Analysis of Surgical Pathology Data in the HIRA Database: Emphasis on Current Status and Endoscopic Submucosal Dissection Specimens
Article information
Abstract
Background:
In Korea, medical institutions make claims for insurance reimbursement to the Health Insurance Review and Assessment Service (HIRA). Thus, HIRA databases reflect the general medical services that are provided in Korea. We conducted two pathology-related studies using a HIRA national patient sample (NPS) data (selection probability, 0.03). First, we evaluated the current status of general pathologic examination in Korea. Second, we evaluated pathologic issues associated with endoscopic submucosal dissection (ESD).
Methods:
The sample data used in this study was HIRA-NPS-2013-0094.
Results:
In the NPS dataset, 163,372 pathologic examinations were performed in 103,528 patients during the year 2013. Considering sampling weight (33.3), it is estimated that 5,440,288 (163,372 × 33.3) pathologic examinations were performed. Internal medicine and general surgery were the most common departments requesting pathologic examinations. The region performing pathologic examinations were different according to type of medical institution. In total, 490 patients underwent ESD, and 43.4% (213/490) underwent ESD due to gastric carcinoma. The results of the ESD led to a change in disease code for 10.5% (29/277) of non-gastric carcinoma patients. In addition, 21 patients (4.3%) underwent surgery following the ESD. The average period between ESD and surgery was 44 days.
Conclusions:
HIRA sample data provide the nation-wide landscape of specific procedure. However, in order to reduce the statistical error, further studies using entire HIRA data are needed.
In Korea, all medical institutions claim insurance reimbursements for services to the Health Insurance Review and Assessment Service (HIRA). Thus, HIRA databases reflect the general medical services provided in Korea. Since the entire HIRA database is too big to analyze, HIRA provides a specific set of data according to researcher’s requests. HIRA also provides some relatively small sized data sets (statistically extracted, anonymized, and annualized) for research and public purposes [1]. These sample data included national patient sample (NPS), a national inpatient sample, an adult patient sample (65 years or older), and a pediatric patient sample. To the best of our knowledge, this is the first pathology-related analysis using HIRA data.
We conducted two pathology-related studies using HIRA-NPS data. First, we analyzed the rate of surgical pathologic examinations in Korea. After Kamegoro Inamoto introduced pathology to Korea in 1914, pathologic examinations have played a major role in medical services for the improvement of overall care [2]. However, research on the frequency of pathologic examinations in this nation as a whole have not been performed due to a restriction on the sharing of personal medical records.
Next, we analyzed the pathologic results of endoscopic submucosal dissection (ESD) specimens. ESD is considered as an initial treatment modality for early and localized gastric carcinoma or benign epithelial neoplasm [3]. We evaluated several ESD-related parameters. After ESD and pathologic examination, surgical treatment is called for in those cases that show tumor cells in the resection margins, endolymphatic tumor emboli, or submucosal invasion [4]. Several papers have been published on this subject, but most of them are from a single institute and so do not incorporate the data of those patients who later went on to undergo additional surgery in different hospitals [5,6]. One of the advantageous features of the HIRA database is that patients can be tracked through several medical institutions, thereby enabling the study of a more complete data set including those that received secondary treatment in one hospital after ESD in another hospital.
MATERIALS AND METHODS
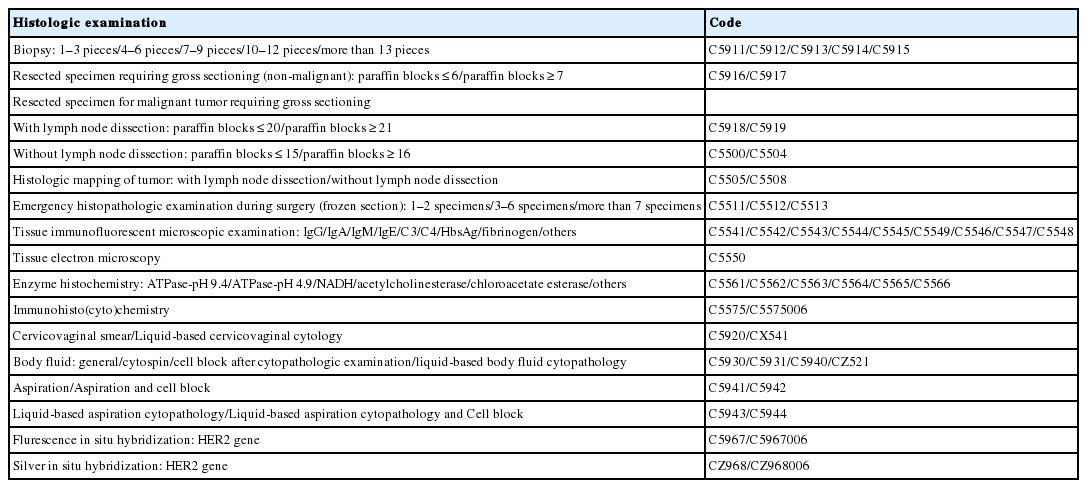
The sample data used in this study was HIRA-NPS-2013-0094. This sample was composed of 26 text files, and the total file size was 16.6 gigabytes (GB). The HIRA data tables were composed of five main tables (general specification, healthcare services, diagnosis information, prescriptions, and general information about the medical institutions). Each table was conjoined with proper claim numbers or medical institution numbers. The disease codes were based on the Korean Standard Classification of Disease (KCD). Specifications of the computer that was used to analyze the data were as follows: central processing unit (CPU), i3-2120 3.30 GHz (Intel, Santa Clara, CA, USA); 32 GB main memory; operating system (OS), Ubuntu 14.04.3 long-term support (LTS); and R 3.2.2 analysis software. The pathologic examination codes used in this study are summarized in Table 1. The sample data contained 22,344,536 claims in 1,361,717 patients (selection probability, 0.03; sampling weight, 33.3).
RESULTS
Pathologic examination statistics in Korea
In the year 2013, 163,372 pathologic examinations were performed in 103,528 patients (45,897 men and 57,631 women). The mean and median ages of the patients were 51.8 and 53 years, respectively. The skewness and kurtosis of patient age were –0.251 and 2.775, respectively. The pathologic examination data and medical institutions according to administrative district are summarized in Table 2. The total numbers of medical institutions according to administrative district are summarized in Appendix 1. In total, 43.5% of the tertiary hospitals (10/23), 15.6% of the general hospitals (48/307), and 23.8% of the other institutions (12,090/50,868) were located in Seoul. In addition, 32.9% of the surgical pathologic examinations (53,711/163,372) were requested in medical institutions located in Seoul.
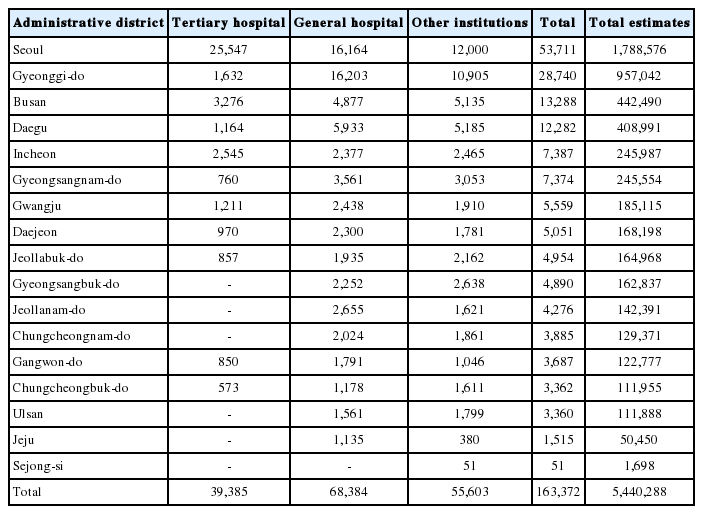
Pathologic examinations claims and requesting medical institutions according to administrative districts (sort based on the total number of claims)
Almost all medical and dental departments requested pathologic examinations (Table 3). Internal medicine (74,232, 45.4%), general surgery (34,808, 21.3%), obstetrics and gynecology (19,382, 11.9%), and urology (9,951, 6.1%) were the most common medical departments (84.7%) requesting pathology examinations. A small subset (38/17,892, 0.2%) of immunohistochemical (IHC) stains were not interpreted by qualified doctors (not claimed as “C5575006”) (data not shown). Claims for acetylcholinesterase (C5564) and chloroacetate esterase (C5565) examinations were not found in our data.

Pathologic examinations requests statuses according to medical departments (sort based on the total number of claims)
Among pathologic examination-associated claims, 162,002 examinations (99.2%) had proper claim codes (examination codes 09 and sub-code 01 (performed in their own institutions) or 02 (performed in outside institutions). Among pathologic examinations, 65.8% were performed in tertiary or general hospitals (39,385 and 67,225 cases, respectively) (Table 4). Almost all examinations claimed by tertiary hospitals were performed in their institute (39,349/39,385, 99.9%), and 85% of examinations claimed by general hospitals were performed (57,163/67,225) in their institute. The other medical institutions claimed considerable pathologic examinations performed by outside services (52,214/55,392, 94.3%).
According to the claims, 76,016 pathologic examinations (44.7%) were performed due to malignancy (disease code “C”) or non-malignant tumorous conditions (disease code “D00-D48”) (Table 5). IHC stains were more frequently performed in tumorous conditions (15,336/17,892, 85.7%). Pathologic examination of biopsy specimens was performed more frequently in non-tumorous conditions (42,661/61,875, 68.9%).
ESD-related statistics
In total, 509 ESDs were performed in 490 patients (341 males and 149 females) in 109 medical institutions. The median age of the patients was 66 years (age, 29 to 89 years; 1st quantile, 58 years; 3rd quantile, 71.75 years). The majority of patients (n=472) underwent one ESD; 17 patients underwent two ESDs (10 patients underwent simultaneous ESD, while seven patients underwent ESDs at different times), and one patient underwent three ESDs (two ESDs at the same time).
The disease codes noted when patients underwent ESD were as follows: C16 (malignant neoplasm of stomach), 213 patients (43.5%); non-C16, 277 patients (56.5%); D00.2 (carcinoma in situ of stomach), 17 patients; D13.1 (benign neoplasm of stomach), 226 patients; D13.9 (benign neoplasm of ill-defined site within the digestive system), one patient; and other, 33 patients. Disease codes changed after the ESD in 10.5% of the non-C16 patients (29/277): D00.2 to C16, seven patients; D13.1 to D00.2, three patients; D13.1 to C16, 18 patients; and D13.9 to C16, one patient (Table 6).
Twenty-one patients (21/490, 4.3%) underwent gastrectomy following ESD, and all of these patients underwent ESD for only once. Fifteen patients received surgery at the same medical institution where ESD was performed, and six patients received surgery at different medical institutions. The mean time between ESD and surgery was 44 days. Two patients changed diagnosis (benign to malignant) after ESD. One patient underwent ESD and surgery during the same hospitalization period.
For further analysis, 472 patients who underwent ESD for only once were selected (Table 7) (C16, 202 patients; D00.2, 17 patients; D13.1, 220 patients; D13.9, one patient; other, 32 patients). In total, 70.0% of these pathologic examinations (329/472) were requested for histologic mapping (C5508). IHC studies were performed in 22.5% of ESDs (106/472). Approximately one-third of the gastric cancer specimens (66/202, 32.7%) and 15.0% of the gastric benign neoplasm specimens (33/220) were subject to IHC studies.
DISCUSSION
In this study, we examined nation-wide statistics regarding surgical pathologic examination. Considering sampling weight, we estimate that 5,440,288 (163,372×33.3) pathologic examinations were performed in Korea in 2013. We also surveyed pathologic examinations according to administrative district, requesting department, type of medical institutions, and patient conditions. These data will be useful for future planning and allocation of resources in the field of pathology and for the Korean Society of Pathologists.
There have been several reports regarding diagnostic discrepancies between endoscopic forceps biopsy and ESD, as well as between ESD and surgery. Recently, two large, single-center, retrospective studies revealed that 22.8% (465/2,041) and 31.7% (587/1,850) of cases changed diagnosis after endoscopic resection in Asan Medical Center (Seoul, Korea) and Samsung Medical Center (Seoul, Korea), respectively [5,6]. Our HIRA-NPS data revealed that only 10.9% of nation-wide cases experienced a change of diagnosis after ESD. HIRA-NPS data does not include detailed pathologic diagnosis information such as tumor size, tumor differentiations, dysplastic degrees, etc., so further analysis for clarifying such differences was limited. Shin et al. [7] reported that complete resection rates were not different according to absolute or expanded ESD indications, though their data were not HIRA data. Although HIRA-NPS data was not available for a sufficient number of ESD patients (509 ESDs in 490 patients) to allow for an accurate assessment, and only limited clinicopathological information was available, the problems associated with the relatively few number of patients can be overcome through further research using the raw HIRA data.
Histologic mapping of ESD specimens is recommended by The Gastrointestinal Pathology Study Group of the Korean Society of Pathologists [8]. However, 30.2% (143/472) of ESD specimens were not claimed as “C5508” (histologic mapping without lymph node dissection). Because precise histologic diagnosis of the ESD specimen is essential to treat patients, we suggest that nationwide surveys be conducted in order to assure quality of pathologic examination of ESD specimens. IHC staining was performed in 22.5% (106/472) of ESD cases. Unlike tissue immunofluorescent microscopic examinations or enzyme histochemistries, HIRA data does not list the specific antibodies used for IHC stains. Thus, further analysis of IHC studies using HIRA data was limited.
The main limitations of our analysis are statistical issues based on probability sampling. Our estimates were calculated from statistically extracted data from one year. Further analysis using HIRA raw data will be needed to decrease the statistical errors and bias and to evaluate changes over time. During our analysis, we experienced many challenges; therefore, we provide advice and guidance for other researchers who would like to analyze the HIRA database.
(1) It is essential to understand the framework of the HIRA database [9]. The HIRA data is intended for insurance claims and not for research. Detailed clinicopathological data are not provided. (2) Sample data are not appropriate for analyses requiring long-term follow-up. (3) Some claim codes have sub-codes (in most cases, additional charges by experts). (4) Disease codes and claims are not always accurate. (5) The analysis system should have at least 32 GB of main memory. (6) It is helpful to create relatively small data tables to decrease operation time. In the usual setting, R should use only one CPU core during calculation.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
References
Appendices
Appendix 1.
Numbers of medical institutions according to administrative districts
jptm-2016-03-04-app1.pdf