Proposal for a Standardized Pathology Report of Gastroenteropancreatic Neuroendocrine Tumors: Prognostic Significance of Pathological Parameters
Article information
Abstract
Background
There is confusion in the diagnosis and biological behaviors of gastroenteropancreatic neuroendocrine tumors (GEP-NETs), because of independently proposed nomenclatures and classifications. A standardized form of pathology report is required for the proper management of patients.
Methods
We discussed the proper pathological evaluation of GEP-NET at the consensus conference of the subcommittee meeting for the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists. We then verified the prognostic significance of pathological parameters from our previous nationwide collection of pathological data from 28 hospitals in Korea to determine the essential data set for a pathology report.
Results
Histological classification, grading (mitosis and/or Ki-67 labeling index), T staging (extent, size), lymph node metastasis, and lymphovascular and perineural invasion were significant prognostic factors and essential for the pathology report of GEP-NET, while immunostaining such as synaptophysin and chromogranin may be optional. Furthermore, the staging system, either that of the 2010 American Joint Cancer Committee (AJCC) or the European Neuroendocrine Tumor Society (ENETS), should be specified, especially for pancreatic neuroendocrine neoplasms.
Conclusions
A standardized pathology report is crucial for the proper management and prediction of prognosis of patients with GEP-NET.
We have previously reported that the incidence of gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) has been on the rise in Korea during the last decade.1 According to the 2000 World Health Organization (WHO) classification, the most significant increase was found in well-differentiated endocrine tumors (WDETs),2 especially those in the rectum. Although the incidence of well-differentiated endocrine carcinoma (WDEC) and poorly differentiated endocrine carcinoma (PDEC) have also increased since 2003, they are still lower than the prevalence of other malignancies in the digestive tract. We additionally found that there was confusion in using diagnostic terminology for tumors due to changes in the classification system over several decades.
Cells of the diffuse endocrine system are defined as neuroendocrine cells because of their features, such as two regulatory pathways of secretion and pertinent antigens, which are similar to those of neurons.3 Neoplastic lesions showing prominent explicit neuroendocrine features of the diffuse endocrine system are thus called neuroendocrine tumors (NETs).
The first WHO classification system of GEP-NENs, proposed in 1980, used the term "carcinoid" to describe all well-differentiated gastrointestinal NETs regardless of their biologic behavior and pathological characteristics.4 Later, in 2000 and 2004, WHO reclassified NETs into well-differentiated tumors and poorly differentiated carcinomas.2,5 The well-differentiated tumors were subdivided into benign, uncertain malignancy, or carcinoma depending on their pathologic features. They also recommended that the term "carcinoid tumor" be used only for benign well-differentiated tumors. Because the term "carcinoid tumor" does not convey the malignant potential of tumors and can be confused with "carcinoid syndrome," the term "neuroendocrine neoplasm" has instead been accepted for general nomenclature, with further recommendation of reserving the former term for benign well-differentiated tumors. The latest WHO update in 2010 refers to all neuroendocrine neoplasms as being potentially malignant and divides them into NET G1, NET G2, and neuroendocrine carcinoma (NEC) based on cell proliferation rate, regardless of tumor location, size, or extent.6
However, gastroenteropancreatic neuroendocrine tumors (GEP-NETs) are well known to have diverse biological behavior according to the organ of origin and pathological features.7 The 2010 WHO classification system still does not include enough information about the tumor to predict prognosis and determine treatment modality. The 10-year survival rate has been reported to be 92.89% for well-differentiated neuroendocrine tumor (WDNET) as defined by 2000 WHO classification and 93.5% in NET G1 as defined by 2010 WHO classification,1 highlighting the uncertain malignant potential of the NETs despite their small size and confinement to the mucosa and submucosa.
The evaluation of pathological features related to prognosis is therefore essential for the proper management of patients. The American Joint Committee on Cancer (AJCC)8 and the European Neuroendocrine Tumor Society (ENETS)9 proposed a staging system for NETs in each organ system based on tumor size and extension. Immunohistochemical staining is also mandatory for the diagnosis of GEP-NETs, especially when using Ki-67 for grading.10 Other pathological features related to the prognosis of GEP-NET have been proposed in several guidelines.3,11-21
From a review of the published literature of guidelines for pathological diagnosis, the subcommittee of GEP-NET in the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists selected the essential data set for a standardized pathology report of GEP-NET and analyzed the prognostic significance of parameters using nationwide Korean data from our previous study.1 In the present study, we describe the prognostic significance with practical issues of pathological factors and propose a standardized form for the pathology report of GEP-NENs.
MATERIALS AND METHODS
Materials
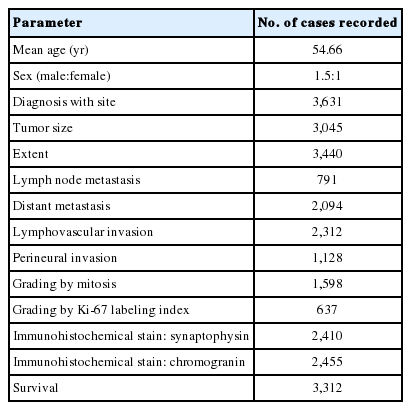
The consensus conference on GEP-NENs was held by subcommittee members of the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists on June 26, 2010 to determine the essential data set for a pathology report. We reviewed the literature of classification systems proposed by WHO,2,6 the ENETS,12 and the North American Neuroendocrine Tumor Society (NANETS).13,14,20 The pathological parameters which have been described as prognostic factors for GEP-NENs in the literature were selected through committee discussion. We statistically analyzed the prognostic significance of the pathological parameters using data that were collected during our previous nationwide study.1 The available information collected from our previous nationwide study is briefly summarized in Table 1.
Statistical analysis
To estimate the association between eligible variables and mean survival time, the Kaplan-Meier test was applied together with the log-rank test to compare various groups. The Spearman correlation coefficient was used for the correlation between parameters. For the comparison between the pathological diagnoses according to the 2000 and 2010 WHO classifications, the McNemar test was performed. Multivariate analysis (e.g., Cox proportional hazard regression) was also performed to evaluate the relative risk of parameters. SAS ver 9.2 (SAS Inc., Cary, NC, USA) was used for statistical analyses. A p<0.05 was considered statistically significant.
RESULTS
Histological diagnosis
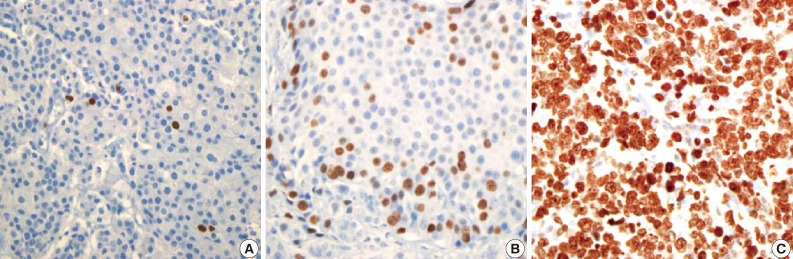
Distinction between well-differentiated and poorly-differentiated tumors based on histology alone is feasible, even on a smaller-sized biopsy specimen. On the contrary, it is sometimes difficult to strictly define and classify NENs into a specific subgroup based only on histologic evaluation of especially small biopsies in the absence of other diagnostic tools such as immunohistochemistry. Our data reveal that patients who have well-differentiated tumors (WDET or WDEC) have a significantly better survival rate than those who have poorly-differentiated tumors (PDEC, MEC, or MEEC) (p<0.0001) (Fig. 1). Thus, we assume that the broad categorization of NENs into well-differentiated and poorly-differentiated tumors is helpful for the prognostic stratification of patients at the time of diagnosis in cases where specific subgrouping is difficult.
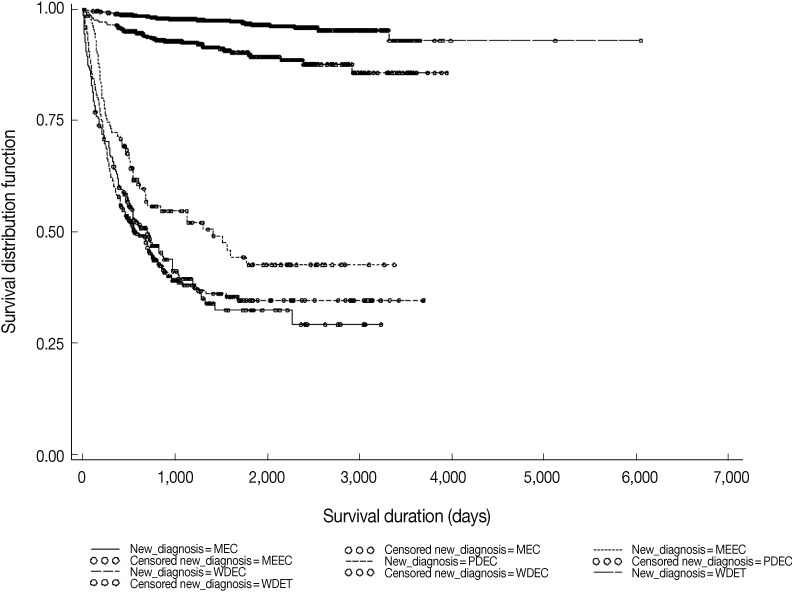
Kaplan-Meier survival curves show prognostic difference between the pathological diagnosis by 2000 World Health Organization (WHO) classification (p<0.0001). MEC, metastatic endocrine carcinoma; MEEC, mixed exocrine-endocrine carcinoma; PDEC, poorly-differentiated endocrine carcinoma/small cell carcinoma; WDEC, well-differentiated endocrine carcinoma; WDET, well-differentiated endocrine tumor.
Grading
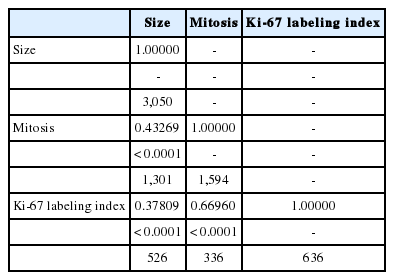
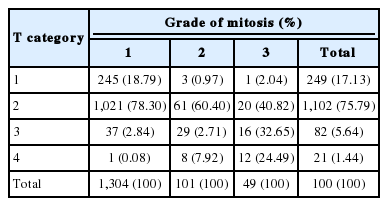
The grade of NENs indicates the proliferative activity of tumors and is assessed by evaluating mitotic rate and/or Ki-67 labeling index. The proliferation grading, proposed by ENETS,22 is internationally accepted as an essential component of a standard pathology report. Mitosis should be counted in at least a 2 mm2 area or in 50 high-power fields (HPFs), and it is presented as number/10HPFs. For the Ki-67 labeling index using MIB1 antibody, 500-2,000 tumor cells in a hot spot area should be counted. Based on our data, mitotic count and Ki-67 labeling index serve as significant prognostic factors (p<0.0001) (Fig. 2). In Cox regression analysis, NET G2 and G3 showed significantly worse prognosis than G1 based on mitotic count (G2: hazard ratio [HR], 9.595; 95% confidence interval [CI], 5.461 to 16.853; p<0.0001) and G3: HR, 28.742; 95% CI, 16.707 to 49.447; p<0.0001). However, based on evaluation of Ki-67 labeling index, only G3 showed a significantly worse prognosis (G2: HR, 1.966; 95% CI, 0.508 to 7.607; p=0.3274 and G3: HR, 18.249; 95% CI, 6.568 to 39.648; p<0.0001). This result demonstrates the significance of mitotic count in risk stratification of patients with NET G2. Additionally, the data reveal that there is significant correlation among tumor size, mitotic count, and Ki-67 labeling index. The larger tumor size was associated with elevated mitotic count and higher Ki-67 labeling index (Table 2). The distribution of tumor extent (T category) in each grade is presented in Table 3. Most T1 tumors were G1, based on mitotic count (98.4%). However, no significant association between T category and mitotic count was found.
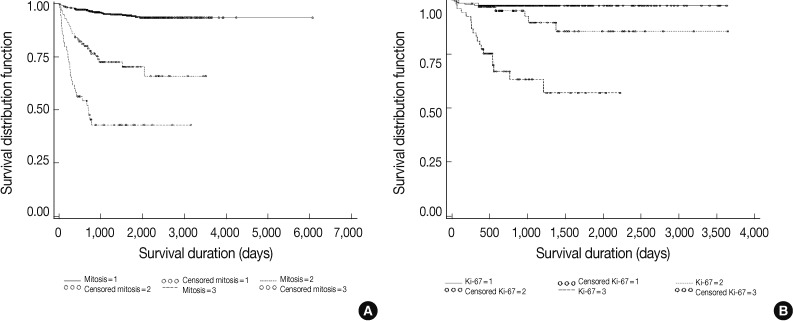
Kaplan-Meier survival curves show prognostic significance of grades based on mitosis (A) and Ki-67 labeling index (B) by 2010 World Health Organization (WHO) classification in all gastroenteropancreatic neuroendocrine neoplasms (p<0.0001). 1, G1; 2, G2; 3, G3.
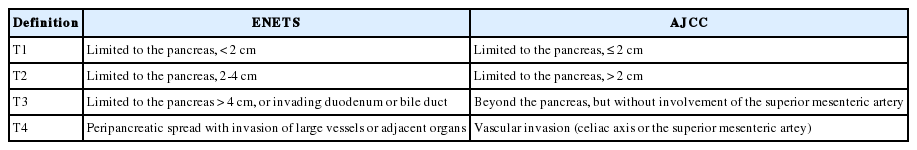
Staging: comparison of AJCC and ENETS systems
To evaluate the significance of tumor size in determining prognosis in patients, we divided tumors into four groups according to tumor size (categorized as 1 cm and then every 0.5 cm). Risk of death was found to be significantly increased in the group with tumors larger than 1.5 cm in size and stage higher than T3 (p<0.0001) (Fig. 3).
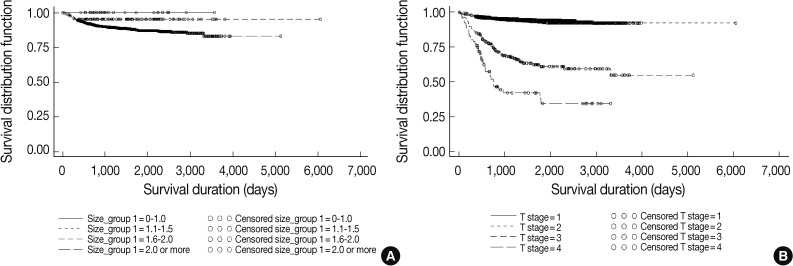
Kaplan-Meier survival curves according to tumor size in cm (A) and T category by 2010 American Joint Cancer Committee (AJCC) TNM staging (B) show a significantly increased risk of death in the group with tumors larger than 1.5 cm in size and stage higher than T3 (p<0.0001).
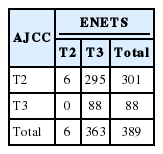
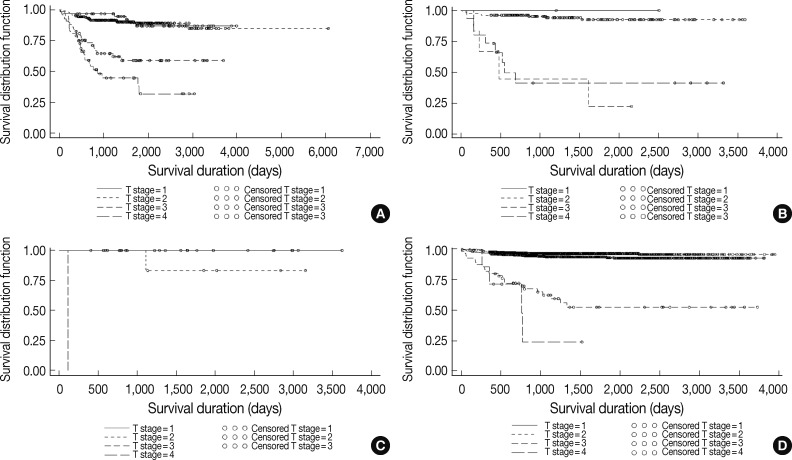
As in other malignant tumors, staging plays an important and integral role for the prognostic stratification of patients with GEP-NET. The AJCC8 and the ENETS3,7,22 proposed site-specific TNM classifications for gastrointestinal NETs. The criteria for T category of NETs in each site, which include tumor extent and size, are different from those of adenocarcinomas. Contrary to that, staging for NECs and NETs of the pancreas are the same as for adenocarcinomas. Therefore, the correct histologic classification and measurement of tumor size are fundamental for staging of GEP-NET. The comparative analysis between AJCC and ENETS staging systems in our collected data confirms that T category of tumors based on the criteria of both systems are concordant to every tumor site (kappa value, 0.8735) except for T3 in the ENETS system and T2 in the AJCC system (Table 4). After separate analyses of the T2 and T3 categories, we found that the discrepancy is caused by the different criteria of the two staging systems in the pancreas (Table 5). In survival analysis, T category of tumors in their sites of origin was a significant prognostic factor in all sites of the gastrointestinal tract; higher T category was significantly associated with worse prognosis (p<0.0001) (Fig. 4). Overall, the prognostic difference between T1 and T2 was not as significant as between T2 and T3 or T3 and T4. T2 (n=301) as defined by the 2010 AJCC staging system showed better prognosis than T3 tumors (n=88) in the pancreas (p<0.0001) (Fig. 5). However, the data was not appropriate for prognostic analysis between T2 and T3 using the ENETS system because only six cases of T2 were found, in contrast to 363 cases of T3.
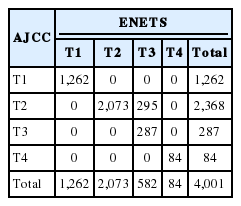
Distribution of case numbers based on T category by European Neuroendocrine Tumor Society (ENETS) and 2010 American Joint Cancer Committee (AJCC) systems in all samples
Distribution of case numbers based on T category by European Neuroendocrine Tumor Society (ENETS) and 2010 American Joint Cancer Committee (AJCC) systems in the pancreas
Kaplan-Meier survival curves according to T category by 2010 American Joint Cancer Committee (AJCC) staging system in stomach (A), small intestine (B), appendix (C), and colorectum (D) show that higher T category was significantly associated with worse prognosis (p<0.0001).
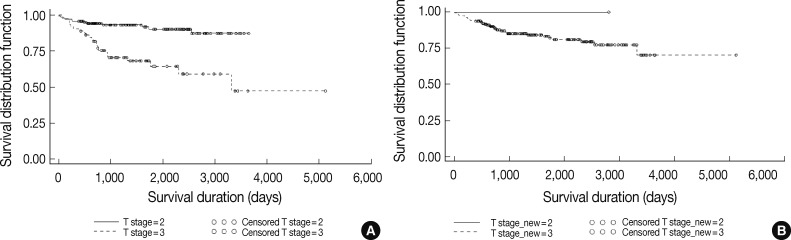
Kaplan-Meier survival curve of T2 according to T classification by 2010 American Joint Cancer Committee (AJCC) (A) shows better prognosis than T3 tumor (n=88) in the pancreas (p<0.0001), but only six cases of T2 were found, in contrast to 363 cases of T3 by European Neuroendocrine Tumor Society (ENETS) (B) staging system.
Lymph node metastasis and lymphovascular and perineural invasion
Lymph node metastasis, lymphovascular invasion, and perineural invasion of tumors were additional significant prognostic factors in GEP-NET (p<0.0001) (Fig. 6). Therefore, if possible, the description of the aforementioned parameters is recommended. From the description of histological classification of NENs, tumor necrosis and marked cellular atypia may indicate NEC.
Immunohistochemical stains
Immunohistochemical stains of synaptophysin and chromogranin A have been described as useful markers for detection of neuroendocrine differentiation. Well-differentiated NETs are usually not difficult to recognize on hematoxylin and eosin stained tumor slides; however, immunohistochemical stains for neuroendocrine markers are sometimes required for the diagnosis of NECs or mixed adenoneuroendocrine carcinomas (MANECs). We found that patients with GEP-NET that are positive for synaptophysin have better prognosis than those that are negative, but no prognostic significance was found for chromogranin A (Fig. 7).
DISCUSSION
From the analysis of our collected data, we found that histologic classification, grading, and staging are essential for the prognostic stratification of patients with NENs.
Histological diagnosis
- WDNET (well-differentiated neuroendocrine tumor)
- PDNEC (poorly-differentiated neuroendocrine carcinoma)
- MANEC (mixed adenoneuroendocrine carcinoma)
It has been difficult to classify GEP-NENs because of functional diversity and the nonrandom distribution of various neuroendocrine cells in the digestive system from which the tumors originate. There are still some debates over the contents of pathology reports due to significant changes made in classification systems over the last few decades, since the first WHO classification was proposed in 1980.4 The first thing that needs to be determined in diagnosis of NENs is whether it is a pure NEN or a MANEC.23 Subsequently, the pure NENs can be classified into well-differentiated tumors or poorly-differentiated carcinomas. Based on the 2010 WHO classification,6 the NETs (G1 and G2) include well-to-moderately differentiated tumors, while NECs comprise poorly-differentiated carcinomas. Considering the results of the survival analysis of our data, there is a significant difference between well-differentiated tumors and poorly-differentiated carcinomas.1 Although in rare cases, high-grade transformation of well-differentiated NETs has been reported,24 this biologic behavior of NETs is unclear. The AJCC proposed a separate staging system for well-differentiated NENs in 2010,8 but the staging for poorly-differentiated NETs is the same as for adenocarcinomas of the gastrointestinal tract. Therefore, the differentiation of well-differentiated NETs from poorly-differentiated NECs is the most basic and essential step of pathological diagnosis. The term "carcinoid tumor" is not recommended for use in daily practice because of the potential confusion with the 1980 WHO classification, in which all NETs were classified as carcinoid regardless of grade.
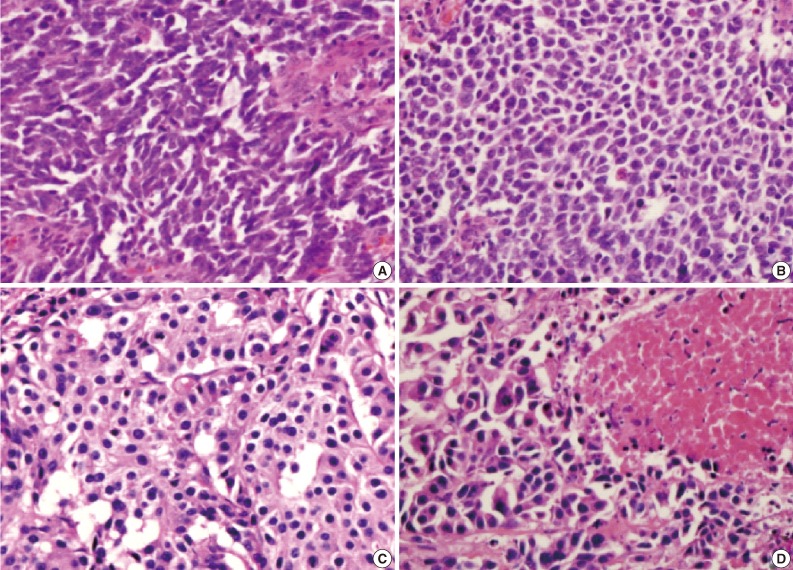
Well-differentiated NETs are composed of monomorphic small- to medium-sized cells with relatively abundant, finely granular cytoplasms and regular nuclei (Fig. 8). Oncocytic or clear cell features have also been described.25 There are different histologic patterns of tumor growth, which may be associated with tumor location and reflect the cell types composing the tumor.26 The solid pattern (type A or I) is usually found in enterochromaffin cell tumors of the small intestine and appendix, and the trabecular pattern (type B or II) is observed in L-cell tumors of the colon and rectum, in contrast to the glandular pattern (type C or III), which is seen in D cell tumors of the ampullary area. Pattern is not an essential component of the pathology report but is optional. If clinical information related to hormone hypersecretion is available, the term "functioning tumor" can be described together with the histologic classification of NENs. The central necrosis of tumor nests may be an indicator of poorly-differentiated NECs if it is associated with marked nuclear atypia and increased mitosis.6 It is helpful to make a correct diagnosis of NECs with the organoid pattern (Fig. 9) resembling well-differentiated NETs. However, cytologic atypia with apoptosis in large solid well-differentiated tumors should be interpreted as a regressive change, if mitosis is not increased.

The histologic patterns of well-differentiated neuroendocrine tumors can be divided into solid (A), trabecular (B), glandular (C), and cytologic atypia (D).
Grading
- G1: mitosis, <2/10HPF or Ki-67 labeling index, ≤2%
- G2: mitosis, 2-20/10HPF or Ki-67 labeling index, 3-20%
- G3: mitosis, >20/10HPF or Ki-67 labeling index, >20%
The grade of NENs indicates the proliferative activity of tumors and is assessed by mitotic counting and/or Ki-67 labeling index (Fig. 10). If there is a discrepancy between the count of mitosis and the Ki-67 labeling index, the higher one (whichever) should be accepted. With regard to the assessment of Ki-67 labeling index, heterogeneity in Ki-67 expression in the tumor and the subjective nature of the assessment should be kept in mind.27 For the evaluation of Ki-67 immunohistochemical stains, the use of an image analysis system or a visual estimate has been suggested. However, an automated system is not recommended for use because of the existence of non-tumoral Ki-67-positive cells and overlapping of nuclei. A visual estimate is also not recommended as a general rule for daily practice, especially in NET G2. The number of tumor cells can be variable in a HPF (×400) depending on the amount of stroma and tumor cell size, with a maximum number of 1,000. In the absence of significant stroma, there are up to approximately 20 Ki-67-positive cells in NET G1 and up to 200 Ki-67-positive cells in NET G2 in one HPF. Therefore, a tumor with marginal value of Ki-67-positive tumor cells between G1 and G2 or G2 and G3 should be carefully evaluated. Due to the heterogeneity in tumor cell proliferation, the grading of tumors in small biopsies can be problematic, regardless of evaluation method.
Staging
Size: _______×_______ cm
if multiple; the deepest one: _______×_______ cm, the largest one: _______×_______ cm.
Extent:
if multiple; the deepest one: _______, the largest one: _______.
The T category of NETs in the digestive tract is determined by tumor size and extent. In the case of multiple tumors, the affix "m" can be used for T category;8 additionally, if the tumors with the largest size and the deepest extent are not the same, they should be separately described. The prognosis of tumor may be related with the higher T category.
The discrepancy between 2010 AJCC and ENETS staging systems found in our data originates from the size criteria of T3 for pancreatic NENs according to ENETS (Table 5).
Tumors in 88 cases were larger than 4 cm and, despite their confinement to the pancreas, were classified as T3 by ENETS. However, according to AJCC they are considered T2 (Table 6). In the pancreas, T2 tumors according to AJCC, some of which are T3 by ENETS, showed better prognosis than AJCC T3. T category by AJCC seems to be more useful than that by ENETS for the prognostic stratification of patients. However, further analysis is required to prove this finding because the clinical information regarding treatment is not considered in this study. The benefit of ENETS staging has been previously described by a large-scale study.28 Therefore, we recommend that the staging system used for a pathology report should be specified, especially in pancreatic NENs. The other problem in staging of pancreatic NENs is the definition of peripancreatic tumor extension. According to the ENETS staging system, NENs with invasion to the duodenum or bile duct are categorized as T3; however, neither ENETS nor AJCC has set a specified criterion for "peripancreatic extension" in NENs of the pancreatic tail. The pancreatic capsule is not distinctly defined and therefore creates some confusion in making a decision of peripancreatic tumor extension for T3 in both AJCC and ENETS systems. Further study for the clarification of the definition of peripancreatic tumor extension is required.
For the prognostic stratification of patients, pathologists have an important role in providing the detailed description of pathologic characteristics of NENs. Therefore, we propose that the essential data set for standardized pathology report is as follows.
Essential data set for the pathology report of resected NENs
- Histological diagnosis: well-differentiated vs poorly-differentiated; functioning tumor name, if clinical data is available
- Grade: mitosis and/or Ki-67 labeling index
-
- Stage: staging system should be specified (AJCC or ENETS), especially for pancreatic NENs
T: size and extent
N: lymph node metastasis, if available
- Resection margins
- Lymphatic invasion, perineural invasion
- Immunohistochemical staining: synaptophysin, chromogranin (optional)
- Associated pathological findings: MEN or gastric NENs, if information is available
Notes
No potential conflict of interest relevant to this article was reported.