Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(2); 2012 > Article
-
Case Report
Ectomesenchymal Chondromyxoid Tumor in the Anterior Tongue: Case Report of a Unique Tumor - Min Gyoung Pak, Kyung Bin Kim, Nari Shin, Woo Kyung Kim, Dong Hoon Shin, Kyung Un Choi, Mee Young Sol
-
Korean Journal of Pathology 2012;46(2):192-196.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.2.192
Published online: April 25, 2012
Department of Pathology, Pusan National University School of Medicine, Yangsan, Korea.
- Corresponding Author: Dong Hoon Shin, M.D. Department of Pathology, Pusan National University School of Medicine, 20 Geumo-ro, Yangsan 626-770, Korea. Tel: +82-51-510-8050, Fax: +82-51-510-8040, 'donghshin@chol.com'
• Received: December 1, 2010 • Revised: March 20, 2011 • Accepted: April 18, 2011
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Ectomesenchymal chondromyxoid tumor (ECMT) is a rare tumor, exclusively arising in the anterior tongue. Thirty-eight cases have been reported in the English literature. It usually presents as a sessile protrusion and shows round to spindle cells embedded in myxoid to chondroid stroma. Tumor cells are almost always positive for polyclonal glial fibrillary acidic protein (GFAP). We report our experience in the recent treatment of a case of ECMT, the third case in 3 years. The mass in the anterior tongue revealed characteristic morphologic features of ECMT and the expression of polyclonal GFAP. Although ECMT should be differentiated from other mesenchymal tumors including myoepithelioma, its clinical, morphological, and immunohistochemical features enable its diagnosis, especially when pathologists are aware of it.
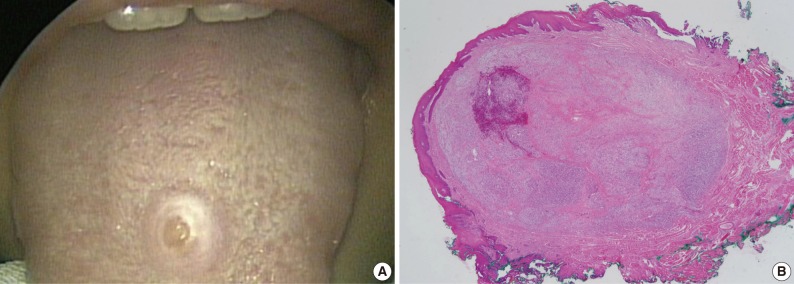
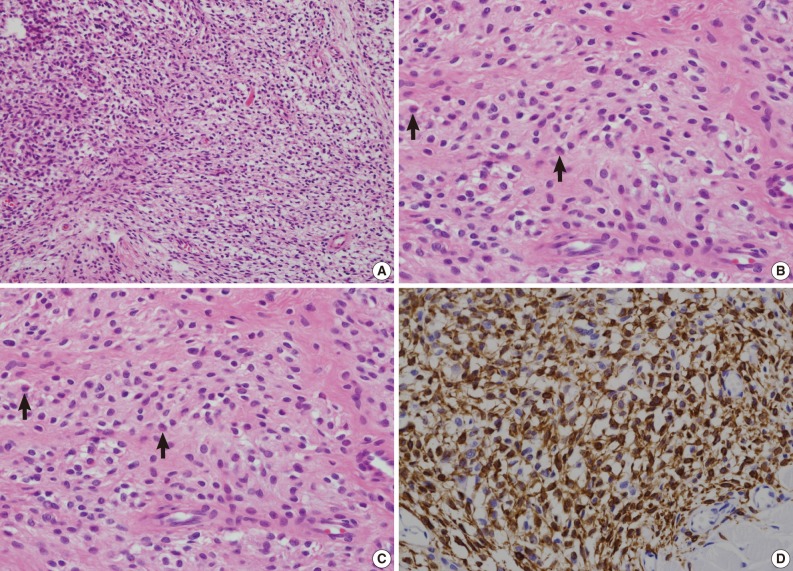
- A 16-year-old female visited the Department of Otolaryngology at Pusan National University, Yang-San Hospital, for treatment of a tongue mass. The mass was first evident 2 years earlier and had recently enlarged. The dome-shaped, 0.5 cm mass was located in the anterior right tongue (Fig. 1). The overlying mucosa was intact without ulceration. For diagnosis and treatment, an excision biopsy was performed. The tumor was located in the submucosa. On scanning power microscopy, the tumor was revealed as generally well-defined without encapsulation (Fig. 2A). Closer inspection revealed that the tumor cells were arranged in a cord, nest, or reticular pattern in focally myxoid stroma (Fig. 2B). The tumor cells were mostly fusiform or spindle shaped, with dark and occasionally cup-shaped nuclei. Significant nuclear atypia or mitosis was not observed although double nuclei were infrequently seen (Fig. 2C). The cytoplasm was scanty and amphophilic or eosinophilic. Pre-existing skeletal muscle fibers were entrapped by tumor cells. The tumor cells were positive for vimentin, and monoclonal and polyclonal glial fibrillary acidic protein (GFAP) (Fig. 2D), and were negative for pancytokeratin, smooth muscle actin (SMA), epithelial membrane antigen, CD34, calponin, S100, smooth muscle myosin heavy chain, and p63.
CASE REPORT
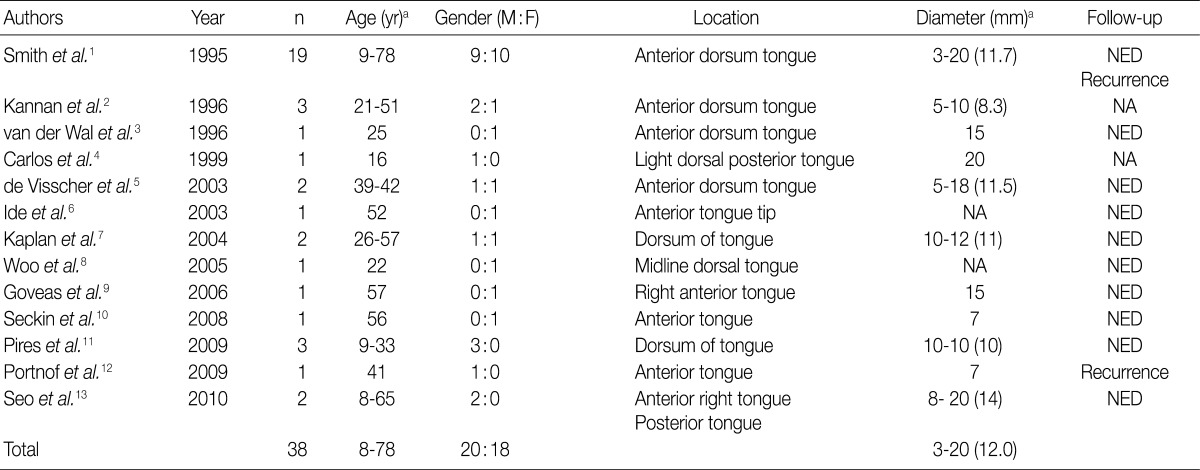
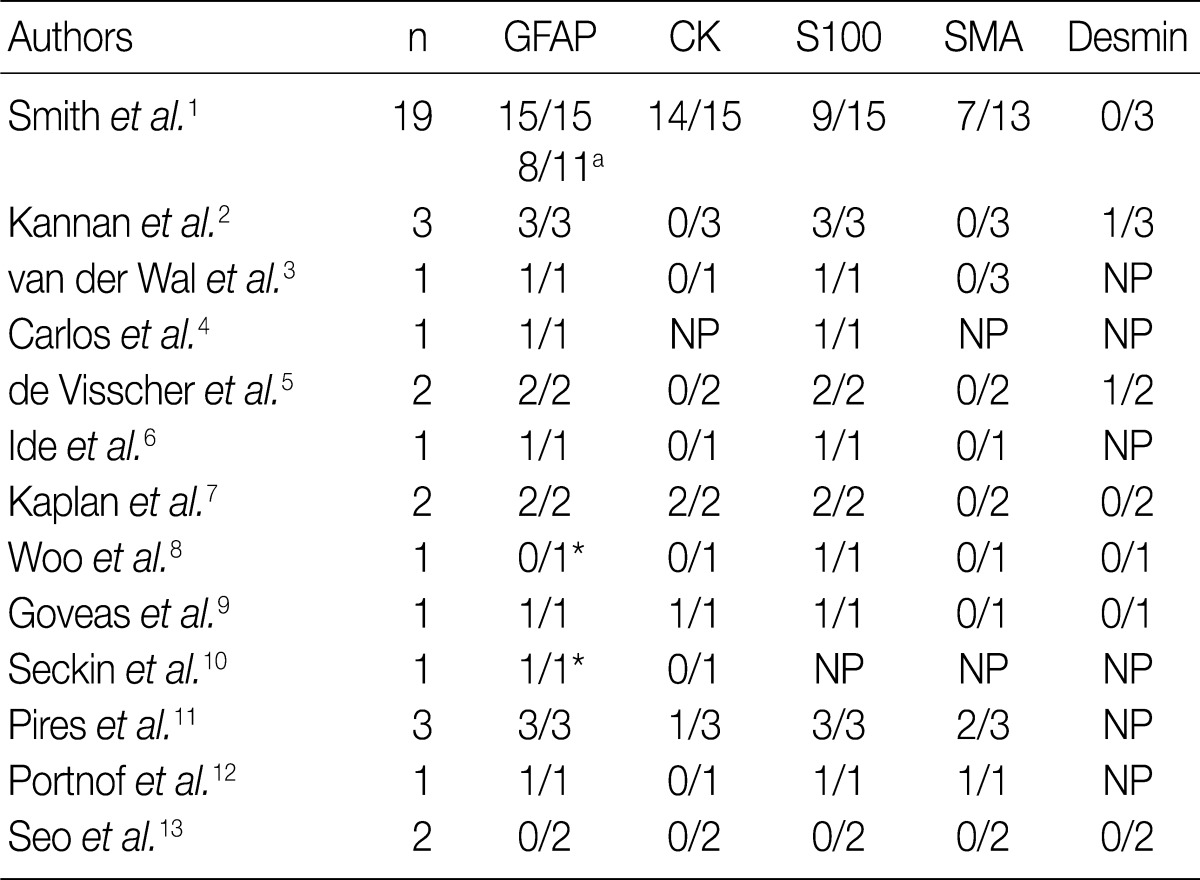
- ECMT is a rare and unique tumor, clinically and pathologically.1-14 It usually occurs almost exclusively in the anterior portion of the tongue as a dome-shaped or sessile protrusion,1-12 except for one case in the posterior tongue.13 Morphologically, these tumors also display characteristic tumor cells embedded in myxoid to chondroid stroma. The nuclei of the tumor cells are spindle to fusiform, or cup-shaped. Some double nuclei can be seen. The tumor cells are arranged in a cord, nest, reticular or whirl pattern. Although the tumor cells can grow in a focally infiltrative pattern and entrap muscle fibers, the boundary of the tumor is generally well-defined. One case showed a myxoglobulosis-like change.6 Immunohistochemically, the tumor cells are usually positive for GFAP (Table 2). Polyclonal GFAP antibody is more frequently expressed than monoclonal antibody1,14 and probing for both polyclonal and monoclonal GFAP is nearly always successful.1-14 Among 32 reported cases which tested for polyclonal GFAP, 29 cases were positive (91%). ECMT presents benign behavior. Although two cases reported recurrences,1,12 it is possible that the purported recurrence was actually an artifact of incomplete excision.
- The present case displayed typical clinical and pathologic features of ECMT, consistent with previous reports.1-13 Clinically, it occurred in the anterior tongue as a submucosal lesion. Tumor cells were fusiform to spindle shaped with occasional cup-shaped nuclei. The stroma was myxoid, although chondroid area was absent. On immunohistochemistry, pancytokeratin was negative, but both polyclonal and monoclonal GFAP were diffusely positive. Myoepithelial markers were all negative including smooth muscle myosin heavy chain, SMA, calponin, p63, and S100. The present clinical, morphological, and immunohistochemical findings were entirely consistent with a diagnosis of ECMT.
- ECMT should be differentiated from several mesenchymal tumors. Above all, myoepithelioma may be the first consideration, since its morphology is very reminiscent of ECMT in that it also exhibits spindle cells or cells with eccentric nuclei in the myxoid stroma. It has been suggested that ECMT is the same entity as myoepithelioma.8 However, the anterior portion of the tongue does not have a minor salivary gland and lacks myoepithelial cells.14 Moreover, ECMT usually lacks the expression of specific myoepithelial markers such as p63, smooth muscle myosin heavy chain, SMA, or calponin, which are generally expressed in myoepithelioma.9,11,13,15 Therefore, ECMT is considered a separate entity from myoepithelioma.14 Although the histogenesis of ECMT is not clear, an ectomesenchymal cell origin, which is derived from neural crest, is the most probable.1,14 In the same context, pleomorphic adenoma can be ruled out. Other myxoid or chondroid lesions including mucocele, myxoma, neurothekeoma, ossifying fibromyxoid tumor of the soft part, extraskeletal chondromyxoid sarcoma, and chondroid choristoma can be included among the differential diagnoses. One case to date was diagnosed as nerve sheath myxoma in the first excision12 and another as hemangioendothelioma (and revised after expert consultation).13 However, most mimicking lesions can be differentiated on the basis of morphology and immunohistochemistry, especially when pathologists are fully aware of the entity of ECMT. Mucocele displays mucin containing macrophages and inflammatory cells. Myxoma does not present chondroid stroma and its cells are spindle shaped but cellularity is scarce. Neurothekeoma displays a well-circumscribed and lobulated appearance, and is positive for S100 and negative for pancytokeratin. Ossifying fibromyxoid tumors have ossification foci that are not seen in ECMT. Extraskeletal chondromyxoid sarcoma exhibits a lobulated pattern and cells are arranged in short anastomosing cords. Chondroid choristoma does not show a spindle cell component.
- Since ECMT was first described in 1995,1 38 cases have been reported in the English literature. Two of them were reported by us13 and the present case is the third ECMT case in our institution in 3 years. This supports the speculation that this unique tumor may be more common than has been presumed. It is conceivable that other ECMT cases have been misdiagnosed as other entities, especially myoepithelioma. In conclusion, we emphasize that pathologists should be aware of ECMT when confronted by a mesenchymal lesion in the anterior tongue.
DISCUSSION
Acknowledgments
Acknowledgments
- 1. Smith BC, Ellis GL, Meis-Kindblom JM, Williams SB. Ectomesenchymal chondromyxoid tumor of the anterior tongue: nineteen cases of a new clinicopathologic entity. Am J Surg Pathol 1995; 19: 519–530. PMID: 7726361. ArticlePubMed
- 2. Kannan R, Damm DD, White DK, Marsh W, Allen CM. Ectomesenchymal chondromyxoid tumor of the anterior tongue: a report of three cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82: 417–422. PMID: 8899780. ArticlePubMed
- 3. van der Wal JE, van der Waal I. Ectomesenchymal chondromyxoid tumor of the anterior tongue: report of a case. J Oral Pathol Med 1996; 25: 456–458. PMID: 8930825. ArticlePubMed
- 4. Carlos R, Aguirre JM, Pineda V. Ectomesenchymal chondromyxoid tumor of the tongue. Med Oral 1999; 4: 361–365. PMID: 11507511. PubMed
- 5. de Visscher JG, Kibbelaar RE, van der Waal I. Ectomesenchymal chondromyxoid tumor of the anterior tongue: report of two cases. Oral Oncol 2003; 39: 83–86. PMID: 12457726. ArticlePubMed
- 6. Ide F, Mishima K, Saito I. Ectomesenchymal chondromyxoid tumor of the anterior tongue with myxoglobulosislike change. Virchows Arch 2003; 442: 302–303. PMID: 12647223. ArticlePubMedPDF
- 7. Kaplan I, Anavi Y, Calderon S. Ectomesenchymal chondromyxoid tumour of the anterior tongue. Int J Oral Maxillofac Surg 2004; 33: 404–407. PMID: 15145046. ArticlePubMed
- 8. Woo VL, Angiero F, Fantasia JE. Myoepithelioma of the tongue. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 99: 581–589. PMID: 15829881. ArticlePubMed
- 9. Goveas N, Ethunandan M, Cowlishaw D, Flood TR. Ectomesenchymal chondromyxoid tumour of the tongue: unlikely to originate from myoepithelial cells. Oral Oncol 2006; 42: 1026–1028. PMID: 17011812. ArticlePubMed
- 10. Seckin D, Demirkesen C, Gurbuz O. Ectomesenchymal chondromyxoid tumor of the anterior aspect of the tongue. J Am Acad Dermatol 2008; 59(2 Suppl 1):S23–S24. PMID: 18625372. ArticlePubMed
- 11. Pires FR, Abrahão AC, Cabral MG, et al. Clinical, histological and immunohistochemical features of ectomesenchymal chondromyxoid tumor. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 914–919. PMID: 19800267. ArticlePubMed
- 12. Portnof JE, Friedman JM, Reich R, Freedman PD, Behrman DA. Oral ectomesenchymal chondromyxoid tumor: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: e20–e24. PMID: 19716722. Article
- 13. Seo SH, Shin DH, Kang HJ, et al. Reticulated myxoid tumor of the tongue: 2 cases supporting an expanded clinical and immunophenotypic spectrum of ectomesenchymal chondromyxoid tumor of the tongue. Am J Dermatopathol 2010; 32: 660–664. PMID: 20661118. ArticlePubMed
- 14. Allen CM. The ectomesenchymal chondromyxoid tumor: a review. Oral Dis 2008; 14: 390–395. PMID: 18593455. ArticlePubMed
- 15. Cheuk W, Chan JK. In : Fletcher CD, ed. Salivary gland tumors. Diagnostic histopathology of tumors. 2007; 3rd ed. Philadelphia: Churchill Livingstone Elsevier, 239–395.
References
Fig. 1Visual appearance of the mass. (A) Photograph of the broad-based mass in the anterior tongue. (B) The cut surface of the mass is yellow white and glistening.
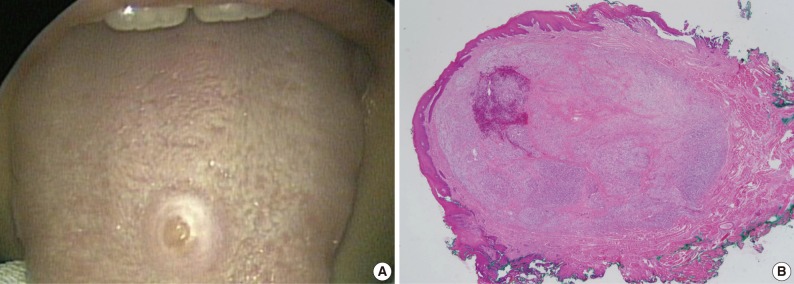
Fig. 2Microscopic appearance of the tumor. (A) On scanning power microscopy, the mass is shown to lack a capsule, but is generally well-circumscribed. (B) The tumor cells are arranged in cords, nests, or in a reticulated pattern in myxoid stroma. (C) The tumor cells possess small dark nuclei that are frequently eccentrically located or cup-shaped (arrows). Nuclear atypism is not evident. (D) The tumor cells are strongly positive for glial fibrillary acidic protein.
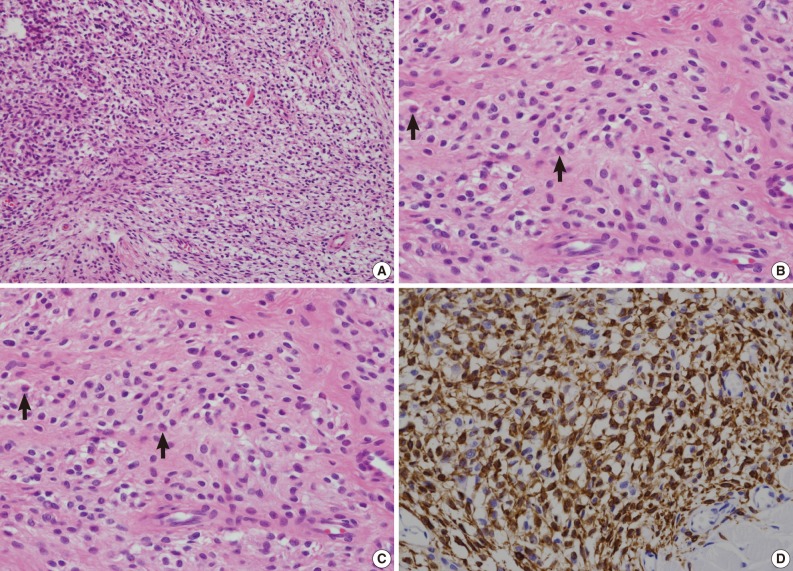
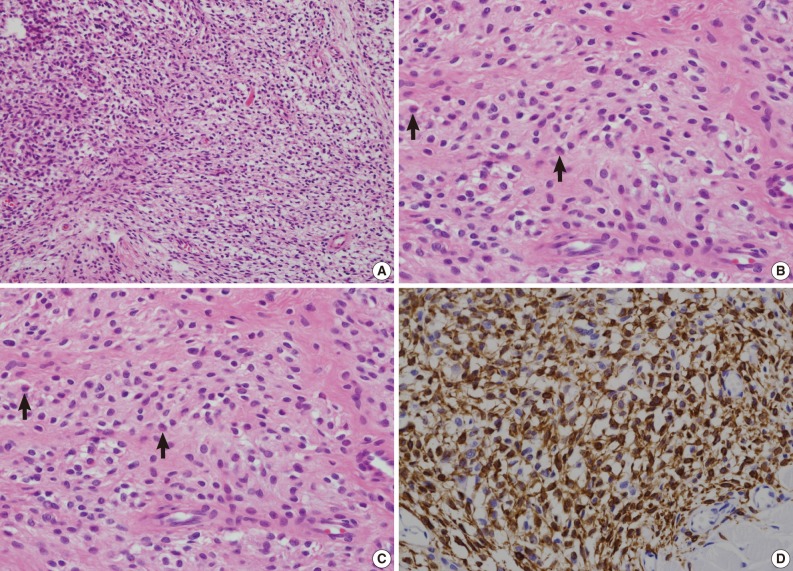
Figure & Data
References
Citations
Citations to this article as recorded by 

- Ectomesenchymal chondromyxoid tumor of the oral cavity: a report of 5 new cases with comprehensive review of the literature and clinicohistopathologic features
Molly Housley Smith, Jack Moynihan
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2023; 135(3): 410. CrossRef - Chondroid choristoma of the tongue: A rare case report
Sumaiya Nezam, Roquaiya Nishat, ShababAhmed Khan, JeevendraNath Shukla
National Journal of Maxillofacial Surgery.2022; 13(4): 121. CrossRef - Ectomesenchymal chondromyxoid tumor: a comprehensive updated review of the literature and case report
Astrid Truschnegg, Stephan Acham, Lumnije Kqiku, Norbert Jakse, Alfred Beham
International Journal of Oral Science.2018;[Epub] CrossRef - Clinical features of ectomesenchymal chondromyxoid tumors: A systematic review of the literature
Masanari G. Kato, Evren Erkul, Kendall S. Brewer, Emily E. Harruff, Shaun A. Nguyen, Terry A. Day
Oral Oncology.2017; 67: 192. CrossRef - Cyclin D1 Expression in Ectomesenchymal Chondromyxoid Tumor of the Anterior Tongue
Jan Laco, Radovan Mottl, Walter Höbling, Stephan Ihrler, Petr Grossmann, Alena Skalova, Ales Ryska
International Journal of Surgical Pathology.2016; 24(7): 586. CrossRef - Nodular lesion in the buccal mucosa
Bruna Jalfim Maraschin, Ana Carolina Amorim Pellicioli, Lélia Batista de Souza, Pantelis Varvaki Rados, Marco Antonio Trevizani Martins, Manoela Domingues Martins
The Journal of the American Dental Association.2015; 146(3): 196. CrossRef

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article