Thyroid fine-needle aspiration cytology in Taiwan: a nationwide survey and literature update
Article information
Abstract
In Taiwan, thyroid fine-needle aspiration cytology is easily accessible and reliable for evaluating thyroid nodules. The sonographic pattern plays a major role and is the deciding factor for aspiration. We conducted a nationwide survey in 2017 and it revealed that 31% of laboratories had adopted The Bethesda System for Reporting Thyroid Cytopathology. There was a relatively high unsatisfactory rate (24.04%) and low rates of indeterminate diagnoses, including atypia of undetermined significance/follicular lesions of undetermined significance: 4.87%, and follicular neoplasm/suspicious for a follicular neoplasm: 0.35%. Moreover, the risks of malignancy in benign, atypia of undetermined significance, and suspicious for a follicular neoplasm were relatively high. These may reflect strict diagnostic criteria for indeterminate categories and better patient selection for surgery. Improvements in specimen sampling and continuing education programs are crucial. Newly-developed thyroid cytology technologies, such as immunocytochemistry, molecular testing, and computerized cytomorphometry, may further facilitate cytology diagnoses.
Fine-needle aspiration (FNA) is minimally invasive and widely used for assessing thyroid nodules [1]. It is also a decisive procedure for evaluating thyroid nodules that require surgery or conservative management [2,3]. Although the Bethesda System is the most widely accepted diagnostic system for thyroid cytology, there are significant deviations in practices in different countries [4,5]. Our previous review summarized the history and the evolution of the thyroid FNA practice in Taiwan [6]. The aims of this article are to provide an overview of the current thyroid FNA practice in Taiwan, particularly data from our nationwide survey, describe the changes due to the new World Health Organization (WHO) classification, and the advances of novel technologies.
CURRENT THYROID CYTOPATHOLOGY IN TAIWAN
In Taiwan, the majority of thyroid FNA cases are now performed with ultrasound guidance, since ultrasound-guided FNA provides better sampling of smaller or multiple nodules compared to palpation-guided FNA. High-resolution neck ultrasonography provides a simple, real-time, and noninvasive method to assess thyroid nodules. The accuracy of neck ultrasonography in distinguishing malignant thyroid nodules was up to 86.8%, secondary to that of ultrasound-guided FNA (90.8%) [7]. The prevalence of thyroid abnormalities detected by ultrasonography in Taiwanese adults without palpable thyroid nodules was 18.5%, which were mostly cysts and small nodules [8]. Several published reports proposed sonographic criteria to prevent unnecessary ultrasound-guided FNA or further surgeries [9-11]. Analyzing data from Taiwan’s National Health Insurance Research Database from 2004–2010, Lee et al. [12] reported that age-standardized rates of palpation-guided thyroid FNA and ultrasound-guided thyroid FNA increased by 10.9% and 349.3%, respectively. There was also a 94.8% increase in the age-standardized annual incidence rate of thyroid cancer. This is likely attributable to the widespread use of medical ultrasound for thyroid nodule evaluation. Despite the increasing trend of thyroid cancers, the mortality associated with thyroid cancer remains almost unchanged.
In regard to the cytology preparation and staining, the conventional smear for both Papanicolaou (on alcohol-fixed slides) and Liu’s stain (on air-dried slides) are the most common methods for thyroid FNA cytology in Taiwan [6]. Although liquid-based cytology (LBC) is not currently prevalent, it has become increasingly popular due to easier specimen collection and transportation, standardized preparation, and reduction of various obscuring factors and artefacts [6,13]. Additionally, LBC provides specimens for further ancillary techniques, such as immunocytochemistry and molecular testing.
The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) is widely accepted for standardized terminology and better consistencies among cytopathologists and clinicians [14]. The six diagnostic categories are: unsatisfactory/nondiagnostic (US/ND), benign, atypia of undetermined significance/follicular lesion of undetermined significance (AUS/FLUS), follicular neoplasm/suspicious for a follicular neoplasm (FN/SFN), suspicious for malignancy (SM), and malignant. Before TBSRTC, investigators in Taiwan used different diagnostic categories for thyroid FNA reporting [6,15].
In 2017, the Taiwan Society of Clinical Cytology performed the first nationwide survey to evaluate the general practice of thyroid cytopathology, application of the reporting system, and risk of malignancy (ROM). The questionnaires were sent to 119 cytology laboratories at medical centers, regional hospitals, and private clinical laboratories. Participants were asked seven questions as follows: (1) How many doctors are there signing out thyroid cytology reports?, (2) What are their subspecialties?, (3) How many cytotechnologists are there screening thyroid cytology?, (4) What were your annual thyroid cytology case numbers in 2015?, (5) What kind of reporting system is used in your laboratory for reporting thyroid cytology?, (6) Please provide your annual cases number, biopsy rate, and malignancy rate on follow-up for each diagnostic category, and (7) What are your cytology preparation methods for thyroid cytology in your laboratory? Fifty-five effective questionnaires (46%) were collected after a one-month answering period.
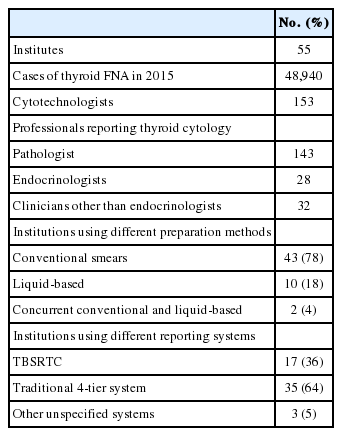
These responses from laboratories represented a total of 48,940 thyroid FNA cases annually in the year of 2015, and there were 143 pathologists, 28 endocrinologists, and 32 clinicians other than endocrinologists signing out thyroid cytology reports and 153 cytotechnologists screening thyroid cytology slides on a routine basis. As for the cytology preparation method, 78% of the laboratories used conventional smears, 18% used LBC, and 4% used concurrent conventional smears and LBC. For the reporting system, 64% of laboratories applied the traditional 4-tier system (negative, atypical, suspicious, and positive for malignancy), 31% adopted the TBSRTC, and 5% used other unspecified diagnostic systems (Table 1).
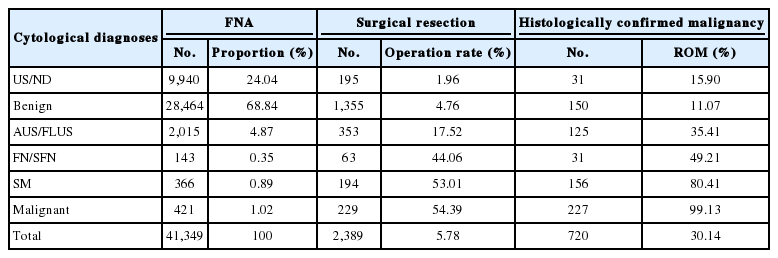
A total of 41,349 FNA cases could be converted to each corresponding TBSRTC diagnostic category. The rate of diagnosis, surgical resection, and malignancy for each category were as follows: US/ND: 24.04%, 1.96%, 15.9%; benign: 68.84%, 4.76%, 11.07; AUS/FLUS: 4.87%, 17.52%, 35.41%; FN/SFN: 0.35%, 44.06%, 49.21%; SM: 0.89%, 53.01%, 80.41%; malignant: 1.02%, 54.39%, 99.13% (Table 2). The nationwide survey demonstrated a high unsatisfactory rate (24.04%) and low rates of indeterminate diagnoses (AUS/FLUS, 4.87%; FN/SFN, 0.35%) for thyroid FNA cytology in Taiwan. The high unsatisfactory rate might be attributable to the routine submission of the fluid from symptomatic hemorrhagic cysts for cytologic examination in our clinical practice. Therefore, a different diagnostic approach for the specimen with cystic fluid only should be considered, such as in the Japanese system, to reduce the unsatisfactory rate. The low rates of indeterminate diagnoses reflected the application of relatively strict criteria for using these categories to avoid clinical uncertainty in the overall management. Moreover, compared to the Western experience [16], the ROM in benign, AUS/FLUS, and FN/SFN in this survey was higher and the resection rate for these nodules were lower. These results suggested a more conservative approach and the application of other clinicoradiological parameters to select eligible patients for surgeries in our clinical practice. Nevertheless, the general characteristics of the thyroid FNA in Taiwan, including fewer malignant FNAs and lower ROMs of all resected nodules, were also different from other Asian countries [16] and deviated more towards the results for Western countries. This implies that the guidelines from Western countries were more closely followed by our clinicians. The major limitation of the present survey was that the data was derived from the questionnaire and there might be some bias regarding the evaluation of the incidence and malignancy rate.
IMPACT OF NONINVASIVE FOLLICULAR THYROID NEOPLASM WITH PAPILLARY-LIKE NUCLEAR FEATURES
In 2016, the new terminology of noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) was been proposed to replace the noninvasive encapsulated follicular variant of papillary thyroid carcinoma (PTC) [17] and this has been further adopted by the 2017 World Health Organization Classification of Tumors of Endocrine Organs [18]. The change in tumor classification inevitably influences the preoperative thyroid FNA diagnosis [19] and the utilization of molecular testing [20]. However, an international multi-institutional study from India, Japan, South Korea, Taiwan, and Thailand revealed a less significant impact of NIFTP reclassification on the practice of thyroid cytopathology [21]. In Taiwan, NIFTP cases constituted only 2.9% of excised thyroid nodules and 5.3% of all malignancies, and most NIFTP cases (66.1%) were interpreted as indeterminate FNA categories (FN/SFN, 32.2%; AUS/FLUS, 22.0%). The differences in the ROM before and after NIFTP reclassification were not statistically significant for all the diagnostic categories.
IMMUNOCYTOCHEMISTRY, MOLECULAR TESTING, AND COMPUTERIZED CYTOMORPHOMETRY
In thyroid FNA, immunocytochemistry had been implemented to differentiate nonfollicular lesions from thyroid follicular lesions [22-24]. Immunocytochemistry may improve the cytologic diagnostic accuracy, but does not have a consistent predictive value for malignancy [24]. For immunocytochemistry, a cell block is usually preferable compared with cytologic specimens, however, thyroid FNA materials might be limited for cell block preparation.
The first report on molecular testing in thyroid FNA from Taiwan can be traced back to 2003. Liou et al. [25] found that human telomerase reverse transcriptase (TERT) gene expression was more prevalent in malignant thyroid FNA samples than in the benign thyroid FNA samples and proposed that it is an adjunctive molecular marker for the preoperative diagnosis of thyroid malignancies. The need for distinguishing benign thyroid lesions from thyroid cancers in thyroid FNA has led to the investigation of differentiating molecular markers. To date, more sophisticated molecular tests for thyroid FNA are commercially available, such as the ThyroSeq, Afirma, RosettaGX Reveal, ThyGenX, and ThyraMIR [26]. These molecular tests have high negative predictive values that range from 92% to 97% and lower positive predictive values that range from 37% to 83% for indeterminate thyroid nodules; therefore, these are more ideal as “rule out” tests. However, these tests are rarely applied in Taiwan due to the high costs.
The application of computerized cytomorphometry had been used as an emerging alternative test to stratify risks in thyroid nodules with indeterminate FNA results in Taiwan [27,28]. Computerized cytomorphometry, serving as a sequential reader, analyzes objective quantification of selected morphologic and chromatic parameters in individual cells on cytology slides [28]. For example, using computerized cytomorphometry, the nucleus-cell ratio and variation of the nuclear area showed significantly positive correlations with PTC recurrence and could be predictors of recurrence [28]. With 100% sensitivity, the computerized quantification of cytological characteristics could assist in differentiating 17.6% of AUS/FLUS, 13.6% of FN/SFN, and 33.3% of SM cases as benign rather than malignant, avoiding unnecessary thyroidectomy [29]. The cytological features used in this computerized method included the mean nuclear size, mean nuclear elongation, nuclear-to-cytoplasmic saturation ratio, nuclear-to-cytoplasmic ratio, nuclear polarity, and inclusion index. A larger nuclear size and higher nuclear-to-cytoplasmic ratio were related to malignancy. This computerized method was developed to assist cytopathologists and clinicians in cases of indeterminate thyroid cytology. The limitation of this technology is that it was developed solely for evaluating nuclear features of PTC and was not useful for differentiating other follicular-patterned neoplasms, particularly borderline tumors such as NIFTP and well-differentiated tumor/follicular tumors of uncertain malignant potential.
FINE-NEEDLE ASPIRATION CYTOLOGY AND INTRA-OPERATIVE FROZEN SECTIONS FOR THYROID SURGERY
Traditionally, intra-operative frozen section was largely applied to confirm the cytological interpretation and to identify malignancy in patients with indeterminate or unsatisfactory cytological diagnoses in Taiwan [1]. Currently, most endocrine surgeons still prefer frozen sections as an intra-operative guide for thyroid surgery to reduce unnecessary extensive surgery or the chance of repeated operations. Intra-operative frozen sections provide valuable information, especially in rare cancers [29,30].
However, it is extremely difficult to diagnose follicular thyroid carcinoma (FTC) either by using FNA or intra-operative frozen section. In a retrospective study of 22,134 FNA cases, only 23 cases (46%) were intra-operatively diagnosed as malignant by frozen section among 50 cases of FTC, and 13 cases (26%) were intra-operatively diagnosed as benign nodules (nodule hyperplasia and adenoma) [31]. Similarly, Hürthle cell carcinoma (HTC) is difficult to diagnose by intra-operative frozen section. Lee et al. [32] reported that 60% of surgical cases with HTC were designated as malignancies based on frozen sections. A meta-analysis for Hürthle cell lesions in thyroid FNA in nine institutions from six Asian countries revealed that there was interinstitutional variation in the cytologic interpretation of Hürthle cell morphology and in Bethesda categorization [33]. Hürthle cell-rich aspirates were most frequently categorized as AUS/FLUS, followed by FN/SFN. Only 13% of Hürthle cell-rich lesions were actually malignant. Clinical risk factors, such as age less than 20 years and history of autoimmune thyroid disease might be parameters for selecting patients for observation or surgery, since the frozen section approach was valuable in deciding the extent of thyroidectomy in patients with follicular and Hürthle cell neoplasms [32].
CONCLUSION
Thyroid FNA cytology is a cost-effective and reliable method for evaluating thyroid nodules in Taiwan, and is typically performed under ultrasound guidance. The sonographic pattern plays a major role and is the deciding factor for aspiration. Even with the recent coronavirus disease 2019 (COVID-19) pandemic, the procedures and preparations are performed according to national and institutional laboratory biosafety guidance [34,35]. Although most laboratories performed conventional smears, 22% of institutions had applied LBC in thyroid cytology. For the reporting system, 64% of laboratories followed the traditional 4-tier system, and 31% had adopted the TBSRTC. In general, the cytopathology laboratories in Taiwan are in transition and plan to gradually accept TBSRTC to allow easy and reliable data sharing for national and international collaboration and comparison. Newly-developed thyroid cytology technologies, such as immunocytochemistry, molecular tests, and computerized cytomorphometry, may further facilitate cytology diagnoses. Finally, intra-operative frozen consultation may serve as a complementary test, except for patients with follicular and Hürthle cell neoplasms.
Notes
Ethics Statement
Not applicable.
Author contributions
Conceptualization: CCC, JFH, CRL. Data curation: CCC, JFH, CYL. Formal analysis: CCC, JFH. Investigation: CCC, JFH, CYL, YHW. Methodology: CCC, JFH. Supervision: CRL. Validation: CCC, JFH. Writing—original draft: CCC. Writing—review & editing: JFH, YHW. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.