Development of quality assurance program for digital pathology by the Korean Society of Pathologists
Article information
Abstract
Background
Digital pathology (DP) using whole slide imaging is a recently emerging game changer technology that can fundamentally change the way of working in pathology. The Digital Pathology Study Group (DPSG) of the Korean Society of Pathologists (KSP) published a consensus report on the recommendations for pathologic practice using DP. Accordingly, the need for the development and implementation of a quality assurance program (QAP) for DP has been raised.
Methods
To provide a standard baseline reference for internal and external QAP for DP, the members of the Committee of Quality Assurance of the KSP developed a checklist for the Redbook and a QAP trial for DP based on the prior DPSG consensus report. Four leading institutes participated in the QAP trial in the first year, and we gathered feedback from these institutes afterwards.
Results
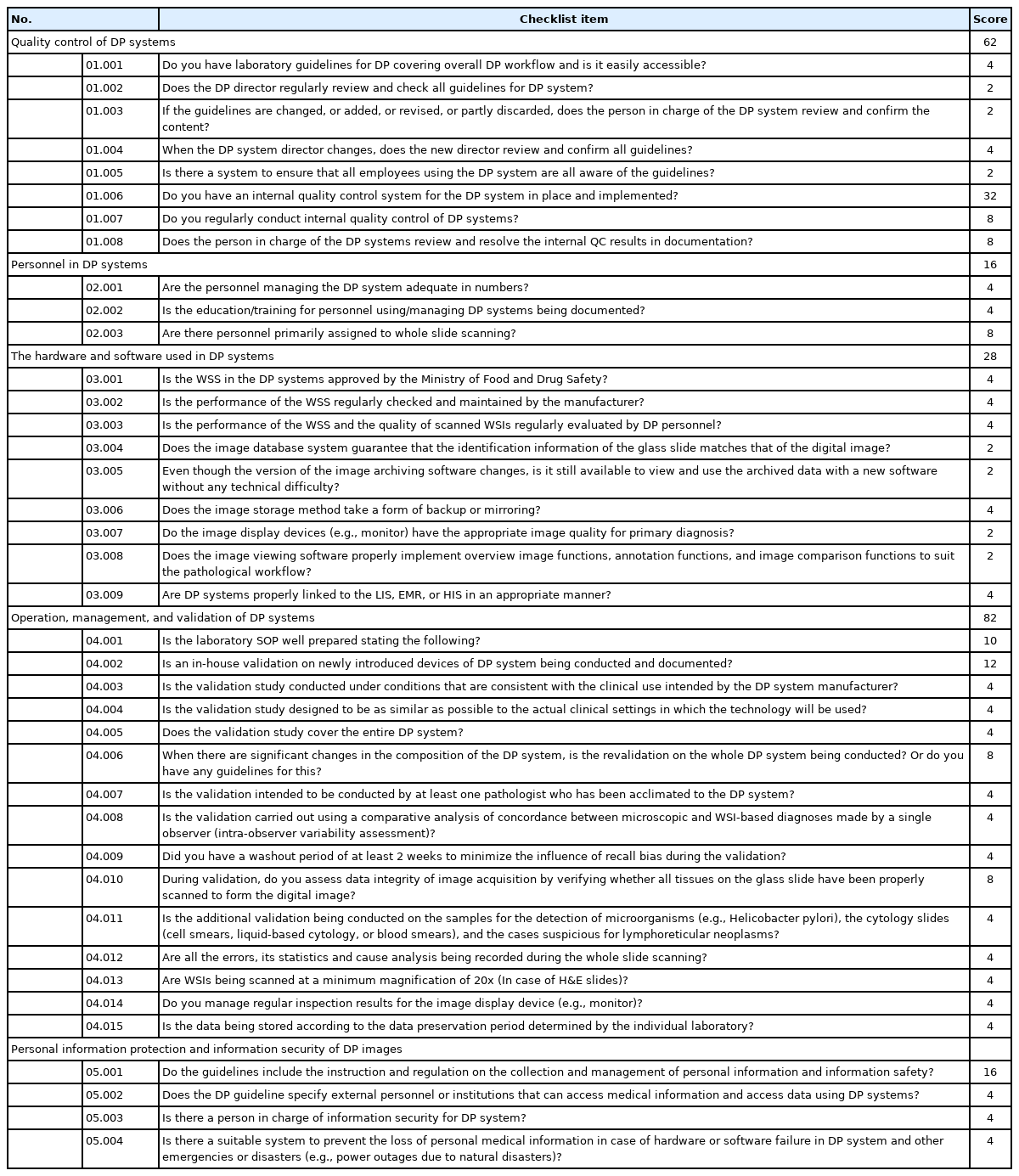
The newly developed checklists of QAP for DP contain 39 items (216 score): eight items for quality control of DP systems; three for DP personnel; nine for hardware and software requirements for DP systems; 15 for validation, operation, and management of DP systems; and four for data security and personal information protection. Most participants in the QAP trial replied that continuous education on unfamiliar terminology and more practical experience is demanding.
Conclusions
The QAP for DP is essential for the safe implementation of DP in pathologic practice. Each laboratory should prepare an institutional QAP according to this checklist, and consecutive revision of the checklist with feedback from the QAP trial for DP needs to follow.
Digital transformation using digital pathology (DP) is currently a hot topic in pathology because it has served as a new platform for a way of making pathologic diagnosis, consultation, interdisciplinary conference, and education [1,2]. Whole slide imaging (WSI) technology is at the center of these fundamental changes, and quality assurance of WSI is essential to guarantee the safety of DP practice. In 2020, the Korean Society of Pathologists (KSP), especially members of the Digital Pathology Study Group (DPSG), formerly known as the Medical Informatics Study Group, published a consensus paper on the recommendation for pathologic practice using DP [2]. The DPSG prepared a consensus recommendation based on all previously published international guidelines and recommendations on DP, including those by the US Digital Pathology Association, College of American Pathologists, UK British Royal College of Pathologists, Canadian Association of Pathologists, Royal College of Pathologists of Australia, Federal Association of German Pathologists, Japanese Society of Pathology, and Spanish Society of Anatomic Pathology [3-10]. Consecutively, there were the Assessment and Approval Guideline on Artificial Intelligence (AI)-based Histopathologic In-vitro Diagnostic Devices (software) from the Ministry of Food and Drug Safety of Korea and the Reimbursement Assessment Guideline of Innovative Medical Technology (Pathology AI-based technology) from the Health Insurance Review and Assessment Service in 2021 [11,12].
According to the safety of DP implementation in daily routine practice, there has been accumulated evidence of comparable concordance between DP-based and conventional microscopic diagnosis in various sample types [13-15]. However, quality assurance program (QAP) (in-house validation) during DP implementation, continuous quality control (QC) activities including pre- and post-scan QCs are essential for guaranteeing the quality of pathologic practice in each laboratory [16]. The consensus recommendation report by the KSP includes the general principles and various consideration embracing not only basic system requirements but every QC activity [2]. However, the preparation of institutional QAP and laboratory checklists, and practical application of guidelines in each laboratory environment are not easy to implement. With this context, the Committee of Quality Assurance (CQA) of the KSP decided to develop QAP checklists for DP and plan external QAP trial to guide member institutes that implemented or are planning to implement DP.
In this report, we present a practical checklist that can be a baseline reference for each pathologic laboratory to prepare internal guidelines for DP QAP, and the results of DP QAP trial that was performed in four leading hospitals with DP systems in Korea along with their feedback.
MATERIALS AND METHODS
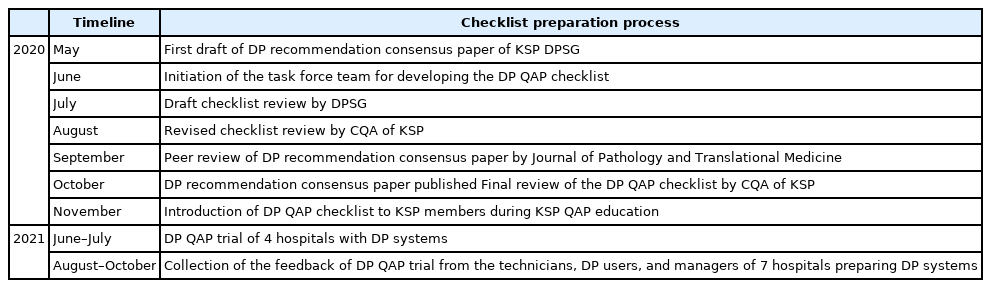
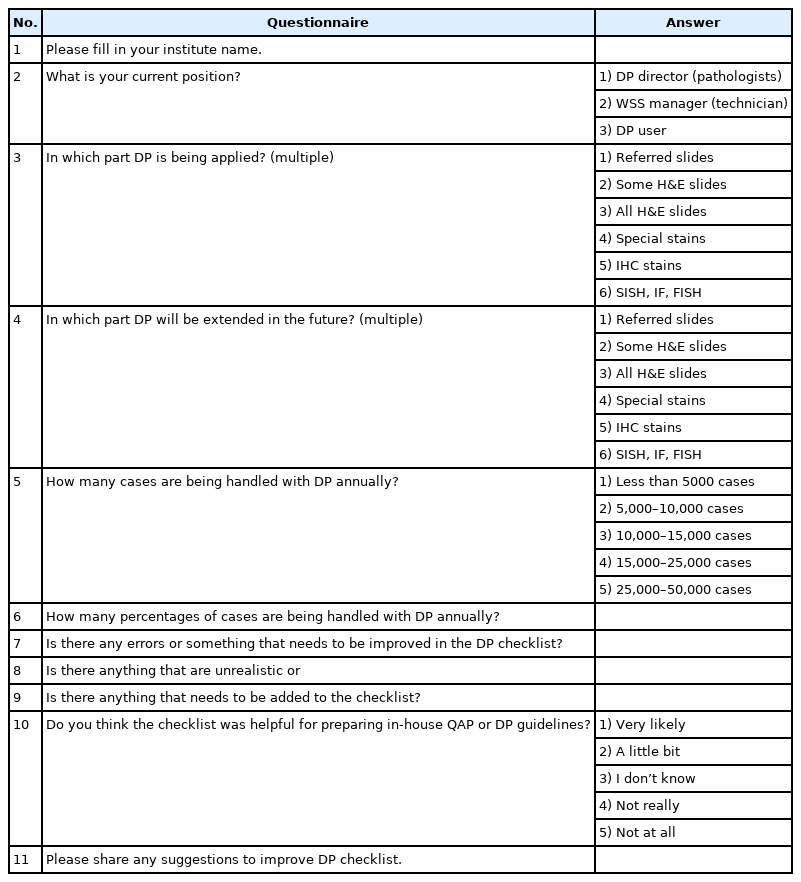
Since the draft of the consensus recommendation paper by the KSP DPSG was prepared in May 2020, the CQA of the KSP initiated the task force team to develop a checklist for DP QAP (YC, JMB, DWK, and HSH) (Table 1). The draft checklist consisted of 39 items (216 score) to check: eight items for QC of DP systems; three items for DP personnel; nine items for hardware and software requirements for DP systems; 15 items for validation, operation, and management of DP systems; and four items for data security and personal information protection (Tables 2, 3). After the preparation of a draft checklist, it was serially reviewed by the DPSG and the members of the CQA. As the consensus recommendation paper was published in October 2020, the final version of the DP QAP checklist was prepared after final revision by the CQA. After the introduction of the checklist to the members of the KSP, the first QAP trial for DP was performed the following year, 2021. Unfortunately, because of the coronavirus disease 2019 (COVID-19) pandemic, the QAP trial could be conducted online in four leading hospitals with DP systems without on-site inspection. After the QAP trial, feedback from technicians, DP users, and DP managers of the hospitals preparing DP implementation was collected (Table 4).
RESULTS
Checklist for DP quality assurance program
Preface
• This checklist was developed based on the ‘Recommendations for Pathologic Practice Using Digital Pathology: Consensus Report of the Korean Society of Pathologists’ (2020.10) [2]. It is highly recommended to refer to the recommendations for understanding the background information related to DP (Supplementary Table S1).
• “DP” used in this checklist for DP QAP refers to a relatively narrow perspective of DP, that is primary diagnosis or consultation using WSIs via displays such as monitors instead of a microscope, by digitalizing all or a part of pathological samples. The DP QAP of the KSP is intended only for institutions conducting primary diagnoses using DP systems.
• “DP” is a dynamic imaging environment (or academic field related to this environment) that involves the acquisition and management of pathologic information, by converting microscopic glass slides into digital files, and the pathologic diagnosis and interpretation of those images using display devices (e.g., monitors). The scope of the application includes education, diagnosis, research, image analysis, archiving, retrieval, expert consultations, and data sharing. In this checklist, its meaning is limited to the primary diagnosis or consultation as part of the pathologic diagnosis process.
• “The digital pathology system” is a computer system that enables the collection, management, and interpretation of pathologic image data by digitalizing glass slides. It includes a whole slide scanner (WSS), computer workstation, operating and managing software (scanner operation software, image viewer, and image analysis software), and network system (server and network environment).
• “Telepathology” is a digital or real-time pathologic image communication environment using wired or wireless networks or a related academic field. Telepathology could be used either for consultation with specialists in a distant location or for the diagnosis of samples in a remote facility.
• “Whole slide image/imaging (WSI)” is a single high-resolution image file or associated technology scanned from a single glass slide using a WSS. WSI can be considered a high-resolution copy or mirrored image of a glass slide.
• “Focus stacking (Z-stacking)” is an image-processing technique that displays multilayer digital images acquired at varying focus levels to obtain a much greater depth of field. In samples with many 3-dimensional microstructures and cell clusters, such as cytology slides, it is difficult to obtain the appropriate depth of field with a single focus. Multiple images at slightly different levels of the z-axis should be combined using various image processing methods to generate a single image file.
• “Pathology picture archiving and communication system (Pathology PACS)” is a system that archives, processes, and transmits DP images in accordance with international standards such as the Digital Imaging and Communications in Medicine (DICOM) format. Pathology PACS consists of an image-viewing and archiving software, a mass storage device, and a computer hardware system.
• “A laboratory information management system, or laboratory information system (LIS)”, is a software system designed to manage information related to the overall operation and management of a laboratory.
• “Validation” describes the process of confirming whether equipment, reagents, and test methods that have already been verified can be appropriately applied to an individual laboratory according to certain standards before implementation. Validation should be conducted using documents that provide a high level of assurance.
QC of DP systems
W.01.001 Do you have laboratory guidelines for DP covering overall DP workflow and is it easily accessible? (4)
Yes ( ) No ( )
* Laboratory DP guidelines can include the following content according to the scope of application and individual needs.
- Principles/guidelines for the operation of DP systems (Standard Operating Procedures, SOP)
- Information on personnel managing and using DP systems (organizational charts and roles)
- Principles/guidelines for the maintenance and repair of all facilities and equipment in a DP system
- Principles/guidelines for the collection, storage, use, and disposal of digital image data
- Principles/guidelines for personal information protection, management, and security
- Principles/guidelines related to telepathology and the use of portable devices
- Principles/guidelines for coping with emergencies and disasters
- Principles/guidelines for education of all DP system users
- Principles/guidelines for QC in DP systems
- Principles/guidelines for validation of DP systems
- Principles/guidelines for the other operation in DP systems
W.01.002 Does the DP director regularly review and check all the guidelines for the DP system? (2)
Yes ( ) No ( )
* The director of the DP system should review and confirm all the guidelines at least once a year, leaving a date and signature.
W.01.003 If the guidelines are changed, added, revised, or partly discarded, does the person in charge of the DP system review and confirm their content? (2)
Yes ( ) No ( )
* When major equipment constituting the DP system is newly introduced/changed, the content of the corresponding guidelines should be changed or added accordingly.
* The director of DP systems should review and leave a date and signature whenever there is a change in the guideline content.
* The contents of the guidelines that are changed or discarded should be retained for at least 2 years.
* Any changes, abolitions, or additions to the guidelines should be dated.
W.01.004 When the DP system director changes, does the new director review and confirm all the guidelines? (4)
Yes ( ) No ( )
* The new director should review and confirm the guidelines, and leave the date and signature.
W.01.005 Is there a system to ensure that all employees using the DP system are aware of the guidelines? (2)
Yes ( ) No ( )
* In-house education for the guidelines should be implemented, and trainees should leave training dates and signatures.
W.01.006 Do you have an internal QC system for the DP system in place and implemented? (32)
Yes ( ) No ( )
* Internal QC of DP systems should include:
- Regular validation of DP systems
- Documentation, causal analysis, and statistics on errors that occur during whole slide scanning
- Maintenance check report for overall equipment of DP system
- Documentation and troubleshooting of errors between DP systems and LIS (or hospital information systems, HIS)
- Inspections related to privacy and personal information security
- Guidelines for follow-up measures of errors in internal QC
W.01.007 Do you regularly conduct internal QC of DP systems? (8)
Scoring: ______________
* Internal QC should be implemented periodically, daily, weekly, monthly, and quarterly, in accordance with internal regulations as well as validation after major changes in the components of the entire DP system due to the introduction of new equipment and others. If it is conducted irregularly (when 20%–80% is satisfied), half of the score (4 points) is given, and if it is conducted with less than 20%, 0 points are given.
W.01.008 Does the person in charge of the DP system review and resolve the internal QC results in documentation? (8)
Yes ( ) No ( )
Personnel in DP systems
W.02.001 Are the personnel managing the DP system adequate in number? (4)
Yes ( ) No ( )
* The management team of DP systems consists of a variety of people, including pathologists, technicians, personnel who perform whole slide scanning, IT managers, and others.
* Information on personnel managing DP systems (such as organization charts and roles) should be thoroughly prepared and updated.
* Personnel managing DP systems should understand the subjects related to implementation, management, and maintenance of DP systems. DP personnel should continuously educate themselves for SOP and understand the difference in the diagnosis process between DP systems and conventional microscopy.
* The appropriate number of personnel managing the DP system may be determined according to the scale and workflow of the DP system in individual institutions.
W.02.002 Is the education/training for personnel using/managing DP systems being documented? (4)
Yes ( ) No ( )
* Training programs for new personnel using/managing DP systems should be prepared, and regular training should be provided for existing members.
* New training should be provided to employees using/managing digital pathology systems in the following circumstances: (1) introduction/replacement of key equipment in the DP system and corresponding changes in the laboratory guidelines, (2) change in the operational scope and method in the DP system, and 3) validation is newly performed.
W.02.003 Are there personnel primarily assigned to whole slide scanning? (8)
Yes ( ) No ( )
* Scanning personnel are required to undergo a certain training period according to the laboratory DP guidelines.
The hardware and software used in DP systems
W.03.001 Is the WSS in the DP system approved by the Ministry of Food and Drug Safety? (4)
Yes ( ) No ( )
W.03.002 Is the performance of the WSS regularly checked and maintained by the manufacturer? (4)
Yes ( ) No ( )
W.03.003 Is the performance of the WSS and the quality of scanned WSIs regularly evaluated by DP personnel? (4)
Yes ( ) No ( )
* Considerations and recommended functional requirements for a WSS (Supplementary Material S1) [2].
W.03.004 Does the image database system guarantee that the identification information of the glass slide matches that of the digital image? (2)
Yes ( ) No ( )
* Recommended functional requirements for image database systems (Supplementary Material S2) [2].
W.03.005 Even if the version of the image-archiving software changes, is it still available to view and use the archived data with updated software without any technical difficulty? (2)
Yes ( ) No ( )
* Recommended functional requirements for image database systems (Supplementary Material S3) [2].
W.03.006 Does the image storage method take a form of backup or mirroring? (4)
Yes ( ) No ( )
* Recommended functional requirements for image database systems (Supplementary Material S4) [2].
W.03.007 Do the image display devices (e.g., monitor) have the appropriate image quality for primary diagnosis? (2)
Yes ( ) No ( )
* Considerations and recommended functional requirements for image display devices and image viewing software (Supplementary Material S5, Supplementary Table S2) [2].
W.03.008 Does the image viewing software properly implement overview image, annotation, and image comparison functions to suit the pathological workflow? (2)
Yes ( ) No ( )
* Considerations and recommended functional requirements for image display devices and image viewing software (Supplementary Material S6) [2].
W.03.009 Are DP systems appropriately linked to the LIS, electronic medical records (EMR), or HIS? (4)
Yes ( ) No ( )
* Issues related to integration/links with LIS and EMR systems (Supplementary Material S7) [2].
Operation, management, and validation of DP systems
W.04.001 Is the laboratory SOP well prepared stating the following? (10)
1) Types of samples and staining methods to be used for primary diagnosis using a DP system (scope) Yes ( ) No ( )
2) Components of the DP system and SOP for each device Yes ( ) No ( )
3) Role and training records of the personnel using and managing DP system Yes ( ) No ( )
4) Guidelines on consultation and management of the referred patient samples using the DP system Yes ( ) No ( )
5) Guidelines for the storage, management, and disposal of DP image data Yes ( ) No ( )
6) Guidelines for privacy and information security Yes ( ) No ( )
7) Principles/guidelines related to telepathology and portable device use Yes ( ) No ( )
8) Guidelines for validation Yes ( ) No ( )
9) Plans/programs for QC Yes ( ) No ( )
10) Principles/guidelines for emergencies and disasters Yes ( ) No ( )
* 1 point to each item.
W.04.002 Is in-house validation of newly introduced devices of the DP system being conducted and documented? (12)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S8) [2].
W.04.003 Is the validation study conducted under conditions that are consistent with the clinical use intended by the DP system manufacturer? (4)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S9) [2].
W.04.004 Is the validation study designed to be as similar as possible to the actual clinical settings in which the technology will be used? (4)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S10) [2].
W.04.005 Does the validation study cover the entire DP system? (4)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S11) [2].
W.04.006 When there are significant changes in the composition of the DP system, is the revalidation on the whole DP system being conducted? Do you have guidelines for this? (8)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S12) [2].
W.04.007 Is the validation intended to be conducted by at least one pathologist who has acclimated to the DP system? (4)
Yes ( ) No ( )
* For general hematoxylin and eosin (H&E) slides, frozen sections, cytology slides, and blood smears, validation must be performed on at least 60 samples for a single applicable field. For additional applicable fields such as immunohistochemical stains and special stains, validation could be performed by adding an additional 20 samples.
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S13) [2].
W.04.008 Is the validation carried out using a comparative analysis of concordance between microscopic and WSI-based diagnoses made by a single observer (intra-observer variability assessment)? (4)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S14) [2].
W.04.009 Did you have a washout period of at least 2 weeks to minimize the influence of recall bias during the validation? (4)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S15) [2].
W.04.010 During validation, do you assess the data integrity of the image acquisition by verifying whether all tissues on the glass slide have been properly scanned to form the digital image? (8)
Yes ( ) No ( )
* Guidelines and considerations for validation needed for the implementation of DP systems and internal QC needed during operation (Supplementary Material S16) [2].
W.04.011 Is additional validation being conducted on the samples for the detection of microorganisms (e.g., Helicobacter pylori), the cytology slides (cell smears, liquid-based cytology, or blood smears), and the cases suspicious for lymphoreticular neoplasms? (4)
Yes ( ) No ( )
* Scope of application (Supplementary Material S17) [2].
W.04.012 Are all the errors, its statistics, and its cause analysis being recorded during the whole slide scanning? (4)
Yes ( ) No ( )
W.04.013 Are WSIs being scanned at a minimum magnification of 20× (in case of H&E slides)? (4)
Yes ( ) No ( )
W.04.014 Do you manage regular inspection results for the image display device (e.g., monitor)? (4)
Yes ( ) No ( )
* Considerations and recommended functional requirements for image display devices and image viewing software (Supplementary Material S18) [2].
W.04.015 Is the data being stored according to the data-preservation period determined by the individual laboratory? (4)
Yes ( ) No ( )
* Considerations and recommended functional requirements for image database systems (Supplementary Material S19) [2].
Personal information protection and information security of DP image data
W.05.001 Do the guidelines include the instruction and regulation on the collection and management of personal information and information safety? (16)
Yes ( ) No ( )
* Digital pathological imaging data should be stored systematically with the help of information processing experts and easily found as needed, and methods for regulating access to appropriate security and information should be established to protect privacy.
* There should be appropriate guidelines for data sharing and wired/wireless transmission that include the extent to which personal information is shared and how it is protected.
* Issues related to telepathology, firewalls, protection of personal information, and mobile device use (Supplementary Material S20) [2].
W.05.002 Does the DP guideline specify the external personnel or institutions that can access medical information and data using DP systems? (4)
Yes ( ) No ( )
W.05.003 Is there a person in charge of information security for the DP system? (4)
Yes ( ) No ( )
W.05.004 Is there a suitable system to prevent the loss of personal medical information in the case of hardware or software failure in the DP system, other emergencies, or disasters (e.g., power outages due to natural disasters)? (4)
Yes ( ) No ( )
* Measures and guidelines should be implemented to prevent the spread of failures or disasters that cause problems, plan periodic data/information backups, and recover corrupted data/information.
Quality assurance program trial for DP
Four leading hospitals, Seoul St. Mary’s Hospital, Seoul National University Hospital, Yongin Severance Hospital, and National Cancer Center participated in the QAP trial for DP. At the 46th Annual Spring Meeting of the KSP and the 73rd Annual Autumn Meeting of the KSP, eight hospitals, including the Samsung Medical Center, Yonsei Severance Hospital, Kangbuk Samsung Hospitals, and Seoul Asan Medical Center, in addition to the aforementioned hospitals, shared institutional experience on DP implementation and feedback after participating in the trial [17-24]. In addition, 11 DP directors, WSS technicians, and DP users from these hospitals submitted a feedback survey.
Current status of DP implementation in Korea
As of 2022, 40 out of 214 pathology laboratories (18.7%) implemented DP for primary diagnosis, archiving, consultation, and research and 2–10 more laboratories are expected to implement DP within next 1–2 years. Majority of the laboratories with DP is using DP for research, followed by archive, and consultation. Only about 15% of these laboratories are being estimated to use DP for primary diagnosis. The feedback survey showed that these pathology laboratories are currently processing 40%–100% of the total H&E examinations digitally (5,000 to 50,000 cases annually per lab). These labs are scanning mostly a part of H&E, some special and immunohistochemical stains, rarely immunofluorescence, silver in situ hybridization, or fluorescence in situ hybridization and are planning to expand the coverage.
QAP trial results
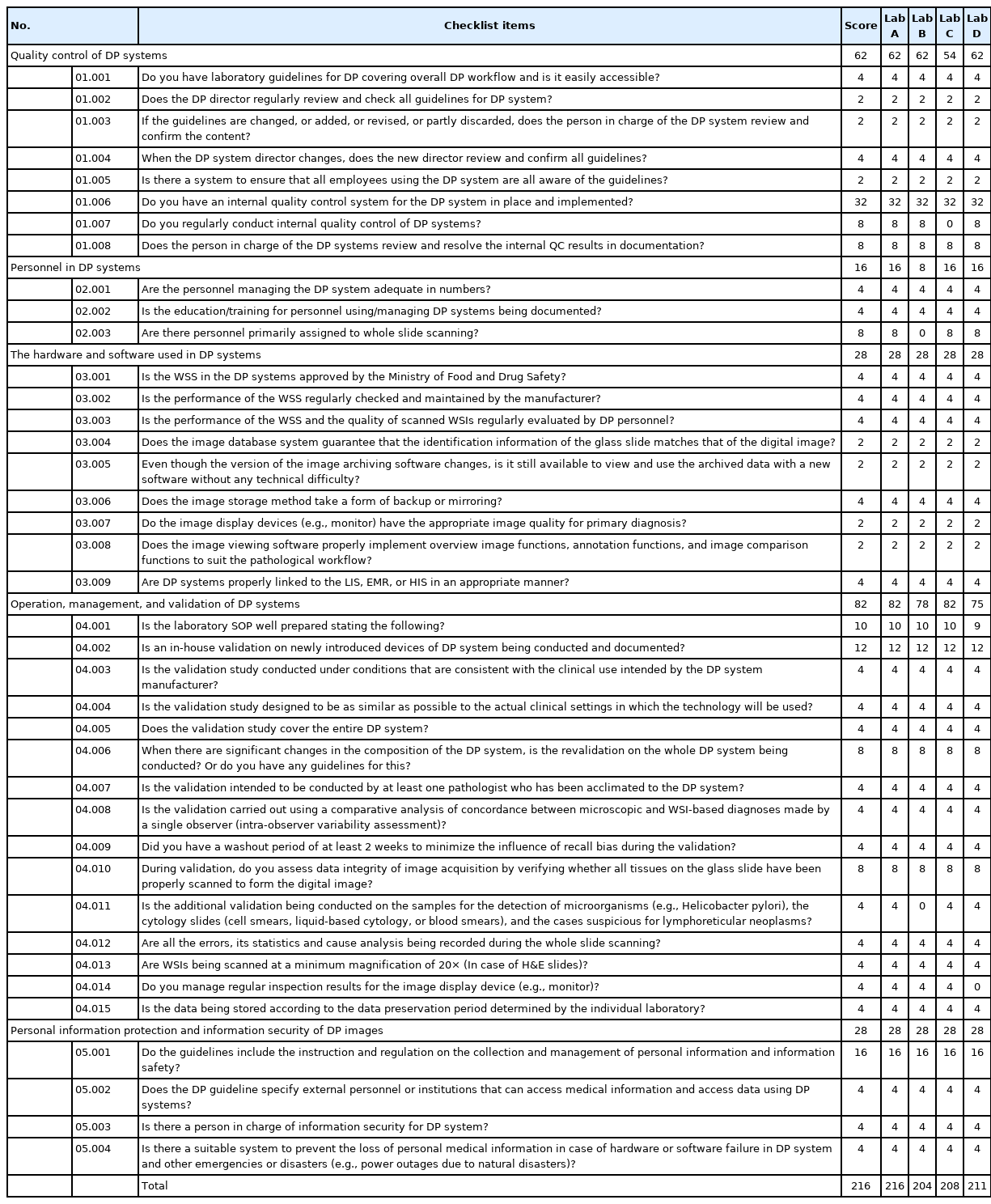
Four leading hospitals, Seoul St. Mary’s Hospital, Seoul National University Hospital, National Cancer Center, and Yongin Severance Hospital, participated in the QAP trial for DP. Table 5 summarizes the results. Average score was 209.75 out of 216 ranging from 204 to 216 with 1 to 2 missed items in each lab. All checklist items according to the hardware and software used in DP systems and personal information protection and information security of DP images were well prepared by all laboratories. Missed items were W.01.007, W.02.003, W04.001.004, W.04.011, and W.04.014, which do not affect the integrity of DP system seriously and can be improved in the future.
Feedback survey after DP QAP trial
Jang K-T from Samsung Medical Center highlighted focusing error, robotic motor dysfunction, localization error of the region of interest, software upgrades issue, compatibility between server and storage, and security software troubles as major issues during DP implementation [20]. He mentioned fast and convenient accessibility and reduced time of tumor annotation for additional ancillary tests, convenient application in multidisciplinary conferences, and education as the major benefits of the DP system. He also pointed out that the current DP systems fall behind the users’ expectations because there are still many problems in incorporating the system into the conventional pathology workflow, in which thorough QAP is required.
Lee KB from Seoul National University Hospital mentioned delayed turn-around time (TAT) due to scanning, unfamiliarity with WSIs, and increased workload of pathology lab personnel as the most worried aspects during DP implementation [24]. However, it turned out that the TAT could be reduced as the DP systems were expanded to the whole sample, including immunohistochemistry. The number of active user pathologists could increase over time, and gradual expansion of the DP system could increase the flexibility of the rapid workload increase. She highlighted the increased patient safety of the DP system, which is based on easy access to the archive, fast comparison of previous examinations, and instant intra- or interdepartmental consultation. She also mentioned that this could be very important for the general quality of pathologic diagnosis services.
Hong SW from Yongin Severance Hospital, Yonsei University introduced the advanced facilities of the digital hospital of Yongin Severance Hospital, including the Integration and Response Space, Real Time Location System, artificial intelligence-based chest X-ray interpretation system, mobile PACS, 5G mobile network-based server and storage, and DP solution, including voice recognition system, digital gross lab recording and photography system, and barcode/QR code sample tracking system [19]. She also shared that most errors were found during the pre- and post-scanning quality checks, such as localization error of the region of interest, foreign body/air bubble during the mounting, and handling errors by lab personnel. Over a year and a half after DP implementation, the error rate of her laboratory decreased from 0.61 to 0.02 as the DP coverage increased from 75% to 100%. She also mentioned witnessing a significantly reduced TAT, especially for reviewing prior exams and intra-/interdepartmental consultation, as well as a possible reduction of workload and slide storage space.
Some surveyees did not seem to understand the DP checklist items properly and they raised questions, the need for revision of some items for better clarification, or the need for more educational opportunity on DP from the KSP. Overall, the surveyees replied that the DP checklist was helpful in preparing internal QC guidelines on DP and laboratory QAP on DP.
DISCUSSION
DP will be a core of pathology in future medicine, playing a central role both in clinical practice and in various fields of translational research by providing faster and more accurate diagnosis and enhanced patient safety, and by becoming valuable data with enormous potential [1]. QAP holds the key to the successful utilization of DP systems considering the many practical difficulties that arise during the incorporation of DP systems into the conventional pathology workflow. As each laboratory should prepare institutional guidelines on DP and QAP for DP, it is highly recommended to refer to this checklist along with consensus recommendations for pathologic practice using DP. In addition to other QAP activities in the pathology field, initial validation when implementing new DP systems, internal pre- and post-scanning quality checks with laboratory QAP for DP during daily routine practice, and continuous education for lab personnel should be prepared and conducted properly.
As the survey after the DP QAP showed, most participants agreed that there should be more educational opportunities on DP from the KSP. Currently, DPSG provides workshops on DP and other newly developed technology to KSP members every 4–5 years and last May, the latest workshop includes sessions for DP terminology, practical recommendations for DP implementation and its integration into HIS, standardization of DP data, introduction of WSSs and displays for DP, morphometric analysis software, AI-based computer-assisted diagnosis software, and other new technologies such as block chain and non-fungible token-based medical data sharing and common data model-based distributed research network. The DPSG also plans a regular educational program for pathology residents and fellows. Continuous efforts to educate new and existing lab personnel and pathologists should be made by the KSP DPSG, and each lab should also encourage personnel to participate in these educational opportunities in addition to the internal education plan. In addition, the CQA of the KSP needs to continue to educate examiners and examinants with the DP checklist items until they become familiar.
Although the long-term benefits of DP are profound and obvious, the initial cost of DP implementation is a huge obstacle for a lab to accept this new technology. In a study on the preparation of the Reimbursement Assessment Guideline of Innovative Medical Technology (Pathology AI-based technology), Lee KB at Seoul National University suggested that government authorities make new reimbursement codes for DP or make an indirect method to support DP implementation [25]. She highlighted that DP can reduce the total amount of medical costs over time and enhance the overall quality of pathologic diagnosis service, as well as the quality of healthcare service, although DP might take more time, costs, and manpower during the initial time for implementation. She also mentioned that it can save a lot of medical costs by increasing specialist consultation and reducing overtreatment or missing treatment time, resulting in increased diagnostic accuracy of pathologic diagnosis and enhanced treatment. It also might reduce redundant tests during hospital transfer, such as immunohistochemistry, and increase patient safety by facilitating the use of sample tracking systems such as barcodes or QR codes. Although DP technology has been implemented since mid-2000s, it took almost 20 years for some leading institutes to become fully digital. The national healthcare service and insurance system should support DP technology to bring about this fundamental change.
The last 2 years were a monumental period for every aspect of society and way of living and working because the COVID-19 pandemic forced us to change. The need for remote communication, working from home, and distant, ‘untact’ medical services has increased. DP has also received attention as the best solution to this unexpected crisis in the field of pathology. Many institutes in Korea have also begun to accelerate the implementation of DP after the pandemic. However, there are still many practical issues during DP implementation that affect the process. Chae SW from Kangbuk Samsung Hospital highlighted the need for standardization of pathologic data. Since the file formats differ by WSS domain, a standardized format such as DICOM in radiologic imaging is essential for smooth incorporation into the electronic health record system or LIS and better utilization for research and collaboration between laboratories [17,26-28]. Jung CK from Seoul St. Mary’s Hospital, Catholic University of Korea mentioned that developing artificial intelligence and other 4th industrial revolution technology was impossible without data standardization [22,29].
In summary, digital transformation in pathology is an inevitable change of timely importance and is the center of next-generation pathologic practice, healthcare service, education, and research. For the successful implementation of DP systems in the pathologic diagnosis process, continuous QAP from each laboratory should be accompanied by institutional, governmental, and policy support. Further efforts on standardization of pathologic data from the market are also needed to inspire innovative applications to new technologies, such as artificial intelligence prediction for cancer classification and mutation [29-31]. The CQA of the KSP will continue to revise this checklist according to feedback from the following QAP trials for DP.
Supplementary Information
The Data Supplement is available with this article at https://doi.org/10.4132/jptm.2022.09.30.
Notes
Ethics Statement
All procedures performed in the current study were approved by the Institutional Review Board of the Catholic University of Korea (UC21ZCSI0057) in accordance with the 2018 Helsinki declaration. Formal written informed consent was not required with a waiver by the appropriate the Institutional Review Board of the Catholic University of Korea (UC21ZCSI0057).
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Code Availability
Not applicable.
Author contributions
Conceptualization: YC, DWK. Data curation: YC, JMB, DWK. Formal analysis: YC, JMB, DWK. Funding acquisition: YC, HSH. Investigation: YC, JBM, GK. Methodology: YC, JMB, DWK. Project administration: HSH. Resources: YC, JMB. Software: YC, JMB, GK. Supervision: DWK, HSH. Validation: YC. Visualization: YC. Writing—original draft: YC. Writing—review amp; editing: JMB, DWK, GK, HSH. Approval of final manuscript: all authors.
Conflicts of Interest
YC, a contributing editor of the Journal of Pathology and Translational Medicine, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding Statement
This study was supported by the Korean Society of Pathologists (2020).
Acknowledgements
I appreciate Prof. Kee-Taek Jang, Prof. Kyoung Bun Lee, Prof. Soon Won Hong, Prof. Seoung Wan Chae, and Prof. Chan Kwon Jung for sharing the data of conference proceedings.