Quilty Lesions in the Endomyocardial Biopsies after Heart Transplantation
Article information
Abstract
Background
The aim of this study was to investigate the clinical significance of Quilty lesions in endomyocardial biopsies (EMBs) of cardiac transplantation patients.
Methods
A total of 1190 EMBs from 117 cardiac transplantation patients were evaluated histologically for Quilty lesions, acute cellular rejection, and antibody-mediated rejection. Cardiac allograft vasculopathy was diagnosed by computed tomography coronary angiography. Clinical information, including the patients’ survival was retrieved by a review of medical records.
Results
Eighty-eight patients (75.2%) were diagnosed with Quilty lesions, which were significantly associated with acute cellular rejection, but not with acute cellular rejection ≥ 2R or antibody-mediated rejection. In patient sdiagnosed with both Quilty lesions and acute cellular rejection, the time-to-onset of Quilty lesions from transplantation was longer than that of acute cellular rejections. We found a significant association between Quilty lesions and cardiac allograft vasculopathy. No significant relationship was found between Quilty lesions and the patients’ survival.
Conclusions
Quilty lesion may be an indicator of previous acute cellular rejection rather than a predictor for future acute cellular rejection.
Cardiac transplantation is a final therapeutic option for patients with end-stage heart failure. Approximately 4,000 cardiac transplantations are performed per year worldwide and the survival rate is approximately 81% at 1 year and 69% at 5 years [1]. The use of endomyocardial biopsies (EMBs) to monitor cardiac allograft rejection contributes to the excellent survival rates of cardiac transplantations. The diagnosis and grading of acute rejection are important for guiding the clinical management of heart recipients.
Along with acute rejection, other histologic findings have been observed in EMBs. One of these findings is nodular endocardial inflammatory infiltrates, which was termed Quilty lesion after the first patient in whom it was observed [2]. Quilty lesions may mimic acute cellular rejection when they extend into the myocardium [3,4]. Other than mimicking acute cellular rejection, the clinical implications of Quilty lesions are poorly understood and controversial.
The aim of this study was to investigate the clinical significance of Quilty lesions in cardiac transplant patients using a series of EMBs performed in a single institute. We analyzed the association of Quilty lesions with acute cellular rejection, antibodymediated rejection, cardiac allograft vasculopathy, and patient survival and graft loss.
MATERIALS AND METHODS
Case selection
This retrospective study protocol was approved with exemption of informed consents from patients by the Institutional Review Board of Samsung Medical Center, Seoul, Korea (IRB No. 2018-08-149). One hundred and fifty-six patients underwent cardiac transplantation between January 2007 and December 2015 at Samsung Medical Center. Patients were included in the study group when all of their hematoxylin and eosin (H&E)–stained EMB slides were available. Patients who survived for less than 30 days, had fewer than three EMBs, or had heart failure associated with cardiac malignancy were excluded. As such, 117 patients were included in this retrospective study. All patients received immunosuppression therapy with basiliximab, prednisolone, tacrolimus, cyclosporine A, and/or mycophenolate after cardiac transplantation. Patients with acute cellular rejection of grade 2R or greater according to the 2005 grading system of the International Society for Heart and Lung Transplantation (ISHLT) (grade 3 or greater according to the 1990 grading system of the ISHLT) were treated with steroid pulse therapy.
Endomyocardial biopsies
As a surveillance biopsy protocol, EMBs were obtained at 2, 4, 8, 12, 18, 24, 36, and 48 weeks following cardiac transplantation. Additional EMBs were obtained when acute rejection was clinically suspected. All H&E-stained EMB slides of the study patients were retrieved and evaluated histologically by a cardiovascular pathologist (J.-S.K.).
Diagnostic criteria of Quilty lesion, acute cellular rejection, antibody-mediated rejection, and coronary allograft vasculopathy
Quilty lesions are defined by dense endocardial inflammatory infiltrates. Patients with at least one EMB with Quilty lesions are classified as Quilty positive, while patients who had never had Quilty lesions in the series of EMBs are classified as Quilty negative. Quilty lesions are subclassified as Quilty A when they are confined to the endocardium and Quilty B when they extend into the myocardium. Quilty-positive patients are further subdivided into Quilty B positive when they have at least one Quilty B lesion and Quilty A positive when they have never shown Quilty B lesions.
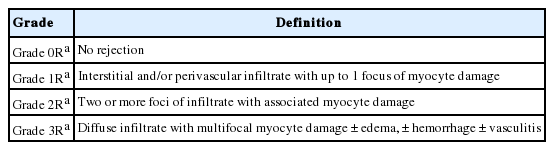
The diagnosis and histologic grading of acute cellular rejection were performed using the 2005 ISHLT criteria (Table 1, Fig. 1) [5]. Antibody-mediated rejection was defined by intravascular macrophages and endothelial cell damage, confirmed by immunostaining against C4d (1:50, polyclonal, Cell Marque, Rocklin, CA, USA) and CD68 (1:1,000, clone KP1, Dako, Glostrup, Denmark) (Fig. 2).
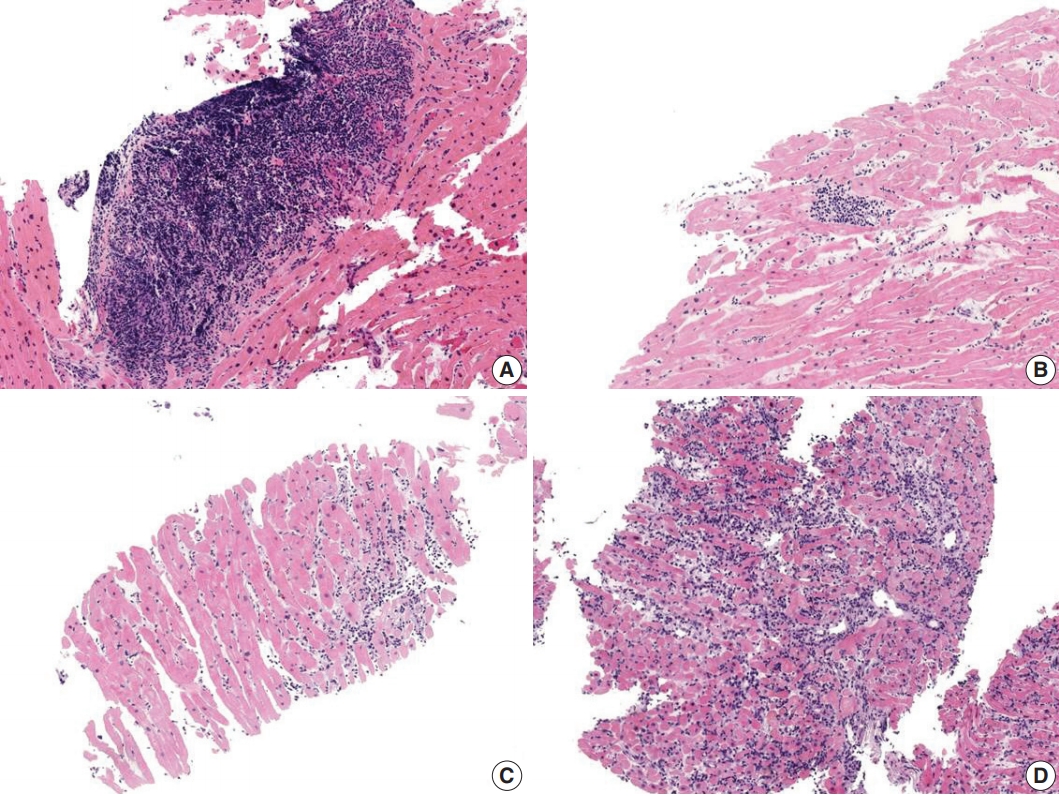
Quilty lesion and acute cellular rejection. (A) Quilty lesion. (B) Grade 1R. (C) Grade 2R. (D) Grade 3R.
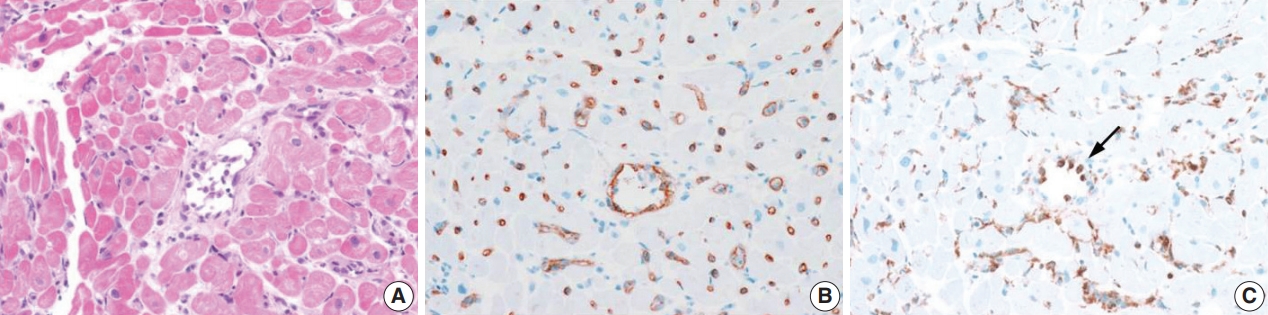
Antibody-mediated rejection. (A) Swollen endothelial cells and intravascular mononuclear cells. (B) Multifocal C4d staining in capillary endothelial cells. (C) CD 68 staining in intravascular macrophages (arrow).
The coronary arteries of transplantation patients were evaluated using coronary angiography at 4 weeks from transplantation and with computed tomography coronary angiography annually following transplantation. Any stenosis of the coronary artery of > 30% was considered cardiac allograft vasculopathy. Stenosis of coronary artery that required either intervention or retransplantation was considered significantly severe cardiac allograft vasculopathy.
Statistics
The IBM SPSS Statistics software package (ver. 24.0, IBM Corp., Armonk, NY, USA) was used for all statistical analyses, and a p-value of < .05 was considered statistically significant. The associations between Quilty lesions and acute cellular rejection or cardiac allograft vasculopathy were evaluated with chisquare test or Fisher exact test.
For patients with both Quilty lesions and acute cellular rejection, the time-to-onset from transplantation to Quilty lesions and acute cellular rejection was calculated by subtracting the date of transplantation from the date when Quilty lesions or acute cellular rejection were diagnosed for the first time, respectively. A paired T-test was used for comparison. The association between Quilty lesions and transplantation failure was evaluated using Kaplan-Meier estimation and assessed using the log-rank test. The clinical variables including the presence of Quilty lesion were evaluated by univariate and multivariate analyses of disease-free survival with Cox proportional hazards model. The composite end-points were graft loss and mortality of any causes.
RESULTS
Transplant recipients
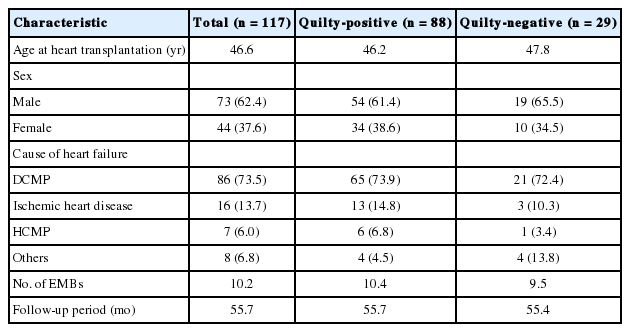
The study population consisted of 73 (62.4%) males and 44 (37.6%) females. The mean age at cardiac transplantation was 46 ± 16 years. The most common cause of heart failure was dilated cardiomyopathy (73.5%), followed by ischemic heart disease (13.7%), and hypertrophic cardiomyopathy (5.8%). The mean follow-up period for all patients was 58 months. A total of 1190 EMBs were collected from 117 patients, and the average number of EMBs per patient was 10.2 ± 0.2 (Table 2).
Quilty lesions in EMBs
Quilty lesions were found in 88 (75.2%) patients, and the average number of the EMBs with Quilty lesions in these patients was 2.8 ± 0.2. The number of EMBs with Quilty lesions for each biopsy order was shown in Fig. 3. The number of EMBs with Quilty lesions had a tendency to increase as the biopsy order increases. There were no significant differences in the age (46.2 ± 16.6 years vs 47.8 ± 14.3 years) or sex (53 males/35 females vs 17 males/12 females) between Quilty-positive and Quilty-negative patients (Table 2).

Then number of Quilty-positive endomyocardial biopsies (EMBs) for each biopsy order. The number of Quilty-positive EMBs increases as biopsy order increases.
Quilty A–positive patients and Quilty B–positive patients showed no significant differences in clinical outcomes, which concur with the previous report (Supplemental Table S1) [2]. As such, we decided not to subdivide Quilty-positive patients for further analyses.
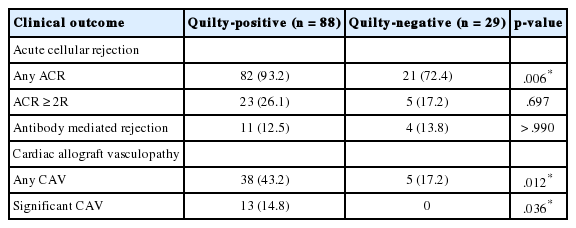
Quilty lesions and acute cellular rejection
Of the 117 patients, 103 (88.0%) were diagnosed with acute cellular rejection in at least one of the series of EMBs and among them, 28 (23.9%) patients were diagnosed with acute cellular rejection of ISHLT grade 2R or higher. In the series of EMBs, Quilty-positive patients were more likely to be diagnosed with acute cellular rejections than Quilty-negative patients, and the difference was significant (p=.006). However, there was no significant association between Quilty lesions and acute cellular rejection of ISHLT grade 2R or higher (p = .697) (Table 3).
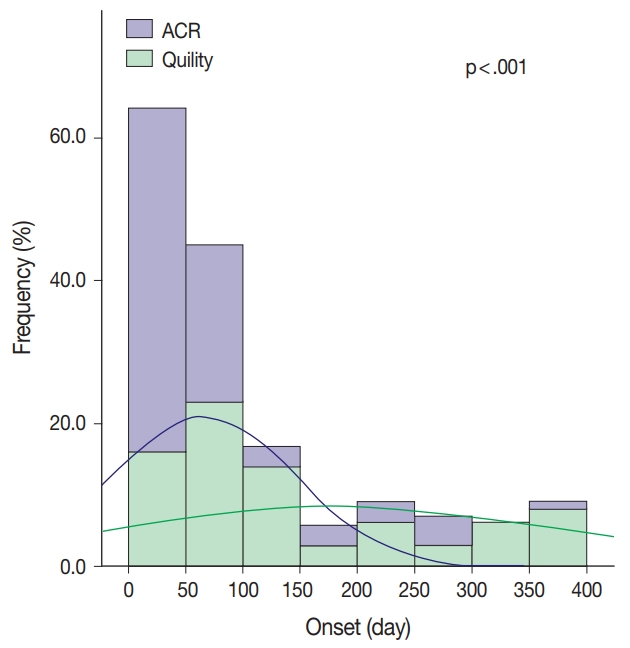
When comparing the time-to-onset of Quilty lesions and acute cellular rejection during the post-transplantation follow-up period, the time-to-onset of Quilty lesions was significantly longer than that of acute cellular rejection (179.2 days vs 65.5 days, p < .001) (Fig. 4).
Quilty lesions and antibody-mediated rejection
Of the 117 patients, 15 (12.8%) showed at least one episode of antibody-mediated rejection in the series of EMBs. Among the 15 patients with antibody-mediated rejection, 11 were Quilty positive while four were Quilty negative. There was no statistically significant association between Quilty lesions and antibody-mediated rejection (Table 3).
Quilty lesions and cardiac allograft vasculopathy
Of the 117 patients, 43 (36.8%) developed cardiac allograft vasculopathy detected by coronary angiography, from as early as 4 weeks to 71 months after transplantation. Among them, 13 patients showed significantly severe cardiac allograft vasculopathy that required treatment: seven underwent percutaneous coronary intervention (PCI) or balloon dilatation, five suffered graft loss and underwent retransplantation, and one underwent retransplantation after PCI. There was a significant correlation between the presence of Quilty lesions and cardiac allograft vasculopathy (p = .012) (Table 3). In addition, a significant correlation was found between the presence of Quilty lesions and significantly severe cardiac allograft vasculopathy requiring either intervention or retransplantation (p = .036) (Table 3).
Quilty lesions and transplantation failure
A Kaplan–Meier analysis was performed for all-cause transplant failure (mortality and graft loss) according to the presence of Quilty lesions (Fig. 5). Median disease-free survival time was 109.5 months for Quilty-positive patients and 96.4 months for Quilty-negative patients, but this difference was not significant (p = .990). No significant difference in survival was observed between Quilty-positive and Quilty-negative groups in multivariate Cox regression analysis, either. The presence of antibody mediated rejection was the only independent factor of disease-free survival in multivariate Cox regression analysis (Table 4).
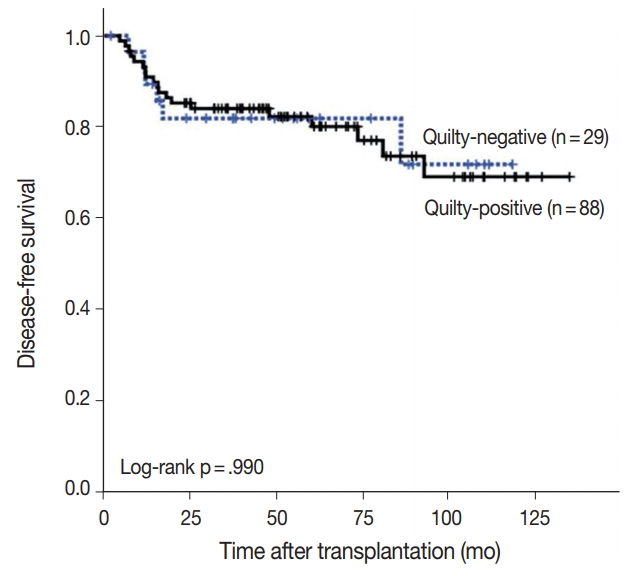
Kaplan-Meier analysis for disease-free survival (death, graft loss) in Quilty-positive and Quilty-negative patients. The difference in survival between Quilty-positive and Quilty-negative is not significant.
DISCUSSION
Quilty lesions in EMBs appear as focal flat to nodular, densely cellular endocardial infiltrates composed mainly of lymphocytes with histiocytes, dendritic cells and occasional plasma cells with a high proportion of T lymphocytes [3,6,7]. Some Quilty lesions appear as extensive inflammatory infiltrates with an extension to the myocardium, and often misinterpreted as high grade acute cellular rejections. Quilty lesions have been reported to occur in 10% to 20% of EMBs and 58% to 74% of cardiac transplantation patients [8,9]. Although Quilty lesions are frequently reported in EMBs and many studies have been conducted on Quilty lesions, the relationship between Quilty lesions and clinical outcomes remains unclear.
Quilty lesions have been reported to be associated with acute cellular rejection and are claimed to signal acute cellular rejection episodes in future EMBs [8-12], while other studies have suggested that there is no significant association between Quilty lesions and acute cellular rejection [2,6,13]. In our study, patients with Quilty lesions showed a significantly higher incidence of acute cellular rejection, which agrees with some of previous studies [8-12], but no significant association with grade 2R or higher acute cellular rejection, which required additional treatment. When we evaluated time-to-onset from transplantation to EMBs with Quilty lesions and acute cellular rejection, we found that Quilty lesions had a significantly longer time-to-onset than acute cellular rejection. This may suggest that Quilty lesion is an indicator of previous acute cellular rejection rather than a predictor of future acute cellular rejections.
We observed a significant correlation between Quilty lesions and cardiac allograft vasculopathy in the graft. Cardiac allograft vasculopathy is a long-term complication after heart transplantation to cause myocardial ischemic injury and graft loss. Histologically, cardiac allograft vasculopathy appears as concentric intimal hyperplasia of the coronary arteries and diffusely involves the coronary arteries, from epicardial arteries to small intramyocardial branches but the native vessels of recipients are spared [14]. The pathogenesis of cardiac allograft vasculopathy is not fully understood. However, the sparing of native vessels suggests an immune mechanism targeting the allograft [15]. Hiemann et al. [16] suggested that Quilty lesions might be associated with endothelial disease, which could lead to graft failure. Yamani et al. [17] observed the expression of the vitronectin receptor (αvβ3) in Quilty lesions and suggested that the vitronectin receptor may be the link between Quilty lesions and transplant vasculopathy, since vitronectin receptor involves endothelial cell migration and vascular smooth muscle cell proliferation induced by growth factors and cytokines. Our result on the association between Quilty lesions and cardiac allograft vasculopathy in the graft was supported by the studies of Hiemann et al. [16] and Yamani et al. [17]
Szymanska et al. [18] reported a significantly higher incidence of Quilty lesions in the EMBs of patients with C4d capillary depositions (antibody-mediated rejection). Cano et al. [19] reported a significant association between Quilty lesions and endocardial C4d deposition in patients without evidence of rejection and suggested association between Quilty lesions and complement activation. We observed no significant association between Quilty lesions and antibody-mediated rejection, in contrast with the previous study by Szymanska et al. [18] This result might be related to the smaller population in our study and the difference in the prevalence of antibody-mediated rejection: the prevalence of antibody-mediated rejection in our study (16/117, 13.7%) was higher than that in the Szymanska’s study (16/212, 7.5%). Further validation in larger groups is desired since there are few reports on the relationship between Quilty lesions and antibodymediated rejection.
The major causes of mortality after cardiac transplantation are early graft failure, allograft rejection, and infection in the first 3 years following transplantation and cardiac allograft vasculopathy, malignancy, and renal failure after 5 years from transplantation [1]. A long list of risk factors such as increasing donor and recipient age, long cold ischemic time, congenital heart disease, history of dialysis and transfusions, prior transplantation are reported to be significantly associated with cardiac transplantation patient survival [1]. Quilty lesions have been reported to be associated with poor survival rates [16,20], while other studies have reported that Quilty lesions were associated with improved survival [10] or had no significant association with survival [2]. In our study, there was no significant difference in the median survival time between Quilty-positive patients and Quilty-negative patients, in spite of the association of Quilty lesions with cardiac allograft vasculopathy and acute cellular rejection. It also supports that Quilty lesion is an indicator of previous acute cellular rejection rather than a meaningful risk factor for patients’ survival.
There are some limitations of our study. (1) The total number of the patients was relatively small and their follow-up was rather short. (2) Evaluation of acute cellular rejection and Quilty lesions was based on the biopsy specimen instead of the whole heart. We evaluated at least three fragments of tissue for each EMB, but there is still the possibility of false negativity for the lesions. (3) The frequency of acute cellular rejection was rather high (88%). However, that of acute cellular rejection ≥ 2R was 24%, which was comparable to that 28% of recipients experienced at least 1 episode of treated acute rejection during follow-up between 2004 and June 2016, according to 2017 ISHLT reports [21].
Our study is the first to describe the significance of Quilty lesions among cardiac transplantation patients in Korea. Our results suggest that Quilty lesion is in fact an indicator of previous acute cellular rejection and has a correlation with cardiac allograft vasculopathy. Further studies employing longer follow-up periods and/or more data from multiple centers are required, and additional studies on pathogenesis would be helpful to understand the biological significance of Quilty lesions.
Electronic Supplementary Material
Supplementary materials are available at Journal of Pathology and Translational Medicine (http://jpatholtm.org).
Notes
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.