Pathologic Factors Associated with Prognosis after Adjuvant Chemotherapy in Stage II/III Microsatellite-Unstable Colorectal Cancers
Article information
Abstract
Background:
Although there are controversies regarding the benefit of fluoropyrimidine-based adjuvant chemotherapy in patients with microsatellite instability–high (MSI-H) colorectal cancer (CRC), the pathologic features affecting postchemotherapeutic prognosis in these patients have not been fully identified yet.
Methods:
A total of 26 histopathologic and immunohistochemical factors were comprehensively evaluated in 125 stage II or III MSI-H CRC patients who underwent curative resection followed by fluoropyrimidine-based adjuvant chemotherapy. We statistically analyzed the associations of these factors with disease-free survival (DFS).
Results:
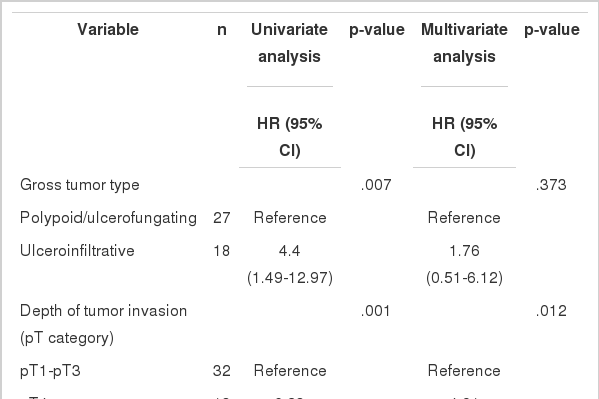
Using a Kaplan- Meier analysis with log-rank test, we determined that ulceroinfiltrative gross type (p=.003), pT4 (p<.001), pN2 (p=.002), perineural invasion (p=.001), absence of peritumoral lymphoid reaction (p=.041), signet ring cell component (p=.006), and cribriform comedo component (p=.004) were significantly associated with worse DFS in patients receiving oxaliplatin-based adjuvant chemotherapy (n=45). By contrast, pT4 (p<.001) and tumor budding-positivity (p=.032) were significant predictors of poor survival in patients receiving non-oxaliplatin–based adjuvant chemotherapy (n=80). In Cox proportional hazards regression model-based univariate and multivariate analyses, pT category (pT1-3 vs pT4) was the only significant prognostic factor in patients receiving non-oxaliplatin–based adjuvant chemotherapy, whereas pT category, signet ring cell histology and cribriform comedo histology remained independent prognostic factors in patients receiving oxaliplatin-based adjuvant chemotherapy.
Conclusions:
pT4 status is the most significant pathologic determinant of poor outcome after fluoropyrimidine-based adjuvant chemotherapy in patients with stage II/III MSI-H CRC.
In the current management strategy for colorectal cancer (CRC), fluoropyrimidine-based adjuvant chemotherapy is generally recommended for all patients with stage III CRC and for a subset of patients with high-risk stage II CRC [1]. However, some previous studies have reported that in patients with microsatellite instability–high (MSI-H) CRC, adjuvant chemotherapy based on fluorouracil, which is the most commonly used intravenous fluoropyrimidine agent, had little or no benefit [2]. Although the mechanisms underlying and the factors determining this poor response to fluorouracil-based adjuvant chemotherapy in MSIH CRC patients remain incompletely understood, previous in vitro experiments have revealed that intact DNA mismatch repair function is necessary for fluorouracil to induce apoptotic effects on cancer cells [3,4]. This finding supports the observed resistance of patients with MSI-H CRC to fluorouracil-based adjuvant chemotherapy.
MSI-H CRC is characterized by unique pathologic features, including predilections for proximal tumor location, mucinous histology, medullary tumor morphology, signet ring cell tumor component, poor tumor differentiation, tumor-infiltrating lymphocytes, Crohn-like lymphoid reaction and peritumoral lymphoid reaction [5]. Molecularly, MSI-H CRC is caused by DNA mismatch repair deficiency, which is usually due to the inactivation of at least one of the mismatch repair genes, including MLH1, MSH2, MSH6, and PMS2, by germline mutation or acquired promoter hypermethylation [2]. Recent investigations have also determined that germline EPCAM deletion-induced MSH2 epimutation can be one of the causes of Lynch syndromeassociated MSI-H CRC [6,7]. In addition, it is well known that sporadic MSI-H CRC is closely associated with MLH1 methylation, CpG island methylator phenotype and BRAF V600E mutations [2]. Based on the pathologic and molecular heterogeneity of MSI-H CRC, it is strongly expected that there may be pathologic or molecular factors affecting prognostic heterogeneity and differential chemotherapy responses in MSI-H CRC [2]. In this context, our previous investigation revealed that the concurrent loss of caudal type homeobox 2 (CDX2) and cytokeratin 20 (CK20) expression in tumors indicates an aggressive clinical phenotype that is associated with early death or tumor recurrence in patients with MSI-H CRC [8]. Ricciardiello et al. [9] previously reported that in CRC patients, MSI-H status is associated with high expression of thymidylate synthase (TS), the target molecule for fluorouracil. Accordingly, this finding could be a putative underlying mechanism of resistance to fluorouracil chemotherapy in MSI-H CRC patients [9], although this has not been clearly shown [10-12]. Recently, Dorard et al. [13] demonstrated that mutant HSP110 expression and its causal mutation, HSP110 T17 microsatellite deletions, can be prognostic and predictive markers in MSI-H CRC [13]. Furthermore, we have also identified the usefulness of wild-type HSP110 (HSP110wt) immunohistochemistry (IHC) for prognostication in MSI-H CRC [14].
MSI-H CRC is associated with various features, but definitive pathologic or molecular factors that can be used to predict the response to adjuvant chemotherapy in patients with MSI-H CRC have yet to be fully identified. Therefore, we decided to investigate the comprehensive pathologic features that are potentially associated with postchemotherapeutic prognosis in MSI-H CRC patients. Through this intensive analysis, we anticipated identifying the major determining factors for chemotherapy response in MSI-H CRC patients that would be helpful for predicting patient prognosis and establishing treatment strategies in the clinical setting.
MATERIALS AND METHODS
Study samples
A total of 125 MSI-H CRC tissues were retrospectively collected from the pathology archives of Seoul National University Hospital, Seoul, Korea and Seoul National University Bundang Hospital, Seongnam, Korea. All samples were obtained from patients who underwent curative surgery and subsequent adjuvant chemotherapy for CRC at these institutions between 2004 and 2008. During this time, 2,957 consecutive patients with CRC who were treated at these institutions were subjected to MSI analysis conducted by the molecular pathology division of Seoul National University Hospital; of these patients, 237 were diagnosed as MSI-H. Among them, patients who were determined to be American Joint Committee on Cancer TNM stage I or IV and who had undergone surgery alone or preoperative neoadjuvant chemotherapy or radiation therapy for the treatment of CRC were excluded. Finally, 125 stage II or III MSI-H CRC patients who had received postoperative fluoropyrimidinebased chemotherapy as a first-line adjuvant treatment were included in this study. Of these patients, 51 received fluorouracil/ leucovorin, 29 received oral prodrug of fluorouracil (21 capecitabine and 8 tegafur-uracil), 43 received fluorouracil/leucovorin/ oxaliplatin and 2 received capecitabine/oxaliplatin. MSI analysis was previously performed in the molecular pathology laboratory of Seoul National University Hospital [14]. Five microsatellite markers (BAT-25, BAT-26, D5S346, D17S250, and D2S123) recommended by the National Cancer Institute were used in the MSI analysis, and MSI-H status was defined as the presence of two or more markers showing instability in tumor DNA compared with normal DNA.
Ethics statement
This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. H-1203-072- 402). Under the condition of retrospective archival tissue collection and data anonymization, our study was exempt from informed consent of the participants. All patient records/information were anonymized and de-identified prior to analysis.
Surgical pathology analysis
We reviewed the surgical and pathological reports and retrieved data on tumor location, size, multiplicity, and gross type. For survival analysis, all patients were categorized into proximal or distal for tumor location using the splenic flexure as a dividing point and were classified into large or small for tumor size using a cutoff value of the average tumor size (7 cm). Two pathologists (J.H.K. and J.M.B.), who were blinded to the clinicopathologic and molecular data of the cases, independently evaluated the histopathologic features of the 125 MSI-H CRCs by examining hematoxylin and eosin-stained tissue slides using light microscopy. The assessed histopathologic factors included tumor border, pT/pN categories, lymphovascular invasion, perineural invasion, tumor differentiation, tumor budding, peritumoral lymphoid reaction, Crohn-like lymphoid reaction, mucinous, signet ring cell, medullary, serrated, and cribriform comedo tumor components. Conflicting assessment results between the two pathologists were reviewed and discussed, and a consensus was reached. The assessment criteria for histologic parameters used in this study are described below.
Tumor differentiation
Although all MSI-H CRCs are considered low-grade tumors according to the 2010 World Health Organization (WHO) classification [15], the degree of histomorphologic differentiation for each tumor in this study was graded as one of three differentiation statuses (well, moderately, or poorly differentiated) based on the percentage of gland formation (>95%, 50%–95%, and <49%, respectively).
Tumor budding
Tumor budding status was evaluated as previously described [16]. Tumor budding was defined as a single tumor cell or a cluster composed of <five tumor cells at the invasive margin. Under a light microscopic field with ×200 magnification, the number of tumor buds was counted in the most intensive budding area. A tumor showing five or more buds in this area was determined to be tumor budding-positive.
Peritumoral lymphoid reaction
The peritumoral lymphoid reaction was assessed using the four-tier scoring system suggested by Klintrup et al. [17]. No increase in lymphoid cells at the invasive margin was scored as 0; a mild and patchy increase in lymphoid cells without destruction of tumor cells by lymphocytes was scored as 1; a band-like infiltration of lymphoid cells at the invasive margin with focal destruction of tumor cells by lymphocytes was scored as 2; and a cup-like intense lymphoid infiltration at the invasive margin with frequent destruction of tumor cells by lymphocytes was scored as 3. Among the 125 cases, four were excluded from the peritumoral lymphoid reaction assessment owing to suboptimal staining or tissue section qualities of peritumoral areas.
Crohn-like lymphoid reaction
Crohn-like lymphoid reaction activity was evaluated using Ueno’s criteria [18]. The maximum size of the largest lymphoid aggregate of Crohn-like lymphoid reaction in CRC was measured. Tumors with the largest lymphoid aggregate ≥1 mm were classified into the active reaction group, whereas tumors with the largest lymphoid aggregate <1 mm were classified into the inactive reaction group. Among the 125 cases, four were excluded from the Crohn-like lymphoid reaction assessment owing to suboptimal staining or tissue section qualities of peritumoral areas.
Mucinous histology
The degree of extracellular mucin pools in a tumor was assessed as absent, focal (<50% of tumor area), or diffuse (≥50% of tumor area).
Signet ring cell tumor component
The signet ring cell component in a tumor was assessed as absent, focal (<50% of tumor cells), or diffuse (≥50% of tumor cells).
Medullary tumor component
The medullary component in a tumor was assessed as absent, focal (<50% of tumor cells), or diffuse (≥50% of tumor cells). Medullary features were determined based on the combination of sheet-like growth pattern of large tumor cells, high nuclear/ cytoplasmic ratios, abundant amphophilic cytoplasm, vesicular nuclei, prominent nucleoli and frequent tumor-infiltrating lymphocytes [19].
Serrated tumor component
The serrated component in a tumor was assessed as absent, focal (<50% of tumor cells), or diffuse (≥50% of tumor cells). Serrated morphology was determined based on the combination of glandular serrations, abundant eosinophilic or clear cytoplasm, vesicular nuclei, prominent nucleoli, absence of necrosis and intra- and extracellular mucin [20].
Cribriform comedo tumor component
The cribriform comedo component in a tumor was assessed as absent, focal (<50% of tumor cells), or diffuse (≥50% of tumor cells). Cribriform comedo histology was defined as cribriform gland architecture with a comedo-like necrosis pattern resembling breast intraductal carcinoma [21].
Immunohistochemistry
Tissue microarray (TMA) construction and IHC were conducted as previously described [14]. For TMA construction, three tissue cores corresponding to three different areas of cancer were extracted from formalin-fixed, paraffin-embedded tissue blocks of individual cases. Immunostaining with antibodies against MLH1 (Dako, Glostrup, Denmark), MSH2 (Invitrogen, Camarillo, CA, USA), PMS2 (Ventana Medical Systems, Tucson, AZ, USA), MSH6 (Ventana Medical Systems), CDX2 (Ventana Medical Systems), CK20 (Dako), TS (Invitrogen), and HSP110wt (NCL-HSP105, Leica Biosystems, Newcastle upon Tyne, UK) was performed on TMA blocks composed of all 125 MSI-H CRC tissues. Automated immunohistochemical staining was conducted using the BenchMark XT immunostainer (Ventana Medical Systems) according to the manufacturer’s protocol. The expression of CDX2, CK20 and each of the mismatch repair proteins was assessed to be negative (loss) or positive (retained), as previously described [8]. The positivity of CDX2 and mismatch repair proteins was determined when a nuclear staining pattern in tumor cells was observed. CK20 expression was determined to be positive when a cytoplasmic to membranous staining pattern in tumor cells was observed. HSP110wt and TS expression statuses were evaluated semiquantitatively using a four-tier scoring system based on staining intensity (0/1+/2+/3+), as previously described [14,22]. The detailed steps of HSP110wt and TS assessment were as follows. Among the three tissue cores of each tumor case, identical scores for two or more tissue cores determined the overall score for the case. Subsequently, for survival analysis, all cases were dichotomously categorized into negative (0) or positive (1+/2+/3+) for HSP110wt expression status and low (0/1+) or high (2+/3+) for TS expression status. The assessment of all immunohistochemical stainings in this study was performed independently by two pathologists (J.H.K. and J.M.B.), who were blinded to the clinicopathologic and molecular data. Conflicting assessment results between the two pathologists were reviewed and discussed, and a consensus was reached.
Statistical analysis
All statistical analyses in this study were performed using IBM SPSS Statistics ver. 20 (IBM Co., Armonk, NY, USA). By reviewing the medical records of our institutions and using the Micro Data Service System by Statistics Korea, the times of death, tumor recurrence and the last clinical follow-up for disease-free survival (DFS) data were collected. The average DFS time was 1,817 days and ranged from 29 to 3,186 days. The DFS rates were analyzed using the Kaplan-Meier method with the log-rank test. To identify independent prognostic factors, univariate and multivariate survival analyses were performed using the Cox proportional hazards regression model. For survival analysis, all 125 patients included in this study were divided into two groups: those receiving oxaliplatin-based therapy (n=45; 43 fluorouracil/leucovorin/oxaliplatin, 2 capecitabine/ oxaliplatin) and those receiving non-oxaliplatin–based therapy (n=80; 51 fluorouracil/leucovorin, 21 capecitabine, 8 tegafururacil). All p-values were two-sided, and statistical significance was determined at p<.05.
RESULTS
Pathologic features of study samples
The pathologic and immunophenotypic features of 125 MSIH CRC patients treated with fluoropyrimidine-based adjuvant chemotherapy are summarized in Table 1. Representative photomicrographs of histopathologic and immunohistochemical features, including tumor budding, mucinous histology, signet ring cell component, medullary component, serrated morphology, cribriform comedo histology, HSP110wt expression and TS expression, are demonstrated in Figs. 1 and 2, respectively.

The pathologic features of samples used in this study (stage II/III MSI-H CRCs treated with fluoropyrimidine-based adjuvant chemotherapy)
Histopathologic features in microsatellite instability–high colorectal cancers. (A) A case determined to be tumor budding–positive (buds ≥5). (B) A case classified as mucinous adenocarcinoma. (C) A case classified as signet ring cell carcinoma. (D) A case classified as medullary carcinoma. (E) A case showing a serrated tumor component. (F) A case showing a cribriform comedo-type tumor component.
Immunohistochemical expression of wild-type HSP110 (HSP110wt) and thymidylate synthase (TS) in microsatellite instability–high colorectal cancers. (A) A case showing high-level expression of HSP110wt (score 3+). (B) A case showing HSP110wt-negativity (score 0). (C) A case showing high-level expression of TS (score 3+). (D) A case showing low-level expression of TS (score 0).
Survival analysis
In the preliminary survival analysis of patients treated with oxaliplatin- and non-oxaliplatin–based therapies, there were no significant differences in DFS between polypoid and ulcerofungating types, pT1 and pT3, pN0 and pN1, scores 1, 2, and 3 for peritumoral lymphoid reaction, well differentiation and moderate differentiation, focal presence (<50%) and diffuse presence (≥50%) of each tumor component (mucinous, signet ring cell, medullary, serrated, and cribriform comedo components), and 1+, 2+, and 3+ of HSP110wt expression. Therefore, we decided to unify each of these sub-classifications into one category, and consequently, all pathologic variables assessed in this study were dichotomously categorized for subsequent survival analyses (Table 1).
Kaplan-Meier survival analysis with log-rank test revealed that, among the 26 pathologic and immunohistochemical factors, ulceroinfiltrative gross tumor type (p=.003) (Fig. 3A), pT4 stage (p<.001) (Fig. 3B), pN2 stage (p=.002) (Fig. 3C), presence of perineural invasion (p=.001) (Fig. 3D), absence of peritumoral lymphoid reaction (p=.041) (Fig. 3E), presence of signet ring cell component (p=.006) (Fig. 3F), and presence of cribriform comedo histology (p=.004) (Fig. 3G) were significant factors for poorer DFS in MSI-H CRC patients who were treated with oxaliplatin-based adjuvant chemotherapy. In contrast, pT4 stage (p<.001) (Fig. 4A) and tumor budding-positivity (p=.032) (Fig. 4B) were significantly associated with poorer DFS in patients treated with non-oxaliplatin–based chemotherapy. Notably, although a statistical significance in survival differences was not observed, there were no deaths or incidences of CRC recurrence in patients with the HSP110wt-negative phenotype (Figs. 3H, Fig. 4C).
Kaplan-Meier survival analyses of microsatellite instability–high colorectal cancer patients receiving oxaliplatin-based chemotherapy (n=45). (A-G) The disease-free survival of patients differed significantly according to gross tumor type (A), pT category (B), pN category (C), perineural invasion (D), peritumoral lymphoid reaction (E), signet ring cell component (F), and cribriform comedo component (G). (H) Note the absence of death or tumor recurrence in patients with wild-type HSP110 (HSP110wt)-negative tumors.
Kaplan-Meier survival analyses of microsatellite instability-high colorectal cancer patients receiving non-oxaliplatin–based chemotherapy (n=80). (A, B) The disease-free survival of patients differed significantly according to the pT category (A) and tumor budding (B). (C) Note the absence of death or tumor recurrence in patients with wild-type HSP110 (HSP110wt)-negative tumors.
Finally, to determine the most significant factor among the pathologic prognosticators, we performed univariate and multivariate survival analyses using the Cox proportional hazards regression model. In univariate analysis, gross tumor type, pT category, pN category, perineural invasion, signet ring cell component and cribriform comedo component were significant prognostic factors in patients treated with oxaliplatin-based therapy (Table 2). By contrast, only the pT category was a significant factor in patients treated with non-oxaliplatin–based therapy (hazard ratio, 17.6; 95% confidence interval, 3.34 to 92.8; p= .001). In multivariate analysis, the pT4 stage, signet ring cell histology and cribriform comedo histology were determined to be independent prognostic factors associated with poor DFS in patients treated with oxaliplatin-based therapy (Table 2).
DISCUSSION
MSI-H is one of the major molecular subtypes of CRC and has been thought to be associated with poor response to fluorouracil-based adjuvant chemotherapy. However, recent evidence has suggested that MSI is not a significant factor for determining postchemotherapeutic prognosis in CRC patients who have been treated with oxaliplatin-based adjuvant chemotherapy [2]. Although controversy may still remain, these findings imply that adding oxaliplatin to fluorouracil-based chemotherapy regimens may be important for overcoming fluorouracil-resistance in MSI-H CRC patients. Therefore, because the pathologic and molecular factors that affect patient prognosis after adjuvant chemotherapy could be fundamentally different depending on the presence or absence of oxaliplatin in their chemotherapy regimens, for survival analysis, all 125 patients with MSI-H CRC in our present study were divided into patient subgroups based on whether they were treated with oxaliplatin- or non-oxaliplatin–based therapy.
In terms of pathology, the depth of tumor invasion (pT category), lymph node metastasis (pN category), gross tumor type, tumor budding, perineural invasion, lymphocytic reactions, and signet ring cell tumor component are known prognostic pathologic factors in CRC [23]. Therefore, it is not surprising that in the present study, these features were confirmed as being significant factors for postchemotherapeutic prognosis in patients with MSI-H CRC. However, several interesting issues regarding the prognostic pathologic features identified in our study remain to be addressed.
One of our interesting findings is the potential association between the peritumoral lymphoid reaction and the response to oxaliplatin-based chemotherapy in CRC (Fig. 3E). It has been well documented that host immune reactions against the tumor can determine the prognosis of cancer patients. It has also been reported that peritumoral inflammatory reaction is an independent prognostic factor in patients with CRC [24]. However, there has not been enough evidence to support a relationship between peritumoral inflammatory reaction and treatment response in CRC patients receiving adjuvant chemotherapy. Therefore, our data provide an important and timely indication of the value of peritumoral lymphoid reaction in predicting the response of CRC patients to oxaliplatin-based chemotherapy. According to a previous in vitro study, oxaliplatin can induce the immunogenic death of CRC cells [25], and this finding could account for the favorable prognostic effect of peritumoral lymphoid reaction during oxaliplatin-based chemotherapy in patients with CRC.
Another interesting finding is the prognostic significance of cribriform comedo-type histology in MSI-H CRC patients receiving oxaliplatin-based chemotherapy (Table 2, Fig. 3G). According to a previous study by Chirieac et al. [21], the presence of cribriform comedo gland patterns in microsatellite-stable CRCs was significantly associated with CpG island hypermethylation. However, the detailed prognostic implications of the cribriform comedo morphology in CRC, including both MSI-H and MSIlow/microsatellite-stable phenotypes, have not been studied. To the best of our knowledge, our investigation is the first study reporting the prognostic impact of cribriform comedo histology in CRC, though our study samples were restricted to patients with MSI-H tumors receiving adjuvant chemotherapy. As such, additional efforts to elucidate the clinicopathologic and molecular associations and the prognostic values of cribriform comedo histology in CRC are needed.
Previous studies have suggested a few molecular factors putatively associated with resistance to fluorouracil chemotherapy in CRC, such as TS expression, but the practical predictive value of these factors remains unclear [26]. In addition, although the beneficial effect of fluorouracil-based adjuvant chemotherapy in patients with MSI-H CRC has been doubtful, few established biomarkers can be used to stratify MSI-H CRC patients into chemotherapy-responsive or chemotherapy-nonresponsive subgroups. In this context, recent investigations have reported notable findings regarding HSP110 T17 deletions and HSP110 expression alterations as promising prognostic and predictive markers in MSI-H CRC [13]. In our previous study, we suggested that IHC for HSP110wt could be a useful tool for stratifying prognostic subgroups of patients with MSI-H CRC [14]. Therefore, we also applied HSP110wt immunostaining in the present study to verify the predictive value of this method in MSI-H CRC patients undergoing adjuvant chemotherapy. However, there were no significant survival differences according to HSP110wt expression status in the patient groups receiving either oxaliplatin- or non-oxaliplatin–based therapies (Figs. 3H, 4C). Interestingly, although the results of survival analysis were not statistically significant, all patients with HSP110wt-negative tumors did not experience death or tumor recurrence. This finding was consistent with the results of our previous investigation. In our previous study, among 168 MSI-H CRC patients, there were no deaths or incidences of tumor recurrence in patients with HSP110wt-negative tumors [14]. Collectively, our previous and present data suggest that HSP110wt-negative MSI-H CRCs may be characterized by remarkably favorable prognosis. Although we could not prove the prognostic significance of HSP- 110wt expression in our cohort of MSI-H CRC patients receiving adjuvant chemotherapy, the potential associations between HSP110 mutation/HSP110 expression statuses and responses to chemotherapy in MSI-H CRC should be further evaluated.
The final issue to be addressed is an interpretation of our study results in terms of potential chemotherapy resistance in MSI-H CRC. Interestingly, recent investigations have suggested that the prognostic impact of the pT category has been underestimated in CRC staging. According to the study by Li et al. [27], the pT category is more significantly associated with patient survival than the pN category in CRC. In addition, according to the study by Snaebjornsson et al. [28], pT4 is the most significant determinant of poor survival in stage II/III colon cancer patients. Based on these reports, our conclusion that pT4 status is the most important indicator of poor outcome after adjuvant chemotherapy in stage II/III MSI-H CRC suggests that the adverse prognostic effect of the major high-risk factor (pT4) in stage II/III CRC is not improved after adjuvant chemotherapy in MSI-H CRC. In other words, this finding may reflect poor responses to fluoropyrimidine-based adjuvant chemotherapy in patients with MSI-H CRC.
In summary, regardless of the efficacy of fluoropyrimidine-based adjuvant chemotherapy in MSI-H CRC patients, the depth of tumor invasion can be considered the most significant pathologic factor associated with postchemotherapeutic prognosis in patients with locally advanced MSI-H CRC. In addition, other pathologic factors, including gross tumor type, lymph node metastasis, perineural invasion, peritumoral lymphoid reaction, signet ring cell component, cribriform comedo histology, and HSP110 expression, should be further evaluated as potential predictive factors for response to adjuvant chemotherapy in CRC patients.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This study was supported by a grant from the Basic Science Research Program through the National Research Foundation (NRF) funded by the Korean Ministry of Education (2013R1 A1A2059080), a grant from the Korea Health Technology R&D Project funded by the Korean Ministry of Health and Welfare (HI13C1804), the NRF grant funded by the Korean Ministry of Science, ICT and Future planning (2011-0030049), a grant from the Priority Research Centers Program through the NRF (2009-0093820), and a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute funded by the Korean Ministry of Health and Welfare (HI14C1277).