Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(5); 2014 > Article
-
Brief Case Report
Cytotoxic Variant of Mycosis Fungoides with CD8+ CD56+ Phenotype: A Case Report and Review of Literature - Meeran Kim, Moon Il Park, Myung Lim1, Jinman Kim,
-
Korean Journal of Pathology 2014;48(5):390-393.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.5.390
Published online: October 27, 2014
Departments of Pathology, Chungnam National University Hospital, Daejeon, Korea
1Departments of Dermatology, Chungnam National University Hospital, Daejeon, Korea
- Corresponding Author: Jinman Kim, M.D. Department of Pathology, Regional Cancer Center, and Infection Signaling Network Research Center, Chungnam National University School of Medicine, 266 Munhwa-ro,Jung-gu, Daejeon 301-747, Korea Tel: +82-42-580-8237, Fax: +82-42-581-5233, E-mail: jinmank@cnu.ac.kr
• Received: September 9, 2013 • Accepted: October 15, 2013
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
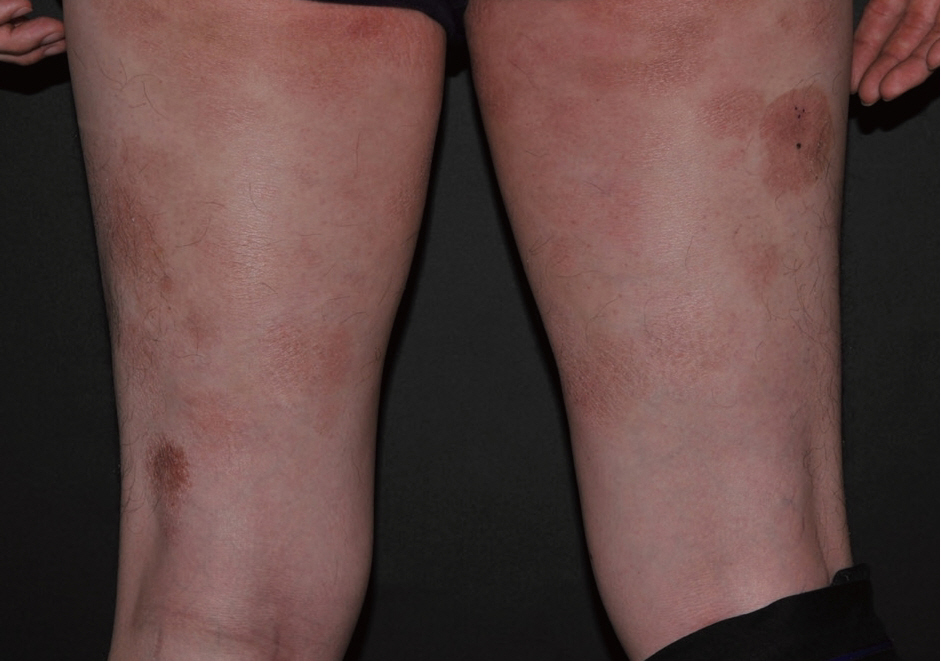
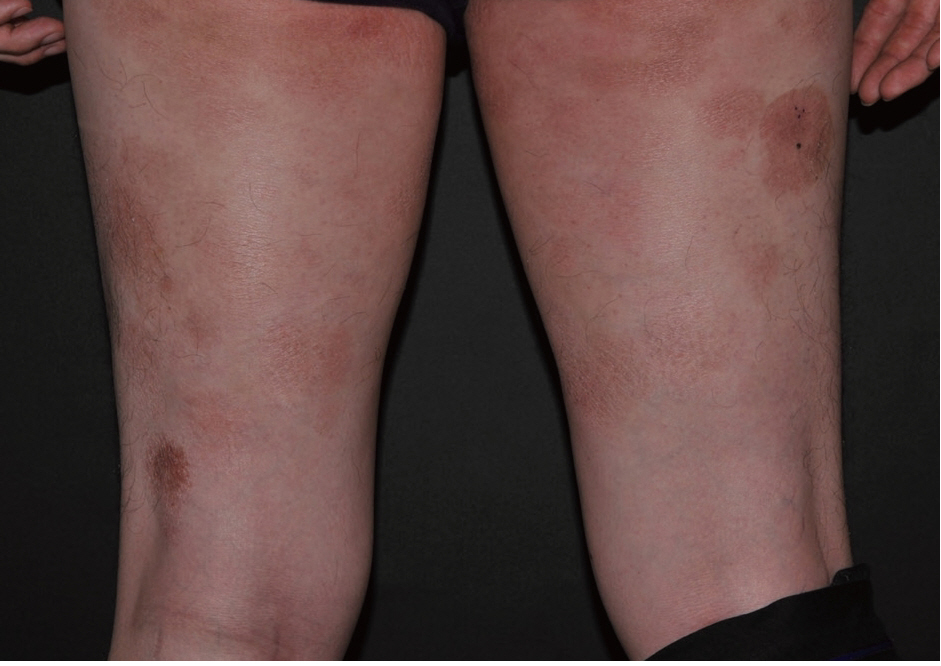
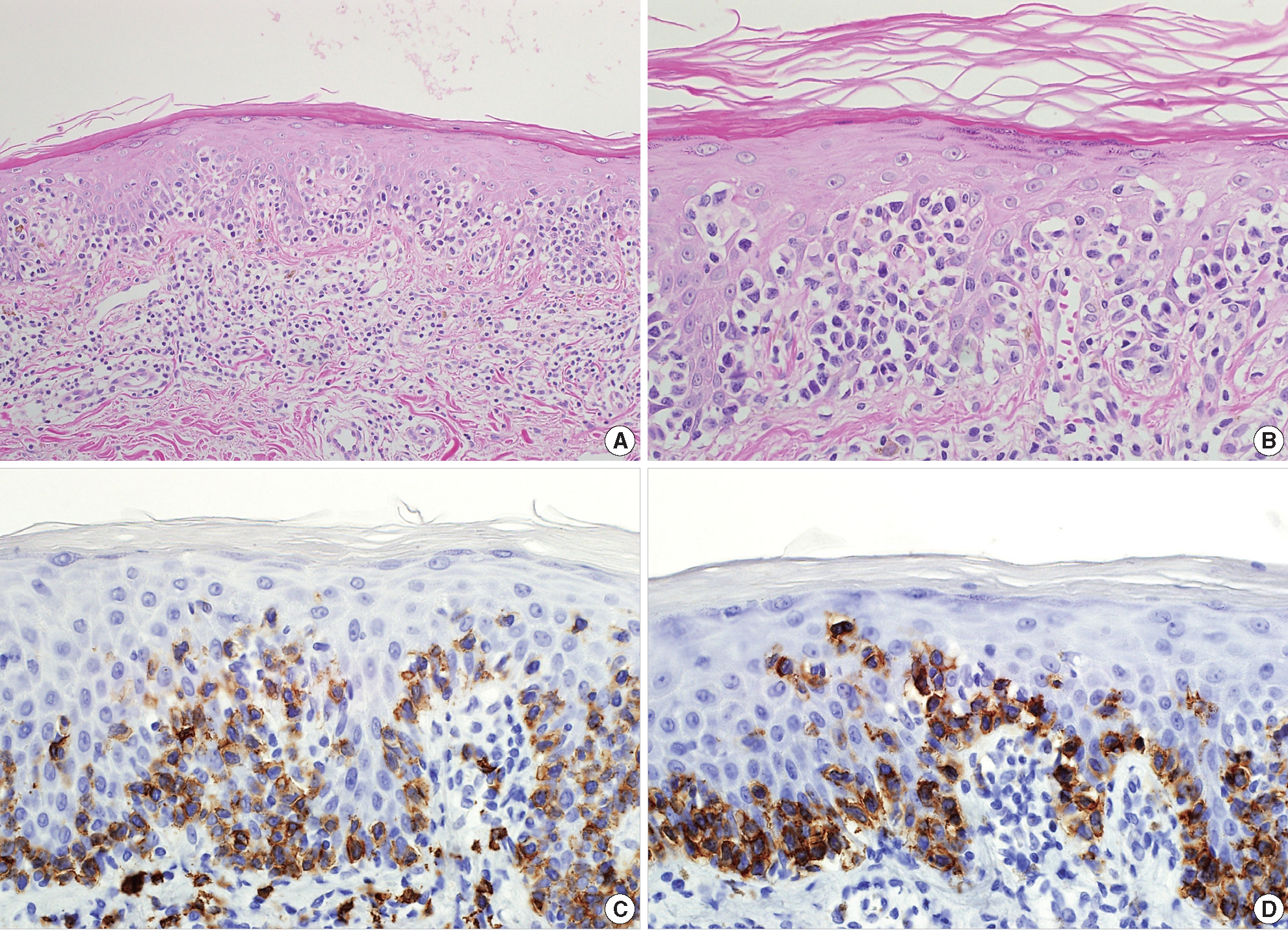
- A 40-year-old male presented with a 5-year history of multiple round erythematous to dusky, brownish scaly patches with mild pruritus (Fig. 1). The skin involvement measured about 30% of total body surface. The lesions appeared first on the buttock and thigh, and lately on the upper arm. The skin lesions did not respond to topical corticosteroid treatment, at which time, he visited our hospital. A skin biopsy was taken from the thigh. The specimen showed a prominent band-like lymphocytic infiltration in the superficial dermis with epidermotropism (Fig. 2A). The epidermotropic lymphocytes were small- to medium-sized with an irregular nuclear membrane and coarse chromatin (Fig. 2B). The immunophenotype of the cells in the epidermis and a few cells in the superficial dermis were CD3+, CD4–, CD8+, CD56+, CD30–, and CD20– (Fig. 2C, D). The majority of lymphocytes in the superficial dermis were not atypical, in contrast to the epidermotropic lymphocytes, and were positive for CD4 and CD8. The neoplastic cells were positive for beta F1 (a marker of alpha/beta T lymphocytes) and granzyme B. An Epstein-Barr virus–encoded small non-polyadenylated RNA-1 (EBER-1) signal was not detected. Lactate dehydrogenase was elevated to 432 IU/L (range, 200 to 400 IU/L). Laboratory blood tests revealed an elevated, total cholesterol level of 235 mg/dL (range, 125 to 220 mg/mL). Complete blood cell count and other results of blood chemistry were within the normal range. The chest X-ray and positron emission tomography–computed tomography revealed no abnormal findings and there was no lymphadenopathy. The patient was diagnosed as having the stage IB, CD8+, CD56+ cytotoxic immunophenotype variant MF. He was treated with narrowband ultraviolet B therapy and his condition was stabilized.
CASE REPORT
- Prognosis of classic MF depends on stage, and, in particular, on the type and extent of skin lesions, as well as the presence of extracutaneous disease[1]. Patients with limited patch/plaque-stage MF have a similar life expectancy to an age, sex, and race-matched control population[1]. However, the prognosis of MF with the cytotoxic phenotype, especially when it express CD56, is not well established.
- To date, there are 8 cases of CD56-expressing MF reported in the current literature, and our case is the ninth case report. The immunohistochemical and clinical characteristics of these cases are summarized in Tables 1 and 2. Among the nine cases, six cases co-expressed CD8 in a majority of the neoplastic cells, one co-expressed CD8 in a minority of neoplastic cells, and two were negative for CD8. One out of nine cases was positive for CD4. Age range was broad, from 6- to 85-years-old. Eight cases were females and our case was the only male case. Poikiloderma was the most frequent clinical feature at the time of diagnosis. Seven cases showed good response to the therapy while two cases, including our case, showed limited response. None of the cases, including our case, had an aggressive clinical course. This result suggests that CD56+ MF is a disease with good prognosis similar to classic MF.
- Several reports of MF with CD8+ and/or CD56+ expression have suggested that this variant would have no prognostic difference compared with classic MF[2,3,5,7-10]. Massone et al.[9] analyzed 73 biopsy specimens from 68 patients with early MF and divided them into four groups based on the immunophenotype. They stated that there was no statistical difference between the survival curves of the four groups, and therefore concluded that cytotoxic phenotype does not have any prognostic significance.
- In our case, with the observed immunophenotype, we considered different diagnoses including primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma, primary cutaneous gamma/delta T-cell lymphoma, and extranodal NK/T-cell lymphoma, nasal type. We were able to rule out these different diagnoses based on the following: clinical course and presentation, beta F1 positivity, and EBER-1 negativity.
- In conclusion, we present a case of a cytotoxic variant of MF with a CD8+, CD56+ immunophenotype. MF with cytotoxic immunophenotype is characterized by a typical clinical presentation, histology, and course of MF. Clinical presentation and course should be a primary consideration in diagnosis. We emphasize that it is important to recognize this rare variant of MF and to distinguish it from other aggressive cutaneous lymphomas to avoid aggressive treatment.
DISCUSSION
Acknowledgments
Fig. 2.(A) The specimen shows a prominent band-like lymphocytic infiltration with epidermotropism. (B) The epidermotropic lymphocytes are small- to medium-sized with an irregular nuclear membrane and coarse chromatin. These cells display the cytotoxic phenotype, showing CD8 (C) and CD56 (D) immunoreactivity.
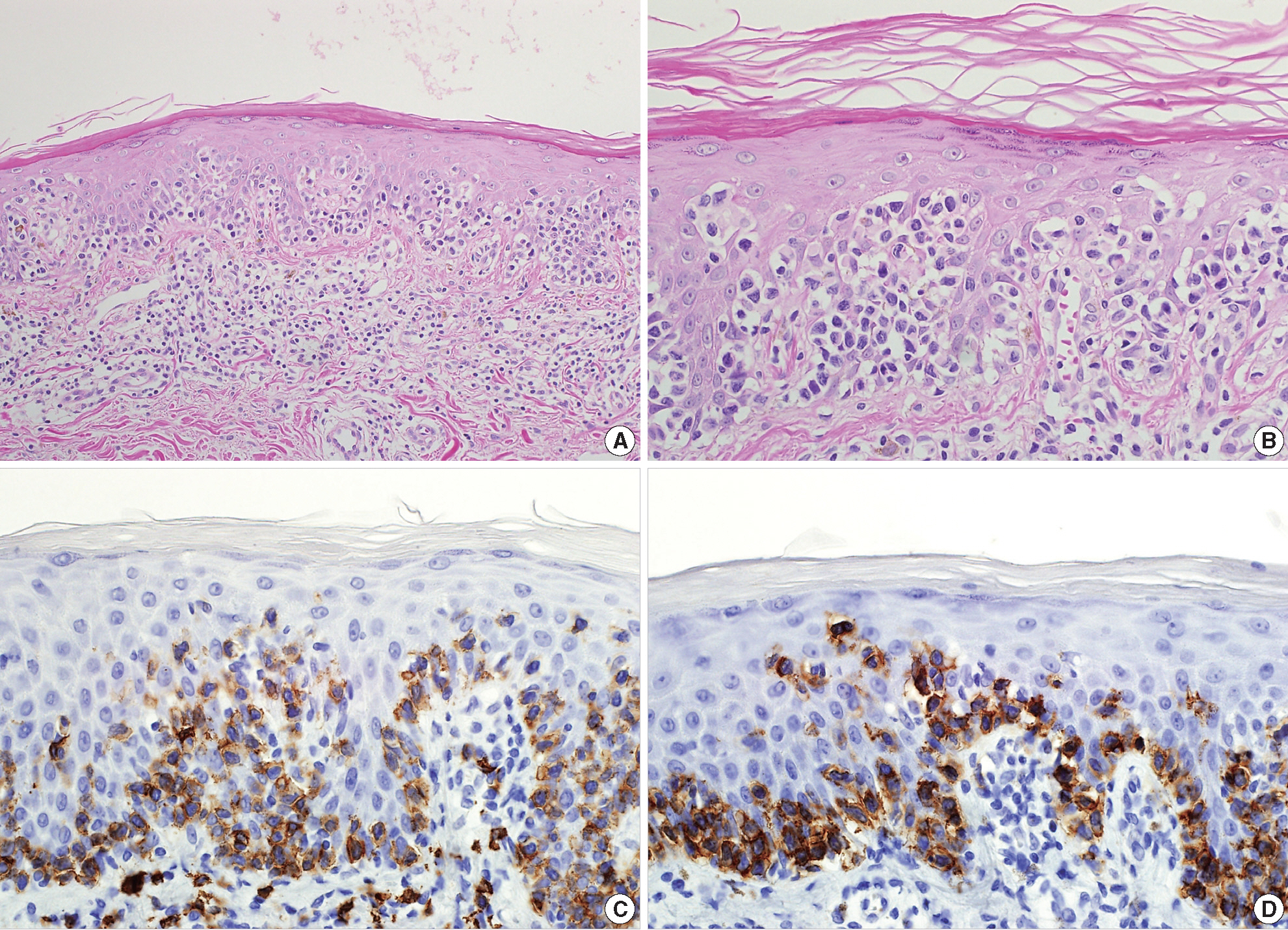
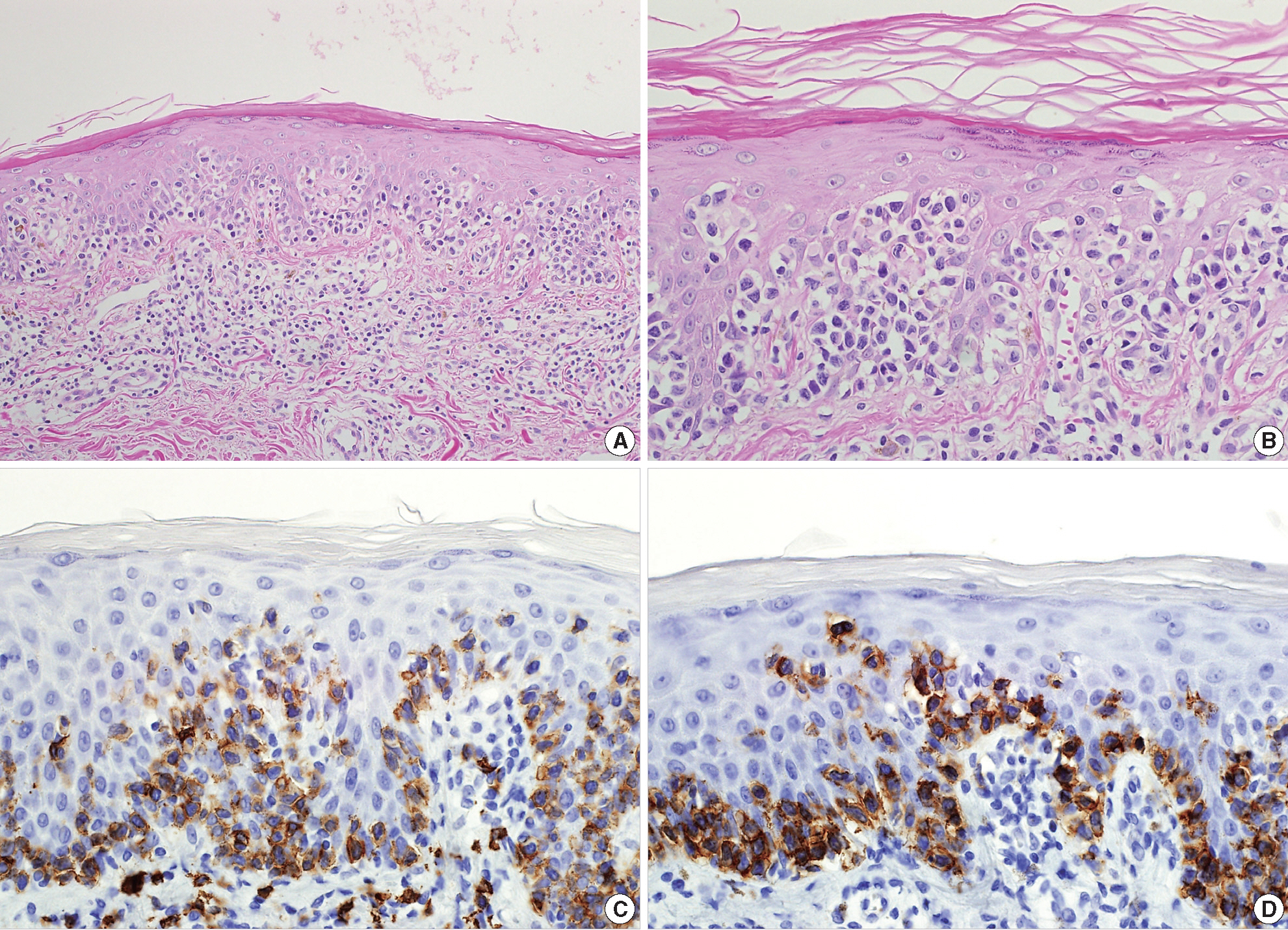
Table 1.Immunohistochemical staining results of the reported cases
| Author | CD3 | CD4 | CD8 | CD56 | Granzyme B | CD30 |
|---|---|---|---|---|---|---|
| Wain et al.[5] (case No. 1) | + | - | + | + | - | - |
| Wain et al.[5] (case No. 2) | + | - | - | + | + | - |
| Wain et al.[5] (case No. 3, poikiloderma) | + | - | + | + | + | - |
| Wain et al.[5] (case No. 3, tumor) | + | - | + | + | + | + |
| Sawada et al.[3] | + | - | + | + | - | - |
| Horst et al.[7] | + | + | +/- | + | Not performed | Not performed |
| Nikolaou et al.[2] | + | - | + | + | Not performed | - |
| Klekotka et al.[8] | + | - | - | + | Not performed | Not performed |
| Shiomi et al.[4] | + | - | + | + | + | - |
| Present case | + | - | + | + | + | - |
Table 2.Clinical characteristics of the reported case
| Author | Age (yr)/Sex | Clinical pattern | Treatment | Clinical course | EBER-1 |
|---|---|---|---|---|---|
| Wain et al.[5] (case No. 1) | 45/F | Poikiloderma | Radiotherapy and topical steroid | Limited response | Not performed |
| Wain et al.[5] (case No. 2) | 6/F | Hypo- and hyperpigmentation | Topical steroid and nUVB | Good response | Not performed |
| Wain et al.[5] (case No. 3) | 37/F | Poikiloderma, tumor | PUVA, excision | Good response | Not performed |
| Sawada et al.[3] | 68/F | Poikiloderma | nUVB, oral PUVA | Good response | Negative |
| Horst et al.[7] | 85/F | Erythroderma | Topical steroid | Good response | Not performed |
| Nikolaou et al.[2] | 43/F | Poikiloderma | PUVA | Good response | Not performed |
| Klekotka et al.[8] | 33/F | Erythroderma | Topical steroid and PUVA | Good response | Not performed |
| Shiomi et al.[4] | 20/F | Poikiloderma | Topical steroid | Good response | Negative |
| Present case | 40/M | Erythroderma | nUVB | Limited response | Negative |
- 1. Willemze R, Jaffe ES, Burg G, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005; 105: 3768-85. ArticlePubMed
- 2. Nikolaou VA, Papadavid E, Katsambas A, et al. Clinical characteristics and course of CD8+ cytotoxic variant of mycosis fungoides: a case series of seven patients. Br J Dermatol 2009; 161: 826-30. ArticlePubMed
- 3. Sawada Y, Sugita K, Kabashima R, et al. CD8+ CD56+ mycosis fungoides with an indolent clinical behaviour: case report and literature review. Acta Derm Venereol 2010; 90: 525-6. ArticlePubMed
- 4. Shiomi T, Monobe Y, Kuwabara C, Hayashi H, Yamamoto T, Sadahira Y. Poikilodermatous mycosis fungoides with a CD8+ CD56+ immunophenotype: a case report and literature review. J Cutan Pathol 2013; 40: 317-20. ArticlePubMedPDF
- 5. Wain EM, Orchard GE, Mayou S, Atherton DJ, Misch KJ, Russell-Jones R. Mycosis fungoides with a CD56+ immunophenotype. J Am Acad Dermatol 2005; 53: 158-63. ArticlePubMed
- 6. Santucci M, Pimpinelli N, Massi D, et al. Cytotoxic/natural killer cell cutaneous lymphomas. Report of EORTC Cutaneous Lymphoma Task Force Workshop. Cancer 2003; 97: 610-27. ArticlePubMedPDF
- 7. Horst BA, Kasper R, LeBoit PE. CD4+, CD56+ mycosis fungoides: case report and review of the literature. Am J Dermatopathol 2009; 31: 74-6. ArticlePubMed
- 8. Klekotka PA, Faulkner-Jones B, Heffernan MP. A case of CD56+ mycosis fungoides. Arch Dermatol 2006; 142: 1370-2. ArticlePubMed
- 9. Massone C, Crisman G, Kerl H, Cerroni L. The prognosis of early mycosis fungoides is not influenced by phenotype and T-cell clonality. Br J Dermatol 2008; 159: 881-6. ArticlePubMed
- 10. Um SH, Oh CW. CD8 expression in mycosis fungoides. Korean J Dermatol 2004; 42: 1525-30.
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Chronic Radiation Dermatitis Secondary to Narrow-Band Ultraviolet B Therapy in a Patient With Primary Cutaneous CD8+ T-Cell Lymphoma With Cytotoxic Granules
Mia P. Edelson, Jane J. Gay, Robert W. Thiel, Douglas J. Grider
The American Journal of Dermatopathology.2024; 46(5): 312. CrossRef - Null T‐cell phenotype mycosis fungoides with aberrant CD20 and CD56 expression: A diagnostic dilemma
Brenna M. Aran, Regina Burton, Whitney A. High, Alejandro A. Gru
Journal of Cutaneous Pathology.2024; 51(8): 614. CrossRef - Primary cutaneous CD8+ cytotoxic T‐cell lymphoma of the face with intraoral involvement, resulting in facial nerve palsy after chemotherapy
Daphine Caxias Travassos, Heitor Albergoni Silveira, Evânio Vilela Silva, Beatriz Zamboni Martins Panucci, Nilson Coelho da Silva Filho, Paula Verona Ragusa Silva, Andreia Bufalino, Jorge Esquiche León
Journal of Cutaneous Pathology.2022; 49(6): 560. CrossRef - A Study of Antimicrobial Activity of Herbal Extracts on Clostridium difficile
Eunhak Seong, Sookyoung Lim, Myeongjong Lee, Hojun Kim
Journal of Korean Medicine Rehabilitation.2021; 31(1): 47. CrossRef - Rare case of CD8+ CD56+ cytotoxic variant of mycosis fungoides clinically presenting with a combination of hypopigmentation and poikiloderma
Min‐Young Park, Shinwon Hwang, Jemin Kim, Abdurrahman I. Almurayshid, Sun Och Yoon, Sang Ho Oh
International Journal of Dermatology.2020;[Epub] CrossRef - Mycosis fungoides in Taiwan shows a relatively high frequency of large cell transformation and CD56 expression
Ren Ching Wang, Seiji Sakata, Bo-Jung Chen, Sheng-Tsung Chang, Pin-Pen Hsieh, Chi-Shun Yang, Satoko Baba, Kengo Takeuchi, Shih-Sung Chuang
Pathology.2018; 50(7): 718. CrossRef - CD8 + mycosis fungoides: A low-grade lymphoproliferative disorder
Maria Estela Martinez-Escala, Robert W. Kantor, Ahuva Cices, Xiaolong A. Zhou, Jason B. Kaplan, Barbara Pro, Jaehyuk Choi, Joan Guitart
Journal of the American Academy of Dermatology.2017; 77(3): 489. CrossRef - Phenotypic Variation in Different Lesions of Mycosis Fungoides Biopsied Within a Short Period of Time From the Same Patient
Natalie Kash, Cesare Massone, Regina Fink-Puches, Lorenzo Cerroni
The American Journal of Dermatopathology.2016; 38(7): 541. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Cytotoxic Variant of Mycosis Fungoides with CD8+ CD56+ Phenotype: A Case Report and Review of Literature


Fig. 1. The skin lesions in the buttocks and both thighs are erythematous to dusky brown.
Fig. 2. (A) The specimen shows a prominent band-like lymphocytic infiltration with epidermotropism. (B) The epidermotropic lymphocytes are small- to medium-sized with an irregular nuclear membrane and coarse chromatin. These cells display the cytotoxic phenotype, showing CD8 (C) and CD56 (D) immunoreactivity.
Fig. 1.
Fig. 2.
Cytotoxic Variant of Mycosis Fungoides with CD8+ CD56+ Phenotype: A Case Report and Review of Literature
| Author | CD3 | CD4 | CD8 | CD56 | Granzyme B | CD30 |
|---|---|---|---|---|---|---|
| Wain et al.[5] (case No. 1) | + | - | + | + | - | - |
| Wain et al.[5] (case No. 2) | + | - | - | + | + | - |
| Wain et al.[5] (case No. 3, poikiloderma) | + | - | + | + | + | - |
| Wain et al.[5] (case No. 3, tumor) | + | - | + | + | + | + |
| Sawada et al.[3] | + | - | + | + | - | - |
| Horst et al.[7] | + | + | +/- | + | Not performed | Not performed |
| Nikolaou et al.[2] | + | - | + | + | Not performed | - |
| Klekotka et al.[8] | + | - | - | + | Not performed | Not performed |
| Shiomi et al.[4] | + | - | + | + | + | - |
| Present case | + | - | + | + | + | - |
| Author | Age (yr)/Sex | Clinical pattern | Treatment | Clinical course | EBER-1 |
|---|---|---|---|---|---|
| Wain et al.[5] (case No. 1) | 45/F | Poikiloderma | Radiotherapy and topical steroid | Limited response | Not performed |
| Wain et al.[5] (case No. 2) | 6/F | Hypo- and hyperpigmentation | Topical steroid and nUVB | Good response | Not performed |
| Wain et al.[5] (case No. 3) | 37/F | Poikiloderma, tumor | PUVA, excision | Good response | Not performed |
| Sawada et al.[3] | 68/F | Poikiloderma | nUVB, oral PUVA | Good response | Negative |
| Horst et al.[7] | 85/F | Erythroderma | Topical steroid | Good response | Not performed |
| Nikolaou et al.[2] | 43/F | Poikiloderma | PUVA | Good response | Not performed |
| Klekotka et al.[8] | 33/F | Erythroderma | Topical steroid and PUVA | Good response | Not performed |
| Shiomi et al.[4] | 20/F | Poikiloderma | Topical steroid | Good response | Negative |
| Present case | 40/M | Erythroderma | nUVB | Limited response | Negative |
Table 1. Immunohistochemical staining results of the reported cases
Table 2. Clinical characteristics of the reported case
F, female; nUVB, narrowband ultraviolet B; PUVA, psoralen plus ultraviolet A; M, male.

 E-submission
E-submission