressive and Poor Prognostic Tumor

 E-submission
E-submission