Primary thyroid diffuse large B-cell lymphoma: fine needle aspiration and histological correlation
Article information
Abstract
Primary thyroid lymphoma (PTL) is a rare type of cancer that arises within the thyroid gland, representing about 2%–8% of all thyroid malignancies. Fine-needle aspiration cytology is commonly used as the first-line diagnostic approach for thyroid nodules and can assist in identifying PTL when suggestive features are present. Herein, we report the case of a 59-year-old female patient who presented with a rapidly enlarging anterior neck mass over 20 days. Clinically, the case was challenging to distinguish from anaplastic thyroid carcinoma because of the sudden enlargement of the neck mass. However, pathological examination confirmed the diagnosis of primary thyroid diffuse large B-cell lymphoma. Fine-needle aspiration cytology proved valuable in avoiding unnecessary surgical resection and guiding appropriate treatment. Additionally, we provide a brief review of the clinical and cytopathological features of primary thyroid lymphomas.
INTRODUCTION
Primary thyroid lymphoma (PTL) is defined as a lymphoma that arises solely in the thyroid gland and regional lymph nodes, without evidence of systemic involvement at the time of diagnosis. It is a rare entity, accounting for approximately 1%–2% of all extranodal lymphomas and 2%–8% of thyroid malignancies [1,2]. Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of PTL. Fine-needle aspiration cytology (FNAC) is the diagnostic method of choice for the initial evaluation of thyroid nodules and can aid in the diagnosis of primary thyroid lymphomas. Herein, we report a case of primary thyroid DLBCL and describe its cytological features as observed through FNAC. Additionally, we briefly review the literature on the clinical and cytopathological characteristics of primary thyroid DLBCL.
CASE REPORT
A 59-year-old female patient presented to the otolaryngology department for evaluation of a rapidly enlarging anterior neck mass over the past 20 days. The patient had a history of diabetes and had been taking medications for 10 years. Laboratory examinations were as follows: thyroid function test showed, thyroid stimulating hormone, 2.740 μIU/mL (normal, 0.27 to 4.2 μIU/mL) and free T4, 15.40 pmol/L (normal, 12–22 pmol/L). Contrast-enhanced computed tomography demonstrated a 5×4 cm-sized mass in the left lobe of the thyroid. The mass revealed well-defined, ovoid, and solid features (Fig. 1A). Lymphadenopathy at levels 2, 3, 4, and 6 was observed in the left side of the neck.
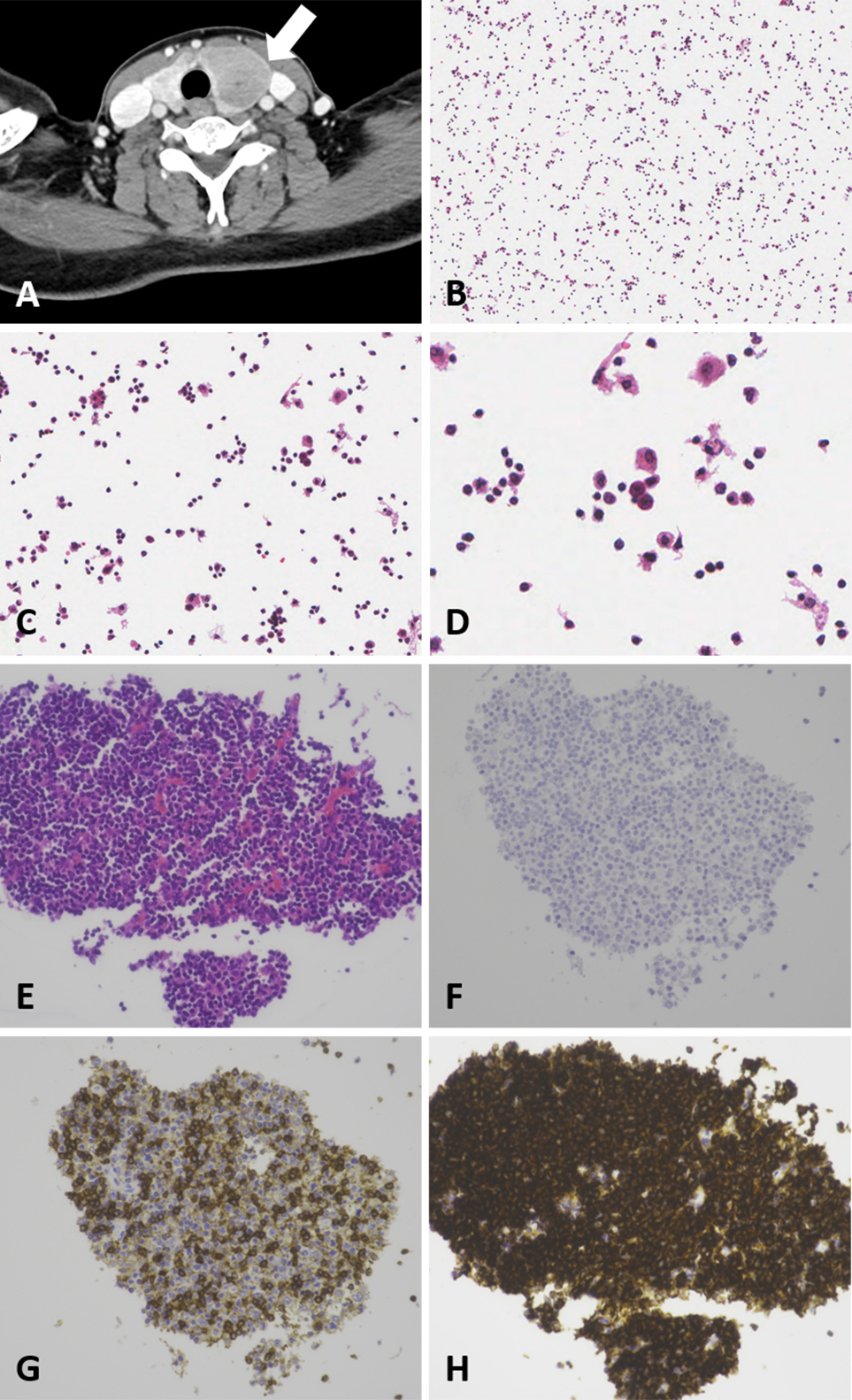
Radiological findings and cytological of primary diffuse large B-cell lymphoma arising in a thyroid gland. (A) Contrast-enhanced computed tomography demonstrated a 5 × 4 cm-sized mass in left lobe of the thyroid. The mass revealed well-defined and ovoid solid feature. (B) The ThinPrep slide showed hypercellular smear. (C) Tumor cells consisted of intermediate to large cells compared to background thyroid follicular cells. (D) At higher magnification, tumor cells revealed prominent nucleoli and mitotic figures. (E) Cell block demonstrating tumor cell clusters of highly atypical large cells with prominent nucleoli. (F) Thyroid transcription factor-1 were negative. (G) CD3 show positivity on T cells. (H) CD20 shows strong cytoplasmic and membranous staining in majority of tumor cells supporting B-cell origin.
FNAC was performed on a lesion in the left thyroid gland. The ThinPrep slide showed a hypercellular smear and intermediate-to-large cells compared to background thyroid follicular cells. The tumor cells showed prominent nucleoli and mitotic figures (Fig. 1B–D). A cell block was prepared from the thyroid FNA material to clarify the tumor cell lineage. The cell block contained several tumor cell clusters of atypical large cells with prominent nucleoli. The tumor cells were immunoreactive for CD19 and CD20. Tests for CD3, pan-cytokeratin and thyroid transcription factor-1 were negative (Fig. 1E–H). Based on these findings, B-cell lymphoma was suspected.
Thyroidectomy and lymph node dissection were then performed. Gross examination of the specimen revealed a well-defined tumor measuring 3.4 × 2.5 cm. At low magnification, the thyroid parenchymal architecture was partially effaced. Infiltration of the thyroid parenchyma by a population of intermediate-to-large lymphoid cells was also observed. Pathological examination of the background thyroid gland revealed Hashimoto’s thyroiditis. At a higher magnification, sheets of lymphoid cells showed irregular nuclear contours, prominent nucleoli, and mitosis (Fig. 2A, B). Immunohistochemical staining revealed strong positivity for CD20 and BCL2, and negativity for BCL6, CD3, CD10, and Epstein-Barr encoding region via in situ hybridization. Tumor cells showed Ki-67 index of 60% (Fig. 2C–F). The pathological diagnosis confirmed that the mass was primary thyroid DLBCL. After diagnosis, the patient was treated with the rituximab, cyclophosphamide, hydroxydaunorubicin, oncovin, prednisone, or prednisolone (R-CHOP) regimen. At the last follow-up in June 2023, the fluorodeoxyglucose‐positron emission tomography/computed tomography showed decrease in the size of left cervical lymph nodes.
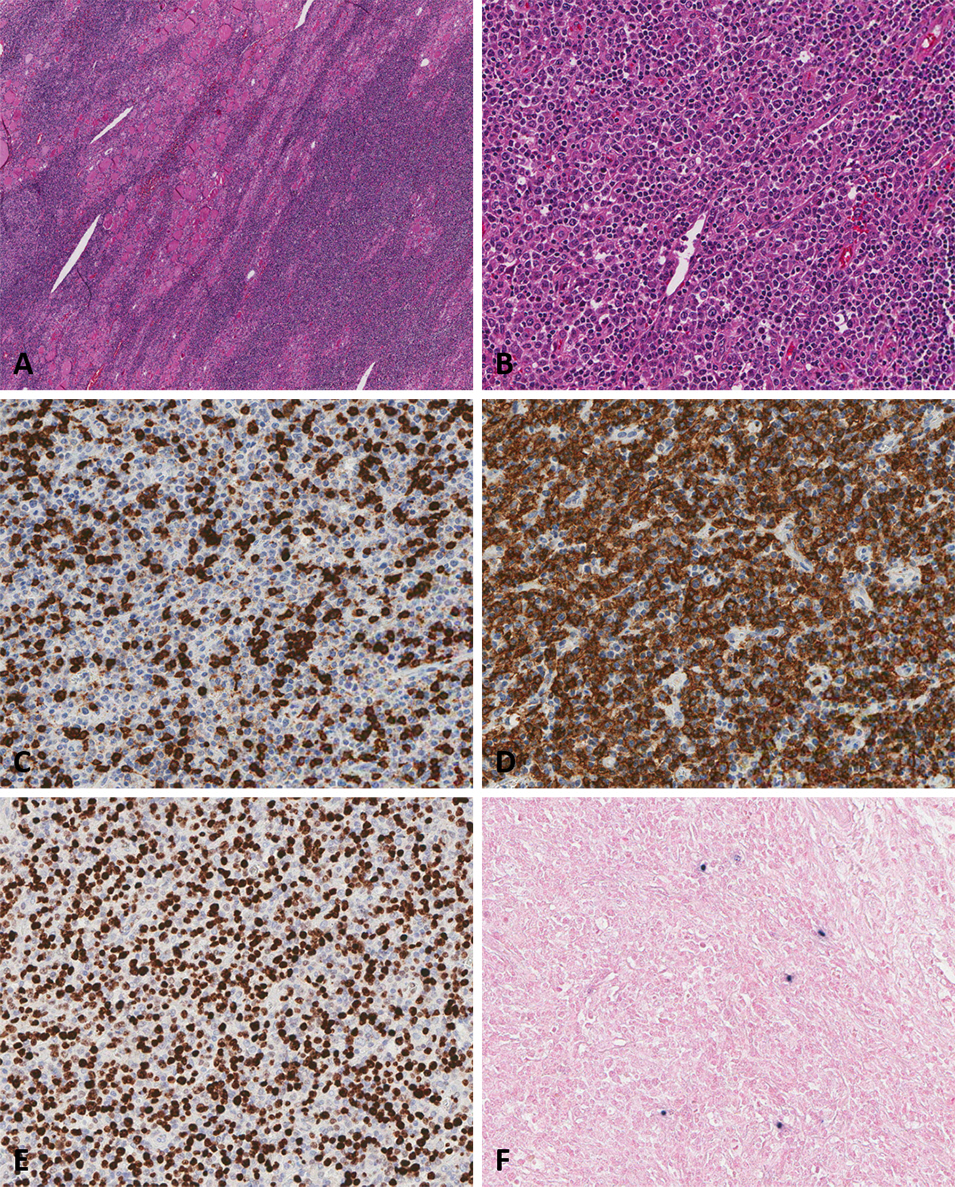
Histopathological and immunohistochemical findings of primary diffuse large B-cell lymphoma arising in a thyroid gland. (A) In low magnification, thyroid parenchymal architecture was partially effaced. (B) Infiltration of the thyroid parenchyma by a population of intermediate to large lymphoid cells was noticed. (C) In the diffuse large B-cell lymphoma (DLBCL) component, CD3 staining was negative. (D) The tumor cell in DLBCL component showed diffuse and strong positivity for CD20. (E) Tumor cells showed Ki-67 index of 60%. (F) In situ hybridization was negative for Epstein-Barr encoding region.
DISCUSSION
PTL is a rare malignancy that involves only the thyroid gland and regional lymph nodes, with no evidence of disease elsewhere at the time of diagnosis. The majority of PTLs are non-Hodgkin lymphomas, with DLBCL being the most common subtype. Other forms include mucosa-associated lymphoid tissue lymphoma, follicular lymphoma, and, less commonly, Hodgkin’s lymphoma [3]. Several studies have shown that PTLs develop in the context of Hashimoto’s thyroiditis [4]. It is well recognized that Hashimoto’s thyroiditis serves as a precursor to PTL [5]. In the present case, the patient was diagnosed with DLBCL arising in a background of Hashimoto’s thyroiditis, consistent with findings from previously reported cases.
The age of the patient with primary thyroid lymphoma typically ranges from 50 to 80 years, with a slight male predominance (male-to-female ratio, 1:0.75). Clinical presentation varies and may include systemic symptoms such as fever, weight loss, and rapidly enlarging neck mass [6]. PTLs lack specific radiological features, making it difficult to distinguish them from other thyroid neoplasms based on imaging alone. In the present case, imaging revealed a well-circumscribed, solid mass. Histopathological examination revealed aggregates of large atypical lymphoid cells. These cells formed a monomorphic population of intermediate-to-large sized lymphocytes with prominent nucleoli, irregular nuclear membranes, high nuclear/cytoplasmic ratios, and elevated mitotic activity. Immunohistochemical staining showed strong positivity for B-cell markers.
FNAC is a valuable diagnostic tool for a wide range of conditions, offering a safer and more cost-effective alternative to incisional biopsy. However, its role in the diagnosis of lymphoma remains controversial, as FNAC alone may be insufficient for definitive diagnosis and precise subtyping. In the present case, a diagnosis of primary thyroid B-cell lymphoma was established using FNAC in combination with cell block preparation and ancillary immunohistochemical studies. This case highlights the potential of FNAC, when supplemented with additional testing, to serve as a reliable alternative to conventional biopsy in the diagnosis of primary thyroid lymphoma.
Optimal treatment guidelines for PTLs have not yet been established. PTLs do not require surgical resection unless symptoms are present. In the present case, the patient underwent thyroidectomy for dysphagia caused by a rapidly enlarging mass. Targeting CD20-positive DLBCL cells has been proposed as a promising breakthrough in DLBCL treatment. Therefore, targeted therapy, including rituximab, may be a useful treatment [7]. In contrast, surgical resection is essential for the treatment of thyroid carcinomas, including papillary thyroid carcinoma, poorly differentiated thyroid carcinoma, and anaplastic thyroid carcinoma in most cases. In particular, the present case was clinically difficult to differentiate from anaplastic thyroid carcinoma in that there is a suddenly enlarging neck mass. Recognition of this entity and the utilization of FNAC are helpful in avoiding unnecessary surgical resection and establishing appropriate treatment guidelines.
Notes
Ethics Statement
This case report was approved by Jeonbuk National University Hospital Institutional Review Board (approval No. IRB 2023-02-020). Patient consent was obtained for publication. This case report was conducted in accordance with the Declaration of Helsinki (1975).
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author Contributions
Conceptualization: ARA. Investigation: YTH, WSM. Supervision: ARA. Writing—original draft: WSM. Writing—review & editing: WSM, YTH, ARA. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.
