Clinicopathological Analysis of 21 Thymic Neuroendocrine Tumors
Article information
Abstract
Background
Thymic neuroendocrine carcinomas (NECs) are uncommon, for which there is no established information available because of a limited number of epidemiological study in Asia.
Methods
We reviewed 21 cases of surgically resected thymic NECs, and evaluated their pathological and clinical features.
Results
It showed male predominance (male/female ratio, 15/6) with wide age range from 20 to 72 years (mean age, 49 years). All 21 cases were divided into two types according to the World Health Organization criteria: atypical carcinoid (n=18) and large cell NEC (n=3). Three cases of atypical carcinoid (AC) were associated with ectopic Cushing's syndrome. All the patients (3/3) with large cell NEC (3/3) and 16.7% (3/18) of those with AC died of tumor progression. Common sites of metastasis included lung, lymph node, brain, lumbar spine, mediastinum, bone, and liver.
Conclusions
In conclusion, thymic neuroendocrine tumors carry a poor prognosis. Regarding the tumor classification, our results showed that a vast majority of carcinoids in the thymus correspond to ACs. In addition, our results also indicate that typical carcinoid is a very rare entity. Some cases of AC exhibited a large size, solid pattern and they showed aggressive clinical behavior, which highlights the spectrum of histologic appearances of thymic NECs.
Thymic neuroendocrine carcinomas (NECs) are uncommon, for which there is no established information available. To date, only a few studies have reported a substantial number of cases of NEC.1-5 The current evaluation of thymic neuroendocrine tumors is dependent on criteria for doing primary pulmonary neuroendocrine tumors.6 According to the World Health Organization (WHO), they are classified into four histological types: typical carcinoid (TC), atypical carcinoid (AC), small cell neuroendocrine cell carcinoma (SCNEC), and large cell neuroendocrine cell carcinoma (LCNEC).6 Most series have used the term "carcinoid" to describe these tumors. Some previous studies indicate that carcinoid tumors arising in the thymus may show a more aggressive behavior than their pulmonary counterparts.6 In recent years, attempts have been made to validate tumor grading and the range of clinical behavior.7-9 Still, however, little is known about the classification of thymic neuroendocrine tumors and their clinical behavior because of their rarity. In this study, we retrospectively reviewed 21 cases of surgically resected thymic NECs and evaluated their pathologic and clinical features.
MATERIALS AND METHODS
Cases
During a 16-year period (1995-2010), a total of 21 patients with primary thymic neuroendocrine tumors had been surgically treated at the department of thoracic and cardiovascular surgery of Samsung Medical Center in Seoul, Korea. Note that these 21 cases included no cases of pulmonary neuroendocrine tumors and tumors involving both lung and thymus. Clinical data and follow-up data were obtained through a retrospective analysis of the medical records, and these data include sex, age, initial symptoms and signs, a notable past history, gross findings, treatment and follow-ups. Adequate information was obtained for all the 21 cases. The postoperative staging was done based on the classification system of Masaoka et al.10 for thymomas. All the patients were followed up until January of 2012 during a median follow-up period of 34.95 months.
Histological classification
For histological classification, the histopathologic features were assessed and these include tumor differentiation, mitotic rate, presence or absence of necrosis, presence of local invasion and lymph node metastasis. The tumors were classified into four types: TC, AC, LCNEC, and SCNEC according to the WHO criteria based on the histopathologic differentiation as shown below:
TC: A well-differentiated tumor with mitotic figures, fewer than 2 mitoses per 10 high power fields (HPFs) and no necrosis
AC: A well-differentiated tumor with mitotic figures, 2-10 mitoses per 10 HPFs and/or presence of necrosis
SCNEC: A poorly-differentiated tumor with small cell cytology, mitotic figures with more than 10 mitoses per 10 HPFs and extensive areas of necrosis
LCNEC: A poorly-differentiated tumor with non-small cell NEC, mitotic figures with more than 10 mitoses per 10 HPFs and extensive areas of necrosis.6
Immunohistochemistry
In the current study, we used representative formalin-fixed, paraffin-embedded tissue sections for the immunohistochemical staining in our series of 21 cases of primary thymic neuroendocrine tumors. To evaluate neuroendocrine differentiation of the thymic neoplasm, synaptophysin, chromogranin or CD56 were chosen as neuroendocrine markers. Immunohistochemical staining was performed on 3-µm thick sections from each case using a biotin-avidin-peroxidase method on a BOND-MAX autostainer (Leica, Wetzlar, Germany) after retrieval with T/E buffer (CD56) or citrate buffer (chromogranin and synaptophysin). We also used primary antibodies to synaptophysin (1:100, Dako, Glostrup, Denmark), chromogranin (1:400, Dako), CD56 (1: 200, Novocastra, Newcastle upon Tyne, UK) and adrenocorticotrophic hormone (ACTH; 1:100, Dako).
RESULTS
Clinical features
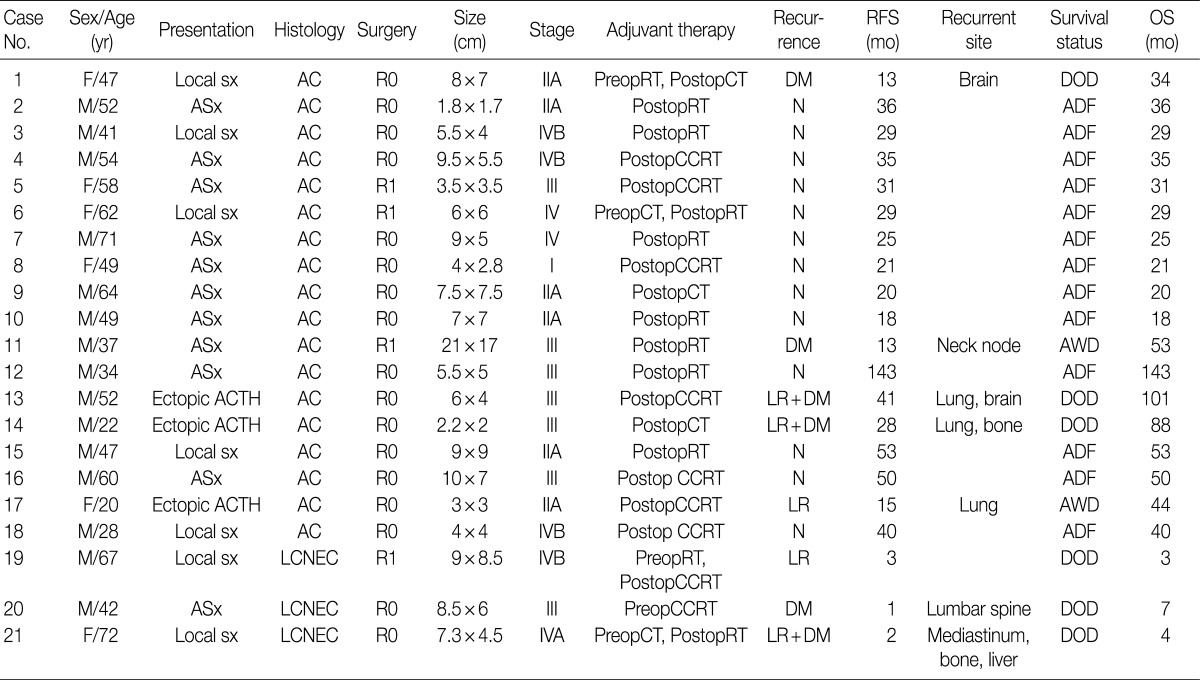
In our series, there was a male predilection with a male-to-female ratio of 15:6. In addition, the mean age of patients was 49 years (range, 20 to 72 years). Three cases of AC were associated with ectopic Cushing's syndrome. Clinical and radiologic impressions were thymoma or lymphoma preoperatively in most cases of our series. After the resection, adjuvant therapy was performed according to our treatment protocol. Postoperatively, the concurrent chemoradiation therapy (CCRT) and the radiotherapy (RT) alone were preferentially performed for cases of LCNEC and AC, respectively. During the follow up period, a local recurrence or a distant metastasis were observed in 100% (3/3) of patients with LCNEC and 27.8% (5/18) of those with AC. Common sites of metastasis included lung, lymph node, brain, lumbar spine, mediastinum, bone, and liver. The cause of death was tumor progression in 100% (3/3) of patients with LCNEC and 16.7% (3/18) of those with AC. Clinical features are summarized in Table 1.
Histological features
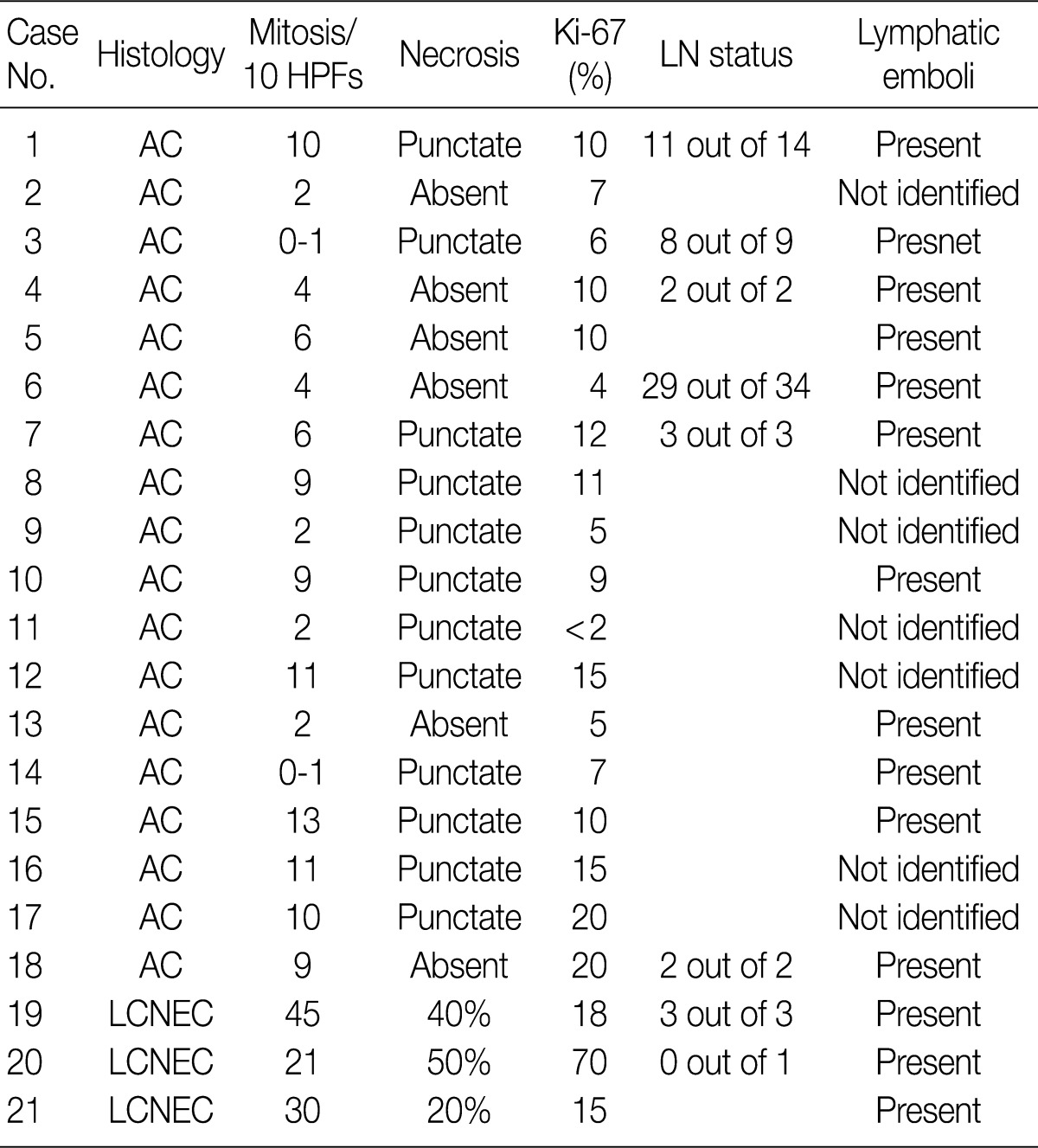
All 21 cases were divided into two types according to the WHO criteria: AC (n=18) and large cell NEC (n=3). In addition, there were no cases of TC tumor. Histological features are summarized in Table 2. The tumors were described as a large, soft and whitish-tan to brown mass with the greatest diameter of 1.8-21 cm (Fig. 1A). The mean size of the mass was 6.81 cm and 8.27 cm in cases of AC and LCNEC, respectively. Some of the tumors showed an infiltrative growth pattern to the adjacent organs such as the pericardium. On cut sections, the tumors revealed focal areas of hemorrhage and necrosis. In particular, LCNEC showed extensive areas of necrosis, which is the hallmark of poorly-differentiated neuroendocrine thymic carcinomas (Fig. 1E). AC showed a punctate necrosis with a maximum of 13 (0-10) mitoses or it was devoid of necrosis but showed a proliferation with a mitotic rate of up to 9 mitoses per 10 HPF (Fig. 1B, C). Thymic LCNEC was defined as a poorly-differentiated non-small cell NEC with a mitotic rate of >10 mitoses per 10 HPF. The mean number of mitotic cells per 10 HPF was 32. It was notable that there was an extensive necrosis (Fig. 1F, G). Of all the 18 cases of AC, 11 frequently revealed lymphatic emboli and six, undergoing a lymph node dissection, demonstrated a nodal metastasis. All the cases of LCNEC frequently showed lymphatic emboli. Of these, one case proved to histologically have a nodal metastasis. Finally, tumors associated with ectopic hormone secretion were also found to share the characteristic features of cytoplasm. That is, tumor cells had focally abundant clear cytoplasm.
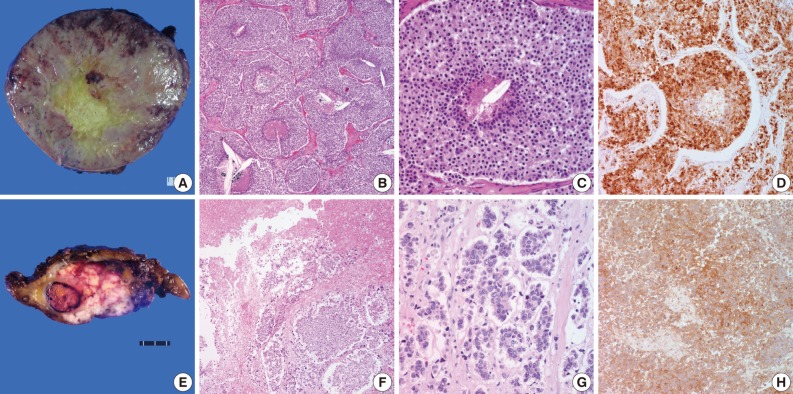
Atypical carcinoid presents as a soft, white-tan to brown mass (A). Atypical carcinoid is defined as a well-differentiated tumor with mitotic figures (2-10 mitoses per 10 high power fields) and/or a punctate necrosis (B, C). The stain of CD56 shows a diffuse membranous and cytoplasmic, dot-like staining in tumor cells of atypical carcinoid (D). Large cell neuroendocrine carcinoma shows an infiltrative growth pattern and the cut section reveals necrotic portion (E). Extensive tumor necrosis and high mitotic counts are highly characteristic of large cell neuroendocrine carcinoma (F, G). Large cell neuroendocrine carcinoma tends to exhibit weaker CD56 staining pattern compared to atypical carcinoid (H).
Immunohistochemical findings
Neuroendocrine differentiation was revealed by positive immunohistochemistry for neuroendocrine markers including synaptophysin, chromogranin and CD56. In all the cases, at least two of these markers were expressed. They showed diffuse membranous and cytoplasmic, dot-like staining pattern. There was no definite difference in the degree of immunohistochemical staining between cases of LCNEC and those of AC (Fig. 1D). But the degree of immunohistochemical staining was lower in cases of LCNEC as compared with those of AC (Fig. 1H). In addition, we also performed an immunohistochemical staining of ACTH for tumors with ectopic ACTH secretion. All the three cases showed a nuclear positivity.
DISCUSSION
We performed a clinicopathologic examination of primary thymic neuroendocrine tumors. Thymic epithelial tumors, predominantly or exclusively composed of neuroendocrine cells, are classified as NECs of the thymus. Thymic NECs are rare, constituting 2-5% of thymic epithelial tumors.6 There is a sufficient amount of statistical data for pulmonary NECs. But there is a paucity of data about the clinicopathologic correlations among the thymic NECs. Considering this, the first edition of the WHO classification of tumors of the thymus suggests that pathologists classify thymic neuroendocrine tumors based on the same criteria as NECs of the lung.6 It is known that a vast majority of carcinoids in the thymus would correspond to ACs if the same criteria are applied as the lung.6 In addition, several studies have reported that a substantial number of cases of AC are associated with ectopic hormone secretion.5,11,12 In the current study, our clinical series of patients (n=21) comprised 18 cases of AC and 3 cases of LCNEC. In addition, three cases of AC had endocrine manifestations. Furthermore, these three cases of AC were accompanied by Cushing's syndrome. It is well known that AC shows a better clinical behavior than LCNEC. However there were two patients with AC, associated with ectopic hormone secretion, both of whom died of tumor progression and metastasis although they had a small-sized tumor and low mitotic counts. Furthermore, there was another patient with ectopic hormone secretion who developed a pulmonary metastasis. In conclusion, our results indicate that ACs associated with ectopic hormone secretion show a poorer prognosis as compared with conventional ones. In our series, there were no cases of TC. This implies that TC is a very rare entity unlike the pulmonary NECs. Over the past few decades, a three-tiered pathologic classification has been used and NECS are classified into low grade, intermediate-grade, and high-grade ones.13,14 Based on this classification system, some previously diagnosed cases of low- or intermediate-grade NECs actually correspond to AC. Those who were diagnosed with low or intermediate grade neuroendocrine carcinoma underwent post-operative CCRT while only post-operative RT was added to AC patients according to the current treatment trend.
With regard to the clinical behavior of NECs, our results are in agreement with the previous reports that thymic neuroendocrine tumors show a poor prognosis. During the follow-up period, 100% (3/3) of patients with LCNEC and 16.7% (3/18) of those with AC died of tumor progression. However no statistical analysis has been attempted to determine whether the classification of tumors is not dependent on a prognosis of patients because of a limited number of cases enrolled in the current study.
Thymic neuroendocrine tumors are histologically classified according to tumor differentiation, presence or absence of necrosis and mitotic counts.6 ACs are therefore classified as a carcinoid tumor having architectural features of the classic type but exhibiting 2-10 mitoses per 10 HPF and/or foci of necrosis. AC is actually classified as a group of well-differentiated NEC. In our series, Cases 12, 15, and 16 were classified as an AC despite a high mitotic index of >10 mitoses per 10 HPF. In these cases, high mitotic counts may pose a diagnostic challenge to pathologists. However, tumor differentiation is one of the most important factors by which pathologists can make a differential diagnosis of carcinoid tumor from SCNEC and LCNEC. According to the WHO criteria, both TC and AC are classified a well-differentiated tumor and both SCNEC and LCNEC are classified a poorly differentiated tumor. Cases 12, 15, and 16 showed the similar characteristics of carcinoid tumor and they had a lack of the typical histologic characteristics of LCNEC such as extensive necrosis or poorly-differentiated pattern. Not including high mitotic counts, the histologic findings did not seem to correlate with a poorly-differentiated carcinoma which usually reveals aggressive clinical behavior. In addition, some tumors exhibited large tumor size and mitotic counts varied depending on the part of the tumor. We thought that high mitotic counts could be seen as the tumor grew. Therefore we classified such tumors as an AC rather than a LCNEC. Considering all LCNEC patients died of the tumor, the fact those patients were alive without evidence of relapse might support out diagnosis. Our results indicate that mitotic counts do not fully reflect morphology of the tumor. It can also be presumed that the current WHO classification needs a more detailed explanation because it might pose a diagnostic challenge to pathologists. Further studies are therefore warranted to examine the tumor classification.
The clinical behavior of AC varies in several studies. It has been reported that even "innocent" looking and encapsulated carcinoids bear a significant risk for recurrence, metastasis and tumor-associated death.6 On the other hand, one of the recent studies has shown a better prognosis of atypical thymic carcinoids as compared to pulmonary carcinoids.6 In our series, 16.7% (3/18) of patients with AC patients died of tumor progression, two of whom had a concurrent presence of ectopic hormone secretion. This implies that hormone-expressing tumors show an unfavorable prognosis.
Further, regarding the view that thymic neuroendcrine tumors are clinically more aggressive than morphologically identical neuroendocrine tumors of the lung, we also observed that primary thymic LCNECs tended to exhibit less neuroendocrine differentiation, such as trabeculae, nesting, rossettes and perilobular palisading patterns, which is commonly seen in pulmonary LCNECs. This may suggest that thymic LCNECs are higher-grade tumors than pulmonary LCNECs.
In conclusion, thymic neuroendocrine tumors carry a poor prognosis. Regarding the tumor classification, our results showed that a vast majority of carcinoids in the thymus correspond to ACs. In addition, our results also indicate that TC is a very rare entity. Some cases of AC exhibited a large size, solid pattern and they showed aggressive clinical behavior, which highlights the spectrum of histologic appearances of thymic NECs.
Notes
No potential conflict of interest relevant to this article was reported.