Chemotherapy-Associated Hepatopathy in Korean Colorectal Cancer Liver Metastasis Patients: Oxaliplatin-Based Chemotherapy and Sinusoidal Injury
Article information
Abstract
Background
Although chemotherapy-related hepatic injury has been reported in colorectal cancer liver metastasis (CRLM) patients, the morphologic changes caused by chemotherapeutic agents and the effect of chemotherapy on postoperative outcome remain ill-defined. A comprehensive review of the morphologic changes in the post-chemotherapy non-neoplastic liver was performed and the clinical effect of preoperative chemotherapy in CRLM patients was analyzed.
Methods
Hematoxylin-eosin, Masson's trichrome and reticulin-stained slides from non-neoplastic livers obtained from 89 CRLM patients were analyzed, and the clinicopathologic features were correlated with the status of chemotherapy exposure.
Results
Histopathologic features of sinusoidal injury (sinusoidal dilatation, centrilobular perivenular fibrosis, parenchymal extinction lesions, small vessel obliteration, and hepatocyte plate disruption) were significantly more frequent in oxaliplatin-exposed livers (p<0.05). The extent of sinusoidal dilatation was positively correlated with increasing numbers of chemotherapy cycles (p=0.022). Abnormal preoperative liver function tests were more frequently seen (p<0.05) and postoperative total bilirubin was higher in the chemotherapy group (p=0.008). Postoperative morbidity was more common in the chemotherapy group (p=0.044).
Conclusions
Sinusoidal injury is frequently seen in oxaliplatin-treated livers, and its presence, especially when extensive, should be documented in surgical pathology practice. The recognition of sinusoidal injury may provide helpful guidelines for surgeons in deciding the extent of hepatic resection.
Although the treatment of colorectal cancer liver metastasis (CRLM) primarily involves surgical resection of the metastatic tumor, the combination of surgical treatment with preoperative systemic chemotherapy has been demonstrated to increase the survival chances of CRLM patients substantially; for example, a 5-year-survival rate has been reported to be as high as 58% with preoperative treatment.1-4 Preoperative chemotherapy reduces the size of hepatic metastases, therefore resulting in the conversion of initially unresectable disease to potentially resectable disease, and hence increasing the likelihood that the metastatic tumor will be curatively resected.5-7 In addition, neoadjuvant treatment may also treat micrometastases which are not detected by imaging studies.7 The most popular regimens are those that combine fluoropyrimidines with irinotecan or oxaliplatin, including the 5-fluorouracil (5-FU) and oxaliplatin (FOLFOX) and 5-FU, oxaliplatin and irinotecan (FOLFIRI) regimens.5-11
However, while these chemotherapeutic agents have remarkable benefits in the management of these patients, they are also associated with significant adverse effects on various organs, including the liver.12-18 5-FU has been shown to be associated with hepatic steatosis,13,14,19 which is possibly mediated by excessive production of reactive oxygen species resulting in the accumulation of lipid vesicles in hepatocytes.19-21 Oxaliplatin has been associated with sinusoidal obstruction syndrome or "blue liver syndrome," possibly caused by sinusoidal endothelial cell damage.14,22 Several histopathologic features of sinusoidal injury have been described, including sinusoidal dilatation and congestion, obliteration of small vessels, disruption of hepatocyte plates, parenchymal extinction lesions (PELs), nodular regenerative hyperplasia (NRH), peliosis and veno-occlusive disease.14,16,22 Poor liver functional reserves and higher complication rates have been seen after major hepatectomy in patients with sinusoidal injury.23 In addition, an association between irinotecan treatment and steatosis or steatohepatitis has been reported.24
Although chemotherapy-related hepatotoxicity has been described, the effect of such injury on postoperative outcome in CRLM patients remains ill-defined. In this study, we performed a comprehensive review of the morphological changes in the non-neoplastic parenchyma in patients who received preoperative chemotherapy for CRLM, and correlated these findings with the clinical features.
MATERIALS AND METHODS
Patient selection and histopathologic analysis
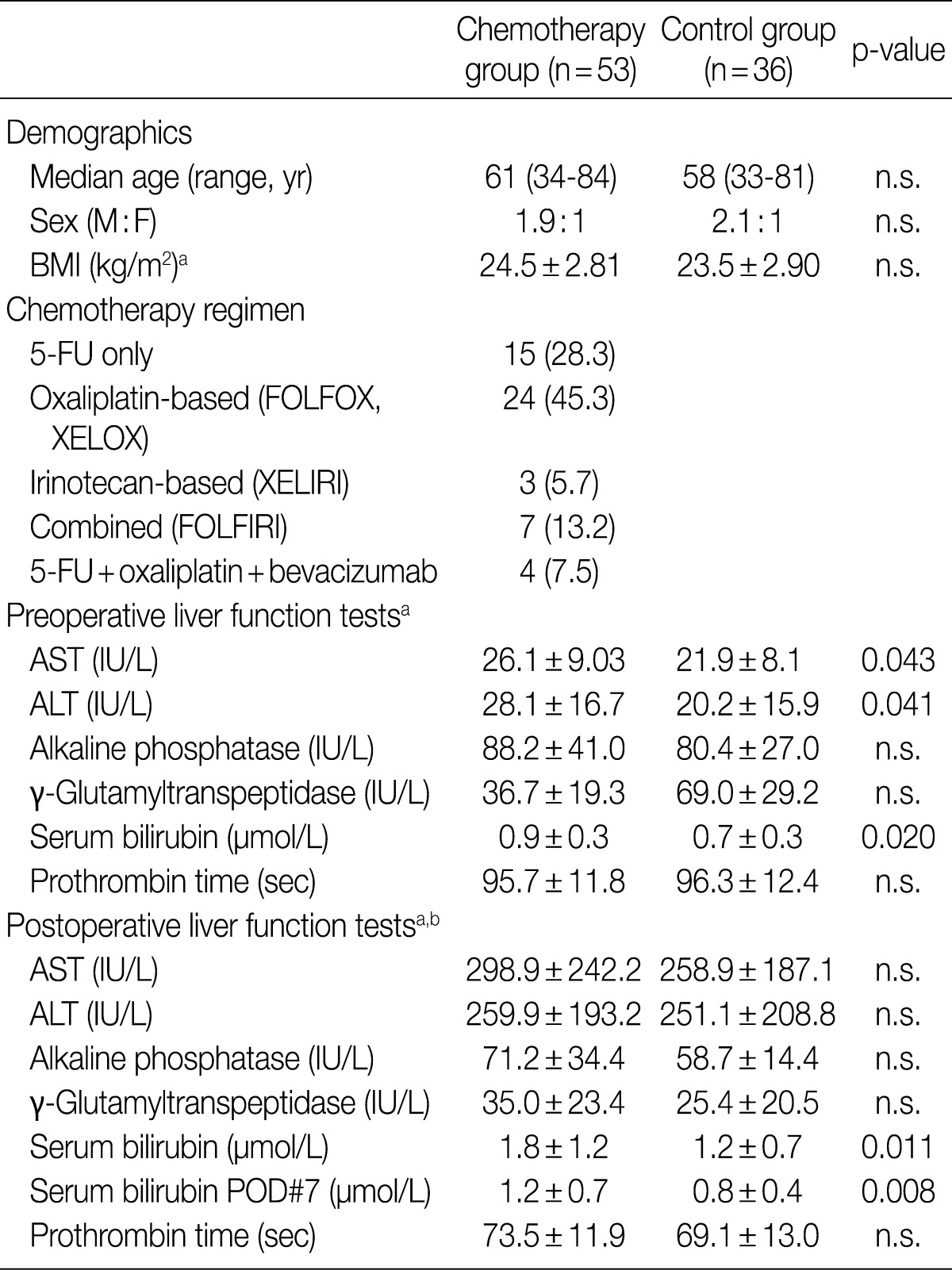
Histopathologic analysis was performed on 89 liver specimens obtained by hepatic resections between March 2003 and May 2009 for CRLMs at Seoul National University Bundang Hospital. The 89 patients fulfilled the following inclusion criteria: 1) absence of underlying liver diseases such as hepatitis B, hepatitis C or alcoholic liver disease; 2) absence of other malignant neoplasms; 3) availability of accurate clinical data (including chemotherapy regimens, number of cycles, dates of treatment); and 4) presence of sufficient non-cancerous hepatic parenchyma for histopathologic evaluation. Fifty-three (59.6%) patients received chemotherapy before hepatic resection. The chemotherapy regimens comprised oxaliplatin-based treatment (FOLFOX, XELOX) in 24 (45.3%) patients, 5-FU-only regimens (5-FU, Xeloda) in 15 (28.3%) patients, irinotecan-based regimens (XELIRI) in 3 (5.7%) patients, combined FOLFIRI in 7 (13.2%) patients and combined 5-FU, oxaliplatin and bevacizumab in 4 (7.5%) patients. Other demographic data, including patient age, sex, body mass index (kg/m2), pre- and postoperative liver function test data - serum aspartate aminotransferase (AST, IU/L), alanine aminotransferase (ALT, IU/L), alkaline phosphatase (IU/L), gamma-glutamyltranspeptidase (IU/L), total bilirubin (mg/dL) and prothrombin time (seconds) - and postoperative course were recorded. The study was approved by the Institutional Review Board of Seoul National University Bundang Hospital. The clinical characteristics of the patients are summarized in Table 1.
Routinely processed hematoxylin and eosin, Masson's trichrome and reticulin stained slides from each case were examined by 2 pathologists (S.J.N. and H.K.), who were both blind to the clinical data. In order to exclude the effects of adjacent space-occupying lesions, cauterization artifacts or subcapsular fibrosis, the histologic features of the non-tumorous hepatic parenchyma, were assessed at a minimum of 1 cm from the tumor, surgical resection margin and the Glisson's capsule.
Sinusoidal injury was determined as the presence or absence of diffuse sinusoidal dilatation, small vessel obliteration, centrilobular vein fibrosis, hepatocyte plate disruption, PELs, NRH, peliosis and veno-occlusive disease. Sinusoidal dilatation was graded as follows: 0, absent; 1, mild (centrilobular involvement limited to 1/3 of the lobular area); 2, moderate (centrilobular involvement extending to 2/3 of the lobular area); and 3, severe (complete lobular involvement). PELs were defined as the approximation of hepatic vein remnants and portal structures due to the loss of intervening hepatocytes. The degrees of macrovesicular and microvesicular steatosis were each graded from 0 to 3: grade 0, <5%; 1, mild (<33%); 2, moderate (≥33% and <66%); and 3, severe (≥66%). Lobular lymphocytic inflammation was also graded from 0 to 3: grade 0, no inflammatory foci; 1, <2 foci per 200× field; 2, 2-4 foci per 200× field; and 3, >4 foci per 200× field. In order to exclude the effect of surgical hepatitis, neutrophilic infiltration was not analyzed. The presence of hepatocellular ballooning, cholestasis or ductular reaction was analyzed. In addition to centrilobular vein fibrosis, the extent of fibrosis was also recorded as follows: portal fibrosis, periportal fibrosis, septal (bridging) fibrosis and cirrhosis.
Statistical analysis
All statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). Categorical data were analyzed using the chi-square test and Mann-Whitney U test, as deemed appropriate. Metric and ordinal values were analyzed using the Student's t-test where applicable. Correlations between variables were assessed using the Spearman's rank correlation test. Results were considered statistically significant when p<0.05.
RESULTS
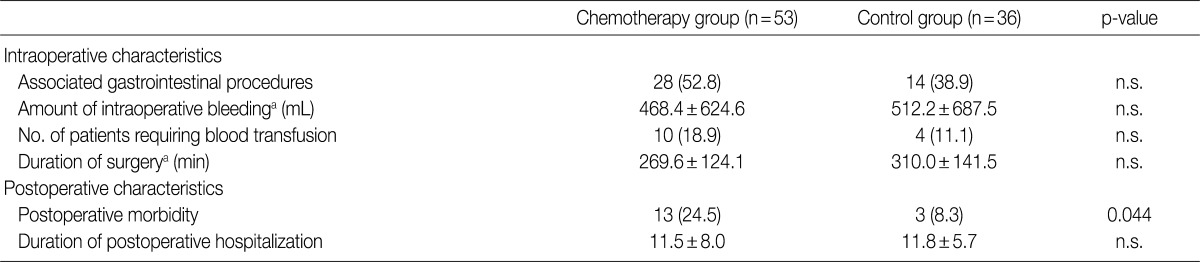
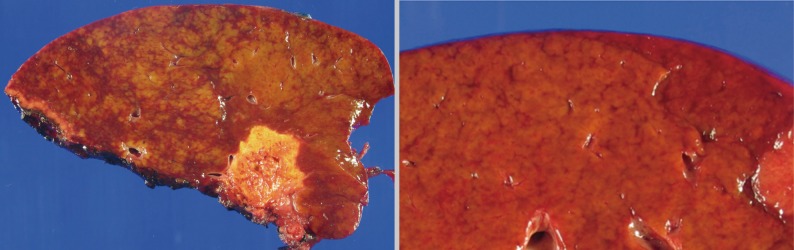
Pathologic features of chemotherapy-associated hepatopathy
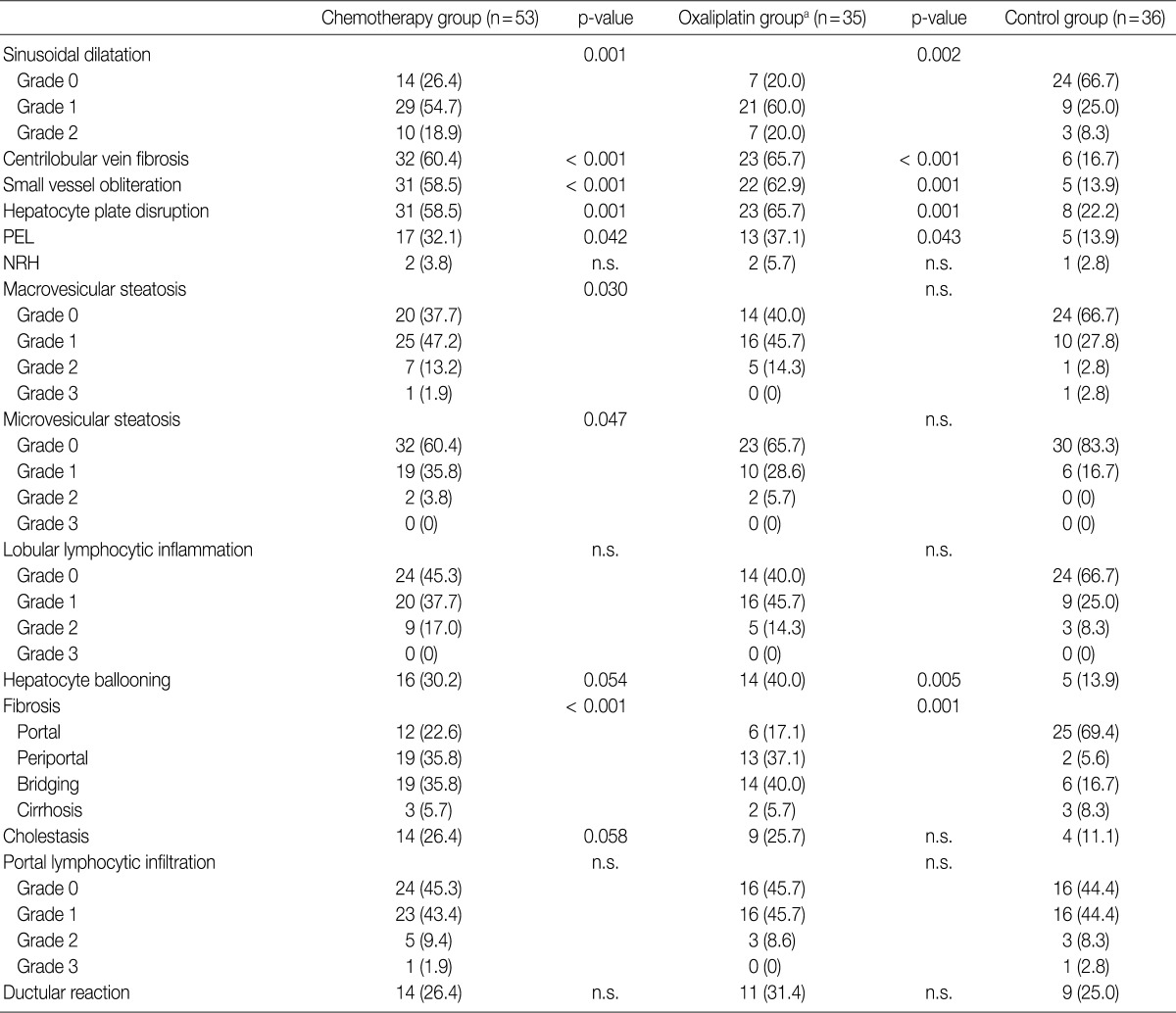
The histopathologic analysis results are summarized in Table 2 and Figs. 1 and 2. Sinusoidal dilatation (p=0.001), centrilobular perivenular fibrosis (p<0.001), small vessel obliteration (p<0.001) and hepatocyte plate disruption (p=0.001) were frequent findings in livers with preoperative chemotherapy. PELs were also more frequent in the chemotherapy group compared to the non-chemotherapy group (p=0.042). These features of sinusoidal injury were sometimes recognizable even by macroscopic examination; areas of marked congestion and parenchymal extinction alternated with relatively normal hepatic lobules, creating a diffusely nodular appearance (Fig. 1). The sinusoidal dilatation score was significantly higher with increasing numbers of chemotherapy cycles (p=0.022).
Histopathologic features of the non-neoplastic liver according to the use of preoperative chemotherapy
Gross findings. Areas of marked congestion and parenchymal extinction alternating with relatively normal hepatic lobules produce a mottled appearance.
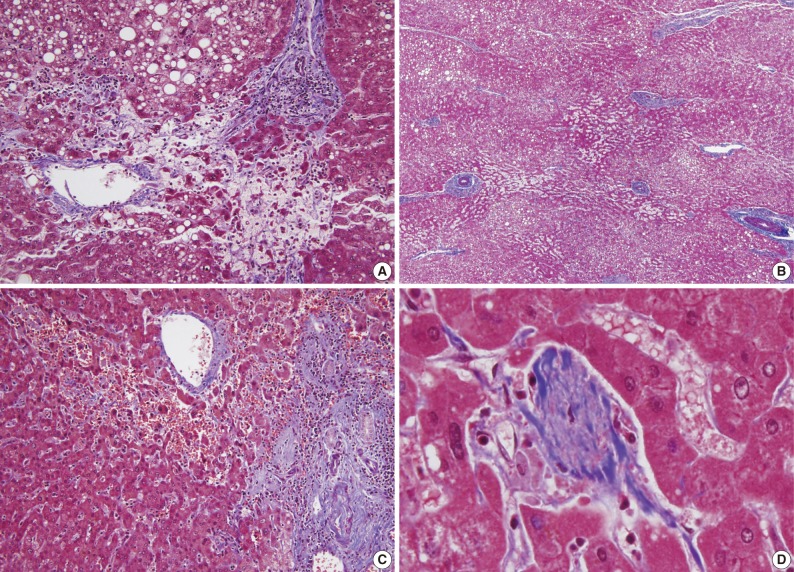
Microscopic findings. A parenchymal extinction lesion is seen, defined as the approximation of portal tract and hepatic vein due to the loss of intervening hepatocytes (A). The hepatocyte plates are disrupted (A, lower half). Macrovesicular and microvesicular steatosis is also seen (A, upper half). Sinusoidal dilatation is seen in the centrilobular area (B), and is accompanied by erythrocyte extravasation and congestion (C). Obliteration of a terminal hepatic venule is seen (D) (A-D, Masson's trichrome).
Significant macrovesicular steatosis (grades 2 and 3) was seen in 8 (15.1%) out of 53 chemotherapy group patients and in 2 (5.6%) out of 36 non-chemotherapy group patients (p=0.030). Significant microvesicular steatosis was seen in only 2 patients, both of whom received preoperative chemotherapy. The extent of fibrosis was significant in livers exposed to previous chemotherapy compared to those of the non-chemotherapy group (p<0.001); periportal and bridging fibrosis was significantly more frequent in livers with preoperative cytotoxic treatment.
Intraoperative liver biopsy for frozen section evaluation was performed for two cases prior to resection, due to the suspicion of marked sinusoidal injury. Sinusoidal dilatation with hepatocyte plate disruption and hepatocellular atrophy was recognized on the frozen section slide (Fig. 3).

Intraoperative frozen section slide demonstrates centrilobular sinusoidal dilatation and congestion with atrophy of hepatocytes, suggestive of sinusoidal damage. The extent of hepatic resection was subsequently reduced in this patient, and a second resection for another metastatic tumor was performed one month later.
Effect of oxaliplatin-based chemotherapy
In order to evaluate the effects of oxaliplatin-containing regimens (FOLFOX, XELOX, FOLFIRI and oxaliplatin+bevacizumab) on the liver, the histopathologic features of the oxaliplatin group (n=35) were analyzed separately. Sinusoidal dilatation (p=0.002), centrilobular perivenular fibrosis (p<0.001), small vessel obliteration (p=0.001), hepatocyte plate disruption (p=0.001) and PELs (p=0.043) were significantly more frequent in oxaliplatin-treated livers compared to the control population. In addition, hepatocyte ballooning was frequently seen in livers subjected to oxaliplatin-based chemotherapy (40.0%) in contrast to the control group (13.9%) (p=0.005). Periportal and bridging fibrosis was more frequent in oxaliplatin-exposed livers compared to the control group (p=0.001).
Lobular inflammation was also more frequent in the oxaliplatin-treated group (60.0%) compared to the control group (33.3%); however, the differences were not statistically significant.
Effects of other chemotherapeutic agents
When the histopathologic features were analyzed for cytotoxic drugs other than oxaliplatin (5-FU, Xeloda, irinotecan and bevacizumab), no statistically significant relationships were found.
Preoperative chemotherapy and patient outcome
Preoperative and postoperative liver function tests were evaluated in the chemotherapy group. Statistically significant differences between the chemotherapy and non-chemotherapy groups were found for preoperative serum AST (p=0.047), ALT (p=0.047) and total bilirubin levels (p=0.012). Interestingly, total bilirubin levels were significantly higher in the preoperative chemotherapy group in the immediate postoperative period (p=0.011) and while the levels decreased to normal range in the non-chemotherapy group after 7 days postoperatively, the total bilirubins still remained elevated after 7 days (p=0.008).
There was no significant difference in the intraoperative course (intraoperative bleeding, transfusion requirements, duration of surgery) between the chemotherapy and non-chemotherapy groups. However, postoperative morbidity was more frequent in the chemotherapy group (13/53, 24.5%) compared to the non-chemotherapy group (3/37, 8.1%), and included wound infection/dehiscence, fluid collection, ileus and bleeding (Table 3).
DISCUSSION
Combined fluoropyrimidines (5-FU, capecitabine) with irinotecan or oxaliplatin (FOLFOX, FOLFIRI, XELOX, XELIRI) regimens are frequently being used as first-line treatments for CRLM. However, the cytotoxic effects of these regimens do not come without complications: various types of chemotherapy-associated hepatopathy have been reported. In our study, non-neoplastic livers exposed to cytotoxic agents showed significantly more frequent sinusoidal dilatation, centrilobular venular fibrosis, PELs, hepatocyte plate disruption, small vessel obliteration, steatosis, and periportal/bridging fibrosis compared to the control group. When the chemotherapy group exposed to oxaliplatin were analyzed separately, features of sinusoidal injury (sinusoidal dilatation, centrilobular vein fibrosis, small vessel obliteration, hepatocyte plate disruption, and PELs) were still significantly more frequent compared to the control population, and in addition, hepatocellular ballooning degeneration and periportal or bridging fibrosis were frequently noted. Steatosis, either macrovesicular or microvesicular, was not a significant feature of oxaliplatin-associated hepatic injury, although it was significantly more frequent in the chemotherapy group as a whole. A high proportion of the chemotherapy group in this study (35/53, 66.0%) was subjected to oxaliplatin-containing regimens, suggesting that the strong association between oxaliplatin and sinusoidal injury may have affected the data of the chemotherapy group as a whole. On the other hand, it is also possible that sinusoidal injury may also occur due to cytotoxic drugs other than oxaliplatin, such as 5-FU, irinotecan and bevacizumab. However, no statistically significant relationships between the histopathologic features and the administration status of the latter drugs were found in this study when analyzed individually, possibly due to the small number of cases.
The pathogenesis of sinusoidal injury associated with oxaliplatin-based chemotherapy is still obscure; however, it has been suggested that the initial toxic injury to the sinusoidal endothelial cells by the chemotherapeutic drug may cause sinusoidal wall disruption, activation of hepatic stellate cells and sinusoidal matrix deposition.22 The sinusoids become markedly dilated and red blood cells extravasate into the Disse's spaces through the discontinuities in the endothelial lining.
In general, regions of sinusoidal injury are irregularly distributed within the hepatic parenchyme. However, there are cases in which the injury is more extensive with diffuse hemorrhagic foci and parenchymal nodularities, and therefore are recognizable as "abnormal" on gross examination. Indeed, surgeons do report gross abnormalities intraoperatively and sometimes request frozen section examinations of the non-neoplastic livers. The extent of surgery may ultimately be reduced, for example, from a lobectomy to a more limited tumorectomy, depending on the status of the non-tumorous liver. In addition, a novel concept of two-stage hepatectomy for multiple bilobar hepatic metastases has recently been introduced with the hope of minimizing the risk of postoperative liver failure.25,26 The idea behind this procedure is that the interval between the first and second hepatic resections provides time for compensatory regeneration of the remnant liver after initial resection, and therefore allowing a safer second curative resection without the risk of liver failure. This procedure may be applied to instances where the liver demonstrates features of marked sinusoidal injury during surgery, and two of the patients in this study actually benefited from two-stage hepatectomy.
The impact of preoperative chemotherapy on postoperative outcome is still controversial. The administration of neoadjuvant chemotherapy has generally not been associated with postoperative mortality, but increased morbidity has been described in a few recent studies.13,23,27 For example, increased postoperative morbidity and length of hospital stay have been demonstrated in patients with sinusoidal injury,23 and higher fibrosis stages have been associated with increased transfusion requirements during operation.13 In addition, a higher morbidity rate, including hepatic failure, pleural effusion, subphrenic abscess and phlebothrombosis, was demonstrated in the chemotherapy group in another study by Karoui et al.,27 and the postoperative morbidity was correlated with the number of chemotherapy cycles. On the other hand, no significant difference in morbidity was reported in another large series of patients.28 In our study, preoperative chemotherapy was associated with increased postoperative complications compared to the control group, and these patients demonstrated increased serum bilirubin levels which remained significantly elevated compared to the control group at postoperative days 1 and 7, similarly to the results in a previous report.23 Thus, it could be suggested that the preoperative treatment had toxic effects on the liver parenchyma, resulting in the derangement of liver function. Interestingly, the degree of sinusoidal dilatation was positively correlated with the number of preoperative chemotherapy cycles, also implying that the damage caused by the chemotherapeutic drugs may be time- and dose-dependent, as previously suggested.29
This study has a few limitations, the most important being that the patient population is heterogeneous and has been subjected to a variety of regimens and different numbers of cycles. In addition, a wide range of time intervals between the most recent chemotherapy cycle and the time of surgery may also affect the data. Nevertheless, we have demonstrated that there is a strong association between oxaliplatin-based treatment - regardless of whether oxaliplatin was combined with 5-FU, irinotecan or other drugs - and sinusoidal injury, that sinusoidal dilatation was more diffuse in patients with increased number of chemotherapy cycles and that preoperative chemotherapy is associated with postoperative morbidity and abnormal liver function tests, suggestive of hepatic functional derangement.
In summary, it is important that the presence of features of marked sinusoidal injury is documented in addition to the description of the tumor, as these features are related to clinical parameters such as high bilirubin levels and more frequent postoperative complications. Features of sinusoidal injury, especially when extensive, are not difficult to recognize microscopically, and the documentation of these features in preoperative or intraoperative biopsies may also provide helpful guidelines for surgeons in deciding the extent of resection.
Notes
No potential conflict of interest relevant to this article was reported.