Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(1); 2012 > Article
-
Case Report
Urachal Mucinous Tumor of Uncertain Malignant Potential: A Case Report - Jung-Woo Choi, Ju-Han Lee, Young-Sik Kim
-
Korean Journal of Pathology 2012;46(1):83-86.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.83
Published online: February 23, 2012
Department of Pathology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- Corresponding Author: Young-Sik Kim, M.D. Department of Pathology, Korea University Ansan Hospital, Korea University College of Medicine, 516 Gojan 1-dong, Danwon-gu, Ansan 425-707, Korea. Tel: +82-31-412-5322, Fax: +82-31-412-5324, 'apysk@korea.ac.kr'
• Received: December 6, 2010 • Revised: February 11, 2011 • Accepted: February 22, 2011
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Urachal mucinous tumor of uncertain malignant potential is very rare and is characterized by a multilocular cyst showing the proliferation of atypical mucin-secreting cells without stromal invasion. As in ovarian and appendiceal borderline tumors, it represents a transitional stage of mucinous carcinogenesis in the urachus. In addition, this tumor may recur locally and develop into pseudomyxoma peritonei. Due to its scarcity and diagnostic challenges, we report a mucinous tumor of uncertain malignant potential arising in the urachus.
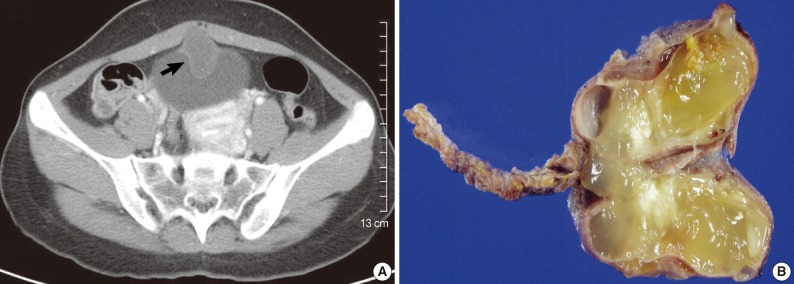
- A 29-year-old female was referred to our hospital because of a intermittent occurrence of right flank pain for 1-week. The patient had neither a family nor personal medical history. Aside from the flank pain, the patient had no other urinary symptoms such as hematuria or mucusuria. Biochemistry and hematologic results were within normal limits. A computed tomography scan of the abdomen and pelvis revealed an ovoid cystic mass located just anterior to the dome of the urinary bladder with a partially calcified wall (Fig. 1A). Radiologically, adenocarcinoma arising from urachal remnant was suggested. The patient underwent a radical excision of this mass including the attached portion of the urinary bladder and median umbilical ligament. At laparotomy, the mass originated from the dome of the urinary bladder without connection to the bladder cavity. There was no evidence of pseudomyxoma peritonei or tumors of other organs including ovary and appendix. The patient has been followed-up postoperatively with no evidence of recurrence for 11 months.
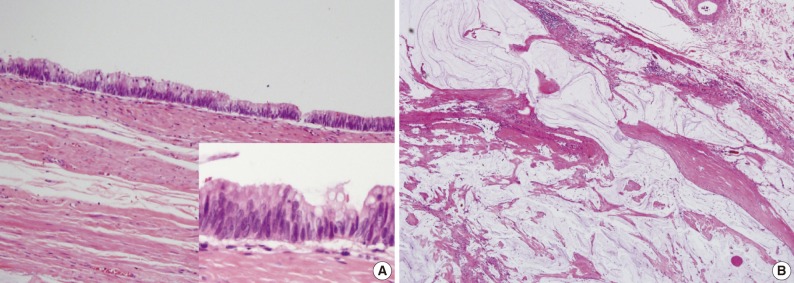
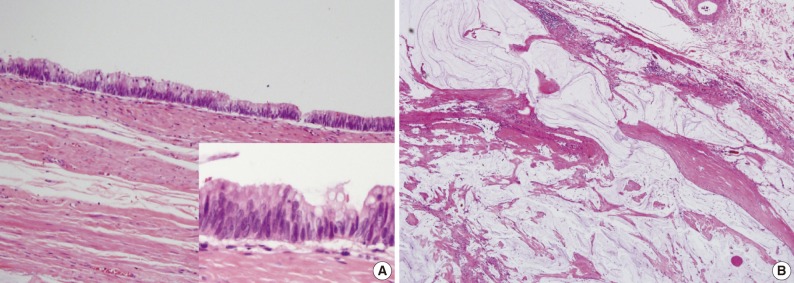
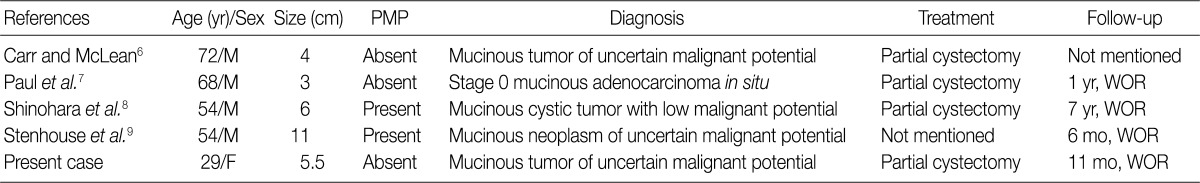
- Grossly, a multilocular cystic mass with abundant mucoid materials, measuring 5.5×3.5×1 cm, was found, which was connected to a small cuff of urinary bladder wall and a segment of median umbilical ligament (Fig. 1B). The mass did not show any papillary or solid lesions and did not communicate with the urinary bladder lumen. Histologically, the cyst was lined by a tall columnar epithelium with cellular crowding and stratification (Fig. 2A). The epithelium showed changes ranging from simple benign columnar epithelium to areas of dysplasia. Cytologically, the lining columnar cells had abundant mucin in the cytoplasm and exhibited loss of polarity, nuclear pleomorphism, and hyperchromatism in dysplastic areas, but there were no mitotic figures. No stromal invasion of the tumor cells was observed, although mucin was extravasated into the cyst wall (Fig. 2B), and foci of dystrophic calcification were present. The underlying stroma was composed of hyalinized connective tissue. On the basis of the proliferation of atypical mucinous cells and the absence of stromal invasion, the tumor was diagnosed as a mucinous tumor of uncertain malignant potential. Its association with urachal remnant and location just anterior to the dome of urinary bladder confirmed the primary urachal origin of this tumor.
CASE REPORT
- Tumors arising in the urachus are generally classified into two categories: benign and malignant. Urachal mucinous tumors with features morphologically similar to ovarian and appendiceal borderline tumors are extremely rare. Only four cases have been reported in the English literature.6-9 The authors of those cases raised the possibility that, as in ovarian and appendiceal borderline tumors, there is a transitional stage of mucinous carcinogenesis from benign to intraepithelial or infiltrative carcinoma, and those reported cases could represent the premalignant phase in this progression sequence. That hypothesis is also supported by other reports that urachal adenomas may coexist with in situ and invasive adenocarcinoma.10,11 All mucinous tumors, regardless of the source, should be accepted as having an aggressive biological potential such as local recurrence and the development of pseudomyxoma peritonei.12 Therefore, it is not surprising that a urachal adenoma with numerous mucinous implants, although histologically benign, might lead to death.13 A recent report described a complex mucinous cystadenoma of undetermined malignant potential on the basis of only extensive mucin extravasation into perivesical soft tissue, even in the absence of dysplasia in the lining of the epithelium and pseudomyxoma peritonei.5
- Characteristics of the so-called borderline urachal mucinous tumors reported thus far are listed in Table 1. All the cases described marked nuclear pleomorphism, stratification, and various degrees of mitoses in the lining epithelium but no stromal invasion. Two cases revealed the occurrence of pseudomyxoma peritonei, which required adjuvant therapy such as intraperitoneal lavage in addition to surgical removal. However, complete surgical excision was of paramount importance, as it was in the benign tumors. No recurrence was found in all of those cases, although there were limitations that the number of cases was too small to be representative and the follow-up periods were not long enough. Notably, the patient of our case was in the third decade, whereas the other reported ones were in their sixth to eighth decades.
- The differential diagnosis of urachal mucinous tumor of uncertain malignant potential includes villous adenoma, urachal mucinous adenocarcinoma, urothelial malignancy with components of adenocarcinoma, and metastatic mucinous tumor from a variety of body sites including breast, pancreas, ovary, prostate gland, and gastrointestinal tract. Villous adenoma is a benign glandular neoplasm lined by pseudostratified columnar epithelium and is characterized by papillary architecture instead of formation of a cyst containing abundant mucinous materials. Mucinous adenocarcinoma, either primary or secondary, can be easily confirmed by clinical information and the presence of stromal invasion. Criteria to classify a tumor as urachal in origin are as follows: 1) presence of urachal remnants, 2) tumor growth in the bladder wall and 3) in the dome of urinary bladder, 4) absence of dysplastic intestinal metaplasia or dysplastic mucosal change, and 5) exclusion of other primary malignancies.14,15
- We herein describe a rare case of mucinous tumor of uncertain malignant potential arising in the urachus. To the best of our knowledge, this is the first reported case in Korea and the fifth case in the English literature. We expect that this report will help to clarify the biological behavior and therapeutic implications of urachal mucinous tumors.
DISCUSSION
- 1. Taylor S, Bacchini P, Bertoni F. An isolated vertebral metastasis of urachal adenocarcinoma. Arch Pathol Lab Med 2004; 128: 1043–1045. PMID: 15338559. ArticlePubMed
- 2. Ohira S, Shiohara S, Itoh K, Ashida T, Fukushima M, Konishi I. Urachal adenocarcinoma metastatic to the ovaries: case report and literature review. Int J Gynecol Pathol 2003; 22: 189–193. PMID: 12649676. ArticlePubMed
- 3. Elliott GB, Freigang B. Observations on the nature of mucin secreting urachal cystadenoma. Ann Surg 1963; 157: 613–617. PMID: 17859733. ArticlePubMedPMC
- 4. Hull MT, Warfel KA. Urachal cystadenoma with abundant glycogen: ultrastructural study. Ultrastruct Pathol 1994; 18: 499–502. PMID: 7810000. ArticlePubMed
- 5. Schell AJ, Nickel CJ, Isotalo PA. Complex mucinous cystadenoma of undetermined malignant potential of the urachus. Can Urol Assoc J 2009; 3: E39–E41. PMID: 19672436. ArticlePubMedPMCPDF
- 6. Carr NJ, McLean AD. A mucinous tumour of the urachus: adenoma or low grade mucinous cystic tumour of uncertain malignant potential? Adv Clin Path 2001; 5: 93–97. PubMed
- 7. Paul AB, Hunt CR, Harney JM, Jenkins JP, McMahon RF. Stage 0 mucinous adenocarcinoma in situ of the urachus. J Clin Pathol 1998; 51: 483–484. PMID: 9771454. ArticlePubMedPMC
- 8. Shinohara T, Misawa K, Sano H, Okawa Y, Takada A. Pseudomyxoma peritonei due to mucinous cystadenocarcinoma in situ of the urachus presenting as an inguinal hernia. Int J Clin Oncol 2006; 11: 416–419. PMID: 17058142. ArticlePubMed
- 9. Stenhouse G, McRae D, Pollock AM. Urachal adenocarcinoma in situ with pseudomyxoma peritonei: a case report. J Clin Pathol 2003; 56: 152–153. PMID: 12560399. ArticlePubMedPMC
- 10. Cheng L, Montironi R, Bostwick DG. Villous adenoma of the urinary tract: a report of 23 cases, including 8 with coexistent adenocarcinoma. Am J Surg Pathol 1999; 23: 764–771. PMID: 10403298. ArticlePubMed
- 11. Seibel JL, Prasad S, Weiss RE, Bancila E, Epstein JI. Villous adenoma of the urinary tract: a lesion frequently associated with malignancy. Hum Pathol 2002; 33: 236–241. PMID: 11957151. ArticlePubMed
- 12. de Bree E, Witkamp A, Van De Vijver M, Zoetmulde F. Unusual origins of Pseudomyxoma peritonei. J Surg Oncol 2000; 75: 270–274. PMID: 11135270. ArticlePubMed
- 13. Eble JN, Hull MT, Rowland RG, Hostetter M. Villous adenoma of the urachus with mucusuria: a light and electron microscopic study. J Urol 1986; 135: 1240–1244. PMID: 3712579. ArticlePubMed
- 14. Abenoza P, Manivel C, Fraley EE. Primary adenocarcinoma of urinary bladder: clinicopathologic study of 16 cases. Urology 1987; 29: 9–14. PMID: 2432717. ArticlePubMed
- 15. Jones WA, Gibbons RP, Correa RJ Jr, Cummings KB, Mason JT. Primary adenocarcinoma of bladder. Urology 1980; 15: 119–122. PMID: 7355534. ArticlePubMed
References
Fig. 1(A) Computed tomography scan of the pelvis reveals an irregular cystic mass (arrow) in the dome of the urinary bladder. (B) Grossly, the multilocular cyst contains abundant mucin.
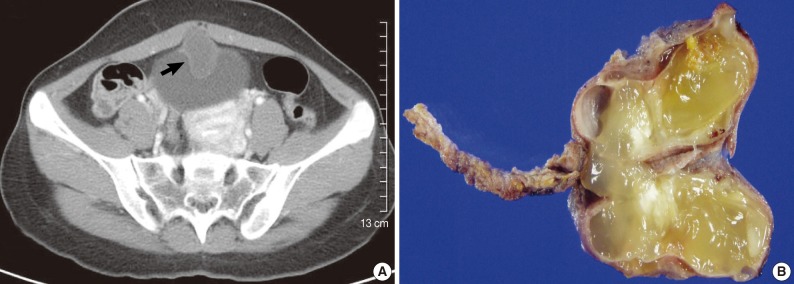
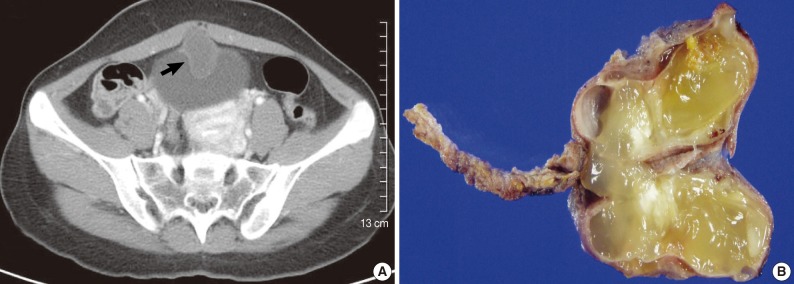
Figure & Data
References
Citations
Citations to this article as recorded by 

- Mucinous Cystadenoma of the Urachus and Review of Current Classification of Urachal Mucinous Cystic Neoplasms
Diping Wang, Norbert Sule
Archives of Pathology & Laboratory Medicine.2019; 143(2): 258. CrossRef - Urachal Mucinous Cystic Tumor of Low Malignant Potential with Concurrent Sigmoid Colon Adenocarcinoma
Kelly Brennan, Paul Johnson, Heather Curtis, Thomas Arnason
Case Reports in Gastrointestinal Medicine.2019; 2019: 1. CrossRef - Pseudomyxoma Peritonei Arising from Mucinous Cystadenoma of the Urachus with Postoperative Disease-Free Survival over 15 Years
Tomoki Kobayashi, Shinichi Mizuno, Hideki Matsuba, Min Kanamori, Toshio Tamauchi, Makoto Urano
The Japanese Journal of Gastroenterological Surgery.2019; 52(6): 307. CrossRef - Urachal borderline mucinous cystadenoma
Jingjun Wu, Ailian Liu, Anliang Chen, Pengxin Zhang
Medicine.2017; 96(47): e8740. CrossRef - Incidental Finding of a Rare Urachal Pathology: Urachal Mucinous Cystic Tumour of Low Malignant Potential
Luke L. Wang, Heath Liddell, Sharman Tan Tanny, Briony Norris, Sree Appu, David Pan
Case Reports in Urology.2016; 2016: 1. CrossRef - A Case of Borderline Mucinous Cystadenoma Thought to be of Urachal Origin
Kiichiro YAGUCHI, Yoshihito GOMYO, Hiroyasu SAITO, Tatsuo IKENO, Hiromi SAKAGUCHI, Hideo MIYAMOTO
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2014; 75(5): 1418. CrossRef - An unexpected mass of the urachus: a case report
Monica C. Pasternak, Jonathan D. Black, Natalia Buza, Masoud Azodi, Aileen Gariepy
American Journal of Obstetrics and Gynecology.2014; 211(4): e1. CrossRef

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article