Tubular adenoma arising in tubular colonic duplication: a case report
Article information
Abstract
Colonic duplication constitutes a rare congenital anomaly, characterized by the presence of hollow cystic or tubular structures exhibiting an epithelial-lined intestinal wall. Diagnostic challenges persist due to its low incidence and manifestation of nonspecific symptoms such as abdominal pain or constipation, resulting in a reluctance to pursue surgical resection. As associated malignancies in colonic duplication are rare, the inherent malignant potential of these anomalies remains undetermined. Additionally, despite reported instances of associated malignancies in colonic duplication, there is an absence of reports in the literature detailing tubular adenoma within these cases. The histologic features of the presented case are particularly noteworthy, situated at the precancerous stage, intimating potential progression towards adenocarcinoma within colonic duplication.
Gastrointestinal duplication manifests as a cystic or tubular structure connected to the broader gastrointestinal tract, featuring a standard epithelial lining and smooth muscle layer. This congenital anomaly is rarely observed, with an incidence rate of one in every 4,500 individuals [1]. Although it can arise anywhere along the gastrointestinal tract, the ileum predominates as the most common site [2]. Colonic duplication, constituting 4%–18% of all gastrointestinal duplication cases [3], typically becomes evident in early childhood, with approximately 80% of cases identified before the age of 2 [4]. Clinical presentations of colonic duplication exhibit variability contingent upon the type and location of the duplication. Patients may manifest chronic or acute abdominal pain, constipation, abdominal distension, or detect a palpable mass. The diagnostic challenge inherent in colonic duplication is compounded by its low incidence and presence of nonspecific symptoms, often resulting in diagnostic confusion with other intestinal disorders.
The risk of malignancy arising in colonic duplication remains unclear [5]. However, cases of adenocarcinoma arising in colonic duplication have been reported [6]. Although tubular adenoma is a precancerous lesion leading to adenocarcinoma in the colon, there is a paucity of reports documenting the occurrence of tubular adenoma within colonic duplication in the literature. This case report highlights a rare occurrence of tubular adenoma developing within a colonic duplication in a 40-year-old male.
CASE REPORT
A 40-year-old male patient visited the outpatient clinic for chronic constipation and abdominal pain. He reported a history of difficulty in defecation since childhood and had been hospitalized at the age of 10 for acute abdominal pain. Physical examination and laboratory assessments yielded no abnormalities.
The primary physician considered the possibility of a congenital anomaly or aganglionic megacolon. The patient was subsequently transferred to our hospital for further evaluation. An abdominal computed tomography scan revealed a large, stool-filled tubular structure on the right side (Fig. 1A), suggesting the diagnosis of a colonic duplication cyst communicating with the sigmoid colon. Colonoscopy further identified a bifurcation or outlet connecting to the duplication cyst within the sigmoid colon (Fig. 1B). The colonic duplication had expanded, and the examination revealed a mixture of liquid stool containing a large number of seeds and nuts.
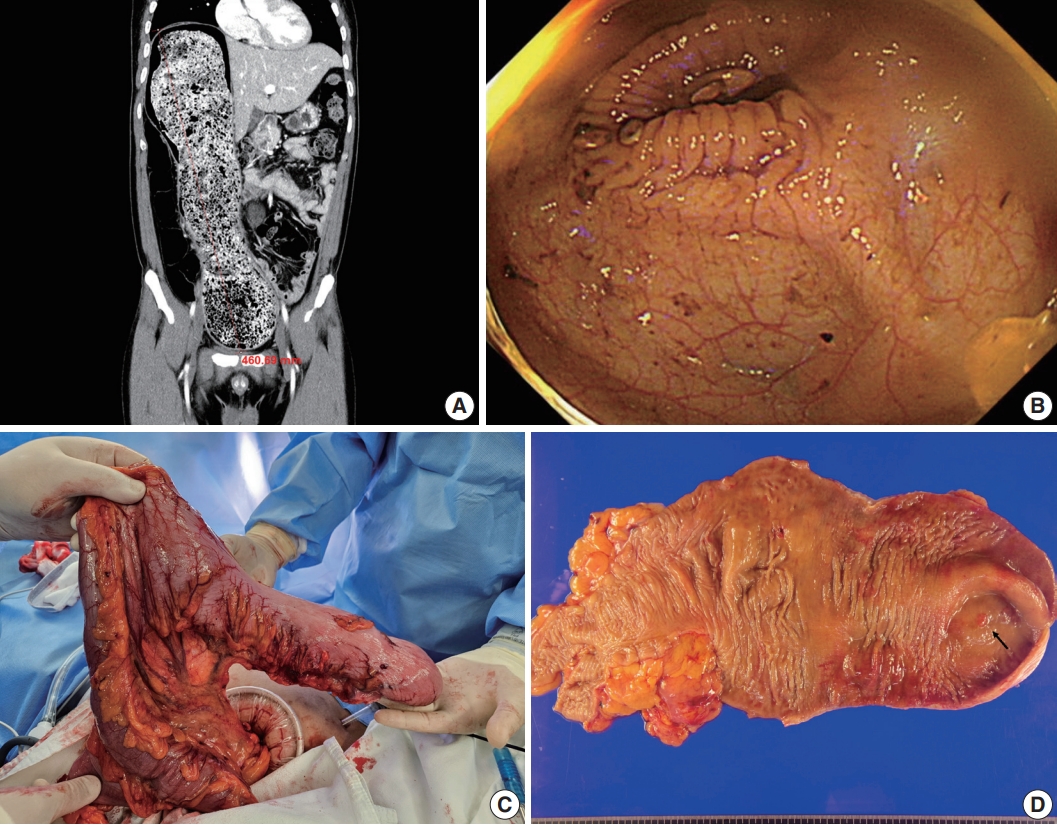
Radiologic, endoscopic, and gross findings. (A) Abdominal computed tomography shows a large tubular colonic structure, suggesting a duplication cyst connected to the sigmoid colon. (B) Endoscopy image shows a bifurcation leading to the duplication cyst in the sigmoid colon. (C) Intraoperative photograph shows the tubular bowel structure with a dead end, communicating with the sigmoid colon. (D) Gross appearance of tubular colonic duplication. The lesion measures 33 cm in length and 20 cm in greatest circumference. A polypoid nodule at the blind end is highlighted (arrow).
The subsequent laparoscopic exploration identified a tubular colonic duplication measuring approximately 30 cm in length, connected to the sigmoid colon (Fig. 1C). This duplication shared a common blood supply with the adjacent sigmoid colon. A colon segmental resection followed by functional end-to-end anastomosis, facilitated by a linear stapler, was performed. Gross examination revealed a blind-end tubular structure of the colon, measuring 33 cm in length and 20 cm in greatest circumference. A polypoid nodule was observed at the end of the duplication, measuring 0.6 cm in greatest dimension (Fig. 1D). Histological analysis demonstrated the full thickness of colonic structures, with three smooth muscle layers (Fig. 2A). The polypoid nodule exhibited characteristics consistent with a hyperplastic epithelial lesion, displaying hyperchromatic and elongated nuclei indicative of a tubular adenoma with low-grade dysplasia (Fig. 2B). Immunohistochemical staining further revealed increased p53 expression (Fig. 2C). The patient was discharged on postoperative day 5 and remained in good health during the 1-month follow-up.
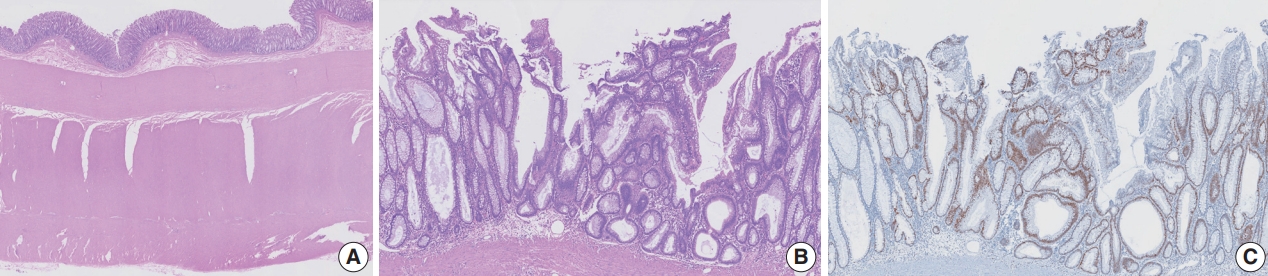
Microscopic findings. (A) A low-power view of the wall reveals normal colonic epithelial lining and three layers of relatively thickened smooth muscle. (B) A medium-power view of the polypoid nodule shows increased nuclear density with hyperchromasia, consistent with low-grade dysplasia. (C) Dysplastic epithelial cells show increased p53 positivity compared with adjacent normal mucosa.
DISCUSSION
Colonic duplication can be classified into two types: cystic and tubular duplication. Cystic colonic duplication is the most prevalent, constituting approximately 86% of cases, while tubular colonic duplication represents only 14% of occurrences [2]. Unlike cystic duplication, tubular colonic duplication establishes one or more direct communications with the native tract [7]. Typically originating on the mesenteric side of the bowel, this duplication shares a common blood supply with the adjacent native bowel, as observed in the presented case.
Despite the prevalence of nonspecific symptoms such as abdominal pain or constipation, the persistence of colonic duplication can lead to severe complications. In neonates or infants, intussusception and volvulus are frequently reported in cases of gastrointestinal duplication, occurring at rates of 10.9% and 23.8%, respectively [2]. Some instances of colonic duplication may mimic Crohn’s disease, possibly attributed to inflammation or ulceration within the adjacent bowel or the duplication itself [2]. In severe cases, there is a risk of spontaneous bowel perforation due to pressure-induced bowel ischemia [8].
A hypothesis exists suggesting that colonic duplication may harbor malignant potential [5]. These duplications are lined by colonic epithelial cells, and the occurrence of dysplasia or cancerization is plausible, akin to colonic mucosa. Given the tubular adenoma observed in our case and the documented cases of adenocarcinoma arising in colonic duplication [6,9], a comprehensive histological examination is imperative to exclude abnormal epithelial lesions obscured by the colonic duplication and to properly manage the disease.
Colonic duplication in adults is rare and presents diagnostic challenges without surgical intervention. Radiologic evaluations revealing a tubular or cystic structure filled with large stool-like materials communicating with the normal bowel should prompt consideration of colonic duplication. Post-surgery, meticulous gross and histological examinations are warranted, considering the potential presence of associated neoplasms such as tubular adenoma or adenocarcinoma arising within the colonic duplication.
Notes
Ethics Statement
Formal written informed consent was not required with a waiver by the appropriate institutional review board (Asan Medical Center IRB No. 2024-0404).
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Code Availability
Not applicable.
Author Contributions
Conceptualization: HL, YP. Investigation: HL. Resources: CK, HA. Supervision: YP. Writing—original draft: HL. Writing—review & editing: HL, YP. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.
