Metaplastic Thymoma: Report of 4 Cases
Article information
Abstract
Metaplastic thymoma (MT), accepted in the World Health Organization 2004 scheme, is a circumscribed tumor of the thymus exhibiting biphasic morphology. We herein describe the clinicopathologic features of four MTs and the differential diagnoses of this unusual tumor. There were three women and one man with mean age of 49.5 years. The patients were found to have mediastinal masses, and underwent surgical excision. One exhibited symptoms of myasthenia gravis, and the serum titer for anti-acetylcholine receptor antibody was positive. Grossly, the tumors were encapsulated, and showed vaguely multinodular, solid, tan-white to yellow cut surfaces. Histologically, they comprised epithelial islands intertwining with bundles of delicate spindle cells. The patients remained well after surgical excision at 5-55 months. Because of the distinctive histological appearance and benign clinical course, MT should be distinguished from other more aggressive mediastinal neoplasms displaying biphasic feature.
Primary thymic epithelial tumors characterized by a biphasic histologic appearance are uncommon.1 Such cases have been reported as examples of sarcomatoid carcimoma (SC) or carcinosarcoma, which account for 7% of all thymic carcinomas.2,3 Metaplastic thymoma (MT), accepted in the World Health Organization (WHO) 2004 scheme, is a circumscribed tumor of the thymus in which anastomosing islands of epithelial cells are intermingled with bland-looking spindle cells.4-7 Relatively bland cytology and usually good prognosis suggest that this tumor is benign. It is important not to mistake MT for the vastly more aggressive tumors displaying a biphasic epithelial and spindle cell morphology. To our knowledge, only one case with a similar histologic pattern has been reported in Korean population, and only about 15 cases have been described in the English literatures.4-9 Here, we present the clinicopathologic features of 4 MTs, one of which is the first case associated with myasthenia gravis (MG).
CASE REPORTS
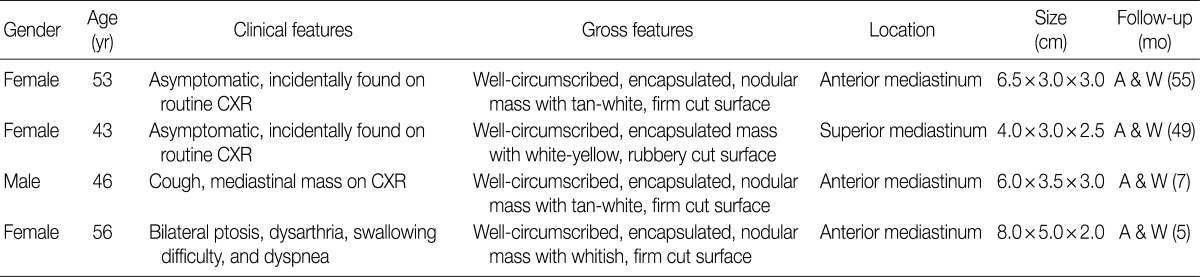
The clinicopathologic features of 4 patients are summarized in Table 1. There were 3 women and one man, and the mean age of diagnosis was 49.5 years. Two patients were asymptomatic, and one, who had smoked for 10 pack-years, complained of cough. A 56-year-old woman had manifested the symptoms of MG, such as ptosis, dysarthria and difficulty in swallowing, and the serum level of anti-acetylcholine receptor antibody was 12.52 nmol/L. The patients were found to have an anterior or superior mediastinal mass on routine chest radiograph, and were further evaluated with computed tomography or magnetic resonance imaging (Fig. 1A). None of the patients had other autoimmune disorders and clinical evidence of tumor elsewhere. The masses were treated with complete surgical excision. All the patients were alive and well without local recurrence at 5-55 months.
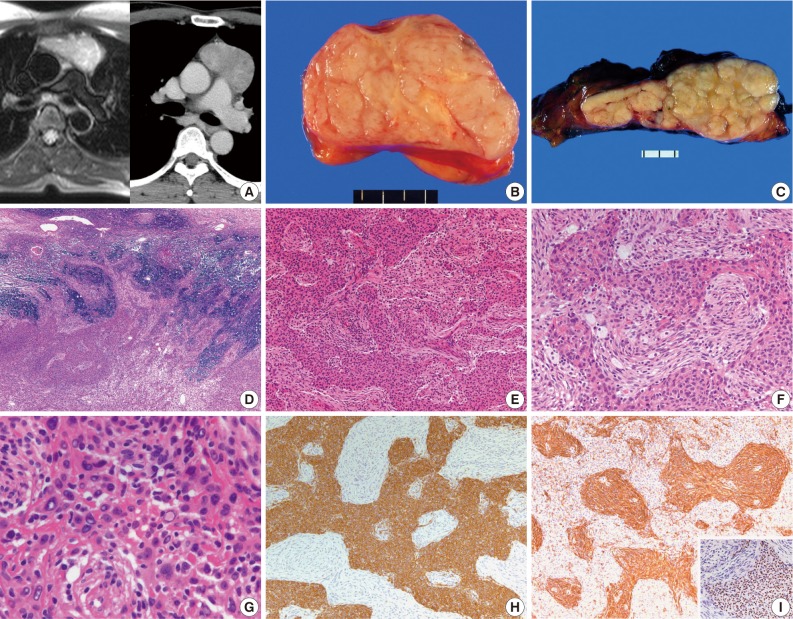
(A) T2-weighted magnetic resonance image shows a high-signal mass lesion in the anterior mediastinum (left). Computed tomography scan reveals a homogenously enhancing soft tissue mass in the anterior mediastinum (right). (B, C) Well-encapsulated masses with a vaguely multinodular appearance. The cut surfaces are solid, firm and tan-white to yellow. (D) The tumors are well-circumscribed, but show invasive buds in some areas. (E) Anastomosing islands of epithelial cells are disposed among spindle cells. (F) The epithelial component is fairly well-delineated from the spindle cell component. The latter comprises slender cells that are benign-looking. (G) The epithelial island shows enlarged atypical nuclei that are either hyperchromatic or empty-looking. (H) Cytokeratin is strongly positive in the epithelial component, but is negative in the spindle cell component. (I) Vimentin and p63 protein (inset) is strongly positive in the spindle and epithelial cells, respectively.
The tumors were variably encapsulated, and measured 4.0-8.0 cm in the greatest diameter. The cut surfaces were vaguely multinodular, firm or rubbery and tan-white to yellow (Fig. 1B, C). All the cases revealed essentially similar histologic features. They were well circumscribed with a thin rim of residual thymic tissue in the peripheral portions. One case showed focal invasion of the surrounding thymic tissue (Fig. 1D). The tumors were composed of anastomosing islands or broad trabeculae of epithelial cells disposed among delicate spindle cells (Fig. 1E). The two components were sharply delineated or gradually merged, and were present in variable proportions from area to area (Fig. 1F). The epithelial cells were oval to polygonal with vesicular nuclei and small prominent nucleoli. Some of the cells exhibited enlarged hyperchromatic or empty-looking nuclei, but mitotic figure was not observed in 30 consecutive high-power fields (Fig. 1G). The spindle cells showed a short fascicular or storiform growth pattern, and were bland-looking with fine nuclear chromatin and bipolar processes. Immunohistochemically, the epithelial cells were strongly positive for cytokeratin (1:130, clone AE1/AE3, Dako, Carpinteria, CA, USA) and p63 protein (1:400, clone 4A4, Dako), and were negative for vimentin (1:200, clone Vim 3B4, Dako). While the spindle cells were strongly positive for viementin, and were negative or focally, weakly positive for cytokeratin (Fig. 1H, I).
DISCUSSION
MT has been reported in the literatures under the designations 'thymoma with pseudosarcomatous stroma,' 'low-grade metaplastic carcinoma' or 'biphasic thymoma, mixed polygonal and spindle cell type'.7 Suster et al.5 suggested that the spindle cell component was reactive fibroblastic/myofibroblastic cells rather than the neoplastic proliferation of stromal elements arising from connective tissue in the thymus. On the other hand, Yoneda et al.4 considered the spindle cell component, which gradually merged with the epithelial islands at least at some foci, to be a deviation of the neoplastic precursor (i.e., mesenchymal metaplasia of tumor cells), and suggested both components arose from the same stem cells with the capacity of multidirectional differentiation.
All cases in our series had been submitted for intraoperative frozen section evaluation, and the diagnosis was rendered as 'consistent with MT.' Grossly, the tumors were well-circumscribed or encapsulated, and lacked distinct fibrous septation or cystic change that can be seen in conventional thymomas. Some areas showed marked predominance of one component to the exclusion of the other. If only areas composed of spindle cells are sampled, the constituent cells can mimic those of a type A thymoma.6 A diagnosis of such cases can be made by additional section to identify the typical biphasic pattern. The epithelial cells form lobules that are separated by acellular fibrous band in type B thymomas, while the epithelial component is intertwined with spindle cells and small amounts of loose collagenous tissue in MTs. Despite some epithelial cells exhibit enlarged atypical nuclei and may be similar to those of type B3 thymoma, MTs lack the perivascular spaces.4,5 The differential diagnosis of biphasic thymic tumor includes biphasic mesothelioma, synovial sarcoma, teratoma and ectopic hamartomatous thymoma (EHT). It is noteworthy that EHT is a benign tumor of the lower neck showing an admixture of epithelial islands with spindle and adipose cells. This tumor is not deep-seated, and cytokeratin is positive in both epithelial and spindle cell component with at least focal glandular differentiation.10-12 In contrast to EHT, MT exhibits alternating areas of epithelial and spindle cell component, which is highlighted by immunostaining for cytokeratin and vimentin, respectively.
The age range of reported MTs was 28 to 71 years (mean, 50.9 years), and the tumor tended to prevail in men.4,5,7 In our series, the male to female ratio was 1:3 with mean age of 49.5 years (range, 43 to 56 years). It seems that MT usually occurs in adult patients of both genders as thymomas and thymic carcinomas.7 Molecular studies on a limited number of cases have shown few genetic alterations, and favor interpretation of this tumor as a thymoma.7 However, MG and paraneoplastic autoimmune phenomena that are common in other types of thymoma have not been observed in MTs. All the 4 tumors had the same histologic and immunohistochemical features as other cases described in the literatures, but one of the patients reported herein was associated with MG, further supporting a closer relationship with thymoma than with thymic carcinoma. MT differs from SC in showing good circumscription and bland-looking spindle cells, even though squamoid epithelial islands may show nuclear polymorphism.4,5 Recently, 2 cases of SC arising in MT have been reported.8,9 The tumors had foci with marked atypical spindle cells, frequent mitotic figures and necrosis, but the follow-up was too short to assess behavior. Only one patient with MT was reported to have developed local recurrence at 14 months, and died at 6 years.4-6,8,9
We report 4 cases of an unusual morphologic variant of thymoma, characterized by a biphasic epithelial and spindle cell morphology. Because of the distinctive histologic appearance and indolent clinical behavior, MT should be distinguished from other more aggressive mediastinal neoplasms which display a biphasic pattern.
Notes
No potential conflict of interest relevant to this article was reported.