Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(6); 2013 > Article
-
Letter to the Editor
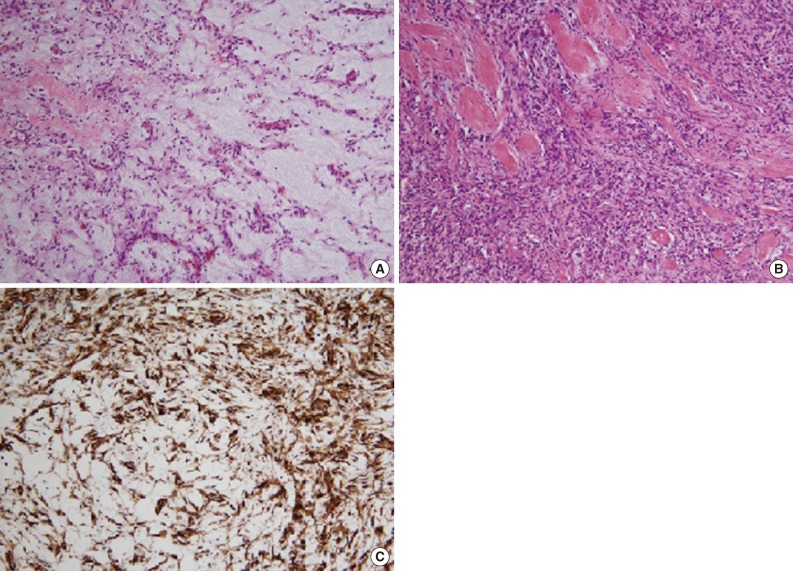
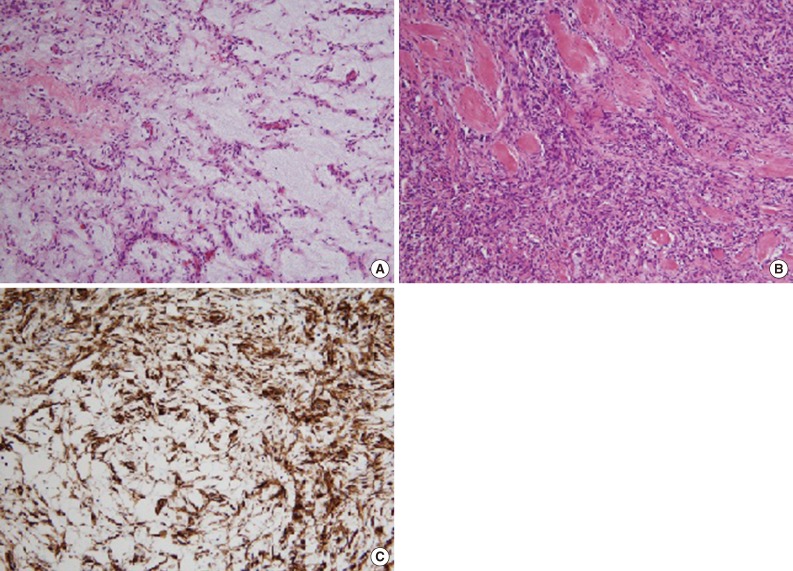
Myxoid Solitary Fibrous Tumor of the Central Nervous System - Haeri Han, Sangjeong Ahn1, Won Hwangbo1, Yang Seok Chae1
-
Korean Journal of Pathology 2013;47(6):505-506.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.505
Published online: December 24, 2013
Department of Medicine, Korea University School of Medicine, Seoul, Korea.
1Department of Pathology, Korea University Anam Hospital, Korea University School of Medicine, Seoul, Korea.
- Corresponding Author: Yang Seok Chae, M.D. Department of Pathology, Korea University Anam Hospital, Korea University College of Medicine, 73 Inchon-ro, Seongbuk-gu, Seoul 136-705, Korea. Tel: +82-2-920-6155, Fax: +82-2-920-6576, 'chaeys21@korea.ac.kr'
• Received: July 29, 2013 • Revised: November 6, 2013 • Accepted: November 7, 2013
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1. Bisceglia M, Galliani C, Giannatempo G, et al. Solitary fibrous tumor of the central nervous system: a 15-year literature survey of 220 cases (August 1996-July 2011). Adv Anat Pathol 2011; 18: 356–392. PMID: 21841406. ArticlePubMed
- 2. Hayashi Y, Uchiyama N, Hayashi Y, et al. A reevaluation of the primary diagnosis of hemangiopericytoma and the clinical importance of differential diagnosis from solitary fibrous tumor of the central nervous system. Clin Neurol Neurosurg 2009; 111: 34–38. PMID: 18922629. ArticlePubMed
- 3. Eom DW, Khang SK, Kim CJ, Ro JY. Solitary fibrous tumor of meninges in pituitary fossa: a case report. Korean J Pathol 2003; 37: 137–140.
References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Cervical Myxoid Solitary Fibrous Tumor: Report of an Unusual Variant and a Brief Overview of the Literature
Bingcheng Wu, Sok Yan Tay, Fredrik Petersson
Head and Neck Pathology.2020; 14(3): 852. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

 E-submission
E-submission