Metastatic Carcinomas to the Oral Cavity and Oropharynx
Article information
Abstract
Background
Metastases to the oral/oropharynx are very rare and their diagnosis is challenging.
Methods
We reviewed pathologic data for malignant tumors of the oral/oropharynx that were diagnosed at the Asan Medical Center, Seoul, Korea from 1995 until 2010.
Results
Twenty-nine cases of oral/oropharyngeal metastases were retrieved, comprising 2.0% of 1,445 malignancies. The most common primary sites were the liver and lung, followed by the stomach, colon, breast, prostate, and kidney. The gingiva was the most common metastatic site, followed by the tonsil/pillar, mandible, tongue, tongue base, palate mucosa, mouth floor, and buccal mucosa. Intervals between detection of primary tumors and metastases were variable, from -1 month to 104 months. Ten patients with lung (7 cases), liver, stomach, and kidney carcinomas manifested with oral/oropharyngeal metastases as the first sign of systemic metastases. The majority of patients had died within one year of the onset of an oral/oropharyngeal metastasis, but exceptionally long-lived cases were also present. The survival periods of patients with lung cancers were longer than those of patients with non-pulmonary tumors.
Conclusions
An awareness of the incidence, common primary sites, metastatic subsites, and metastatic courses or patterns of oral/oropharyngeal metastases is helpful in the diagnosis of metastatic carcinomas.
The oral cavity and oropharynx are very unusual sites of systemic metastases from primary cancers of other organs, which account for only about 1-2% of oral malignant tumors.1,2 A tendancy not to consider this rare possibility might lead to a misinterpretation of such metastases as a primary tumor of the minor salivary glands and result in excessive treatments. According to Western literature, the most common primary sites of oral/oropharyngeal metastases are the lung, kidney, and prostate for men, and the breast, female genital organs, and kidney for women.3 Metastatic tumors tend to involve the jaw bone more often than the oral soft part (2:1 ratio, respectively).3 Lim et al.4 metaanalyzed cases of 41 metastatic tumors in the jaws and the oral soft part that were reported in Korea. Collectively, the most common primary site was the liver (27.8%) for males and the female genital organs (16.7%) for females; the jaw bone was also more involved than the oral soft part (1.3:1 ratio, respectively).4 Roh et al.5 reported a 0.05% occurrence of head and neck metastases among 12,602 Korean patients with hepatocellular carcinoma (HCC). We separated the oral/oropharyngeal location from the sinonasal tract, of which metastases were previously studied,6 and analyzed oral cavity/oropharynx cancers in a 16 year period from one institute to reveal the incidence, primary sites, clinical manifestations, pathologic features, and prognosis of metastatic tumors to the oral cavity and oropharynx.
MATERIALS AND METHODS
Pathologic data on malignant tumors of the oral cavity and oropharynx diagnosed at the Asan Medical Center in Seoul, Korea from 1995 to 2010 were reviewed. There were 1,445 patients diagnosed with oral/oropharyngeal malignancy, which comprised of 1,089 primary carcinomas (984 squamous cell, 88 salivary gland, 5 undifferentiated, 2 odontogenic, 2 neuroendocrine, and 8 undetermined), 300 hematologic malignancies, 14 malignant melanomas, 9 sarcomas, 4 unclassified malignancies, and 29 metastatic carcinomas. Clinical data of metastatic cases, including age, gender, previous tumor history, affected site, treatment, interval of diagnosis between primary tumor and metastasis, the diagnosis time of other systemic metastases, and outcomes, were obtained from electronic medical records. Pathologic materials of metastatic carcinomas were reviewed and compared with primary tumors. No original diagnosis was regarded as incorrect after reviewing hematoxylin and eosin stained and immunohistochemical stained slides of these tumors.
Statistical analysis was performed using the SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). The Mann-Whitney U test was used to compare the time interval from primary tumor detection to oral metastases between pulmonary and non-pulmonary origins, and to compare the survival time after oral metastases between pulmonary and non-pulmonary origins. The Fisher's-exact test was used to compare the incidence of gingival and mandibular metastasis between pulmonary and hepatic origins. Differences were considered significant for p-values of <0.05.
RESULTS
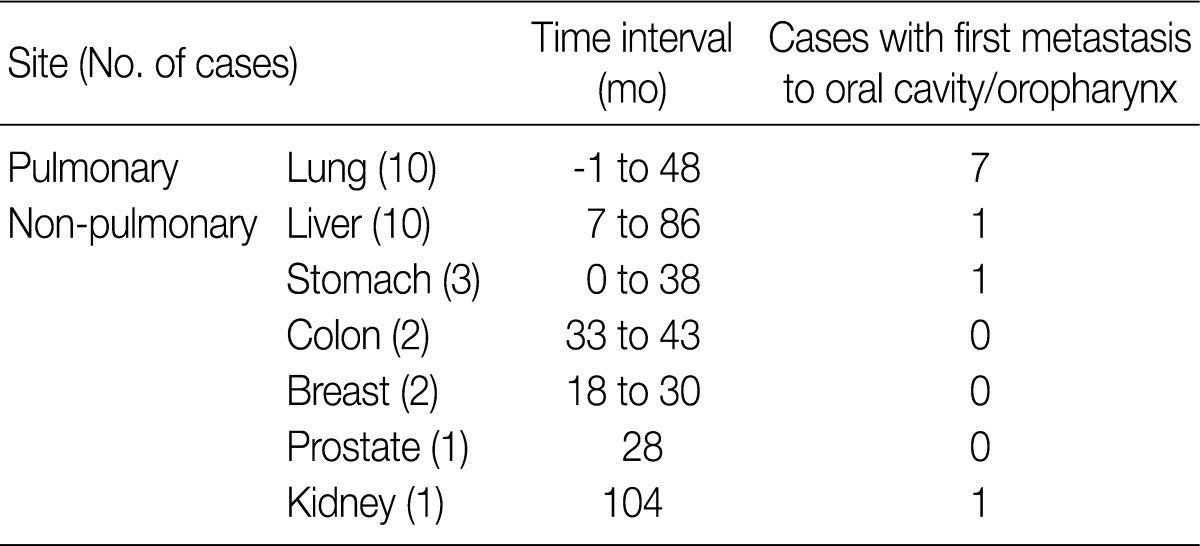
Twenty nine cases of oral/oropharyngeal metastases were retrieved, comprising 2.0% of 1,445 malignancies. The mean age of the patients at the time of oral/oropharyngeal metastases was 64.8 years, ranging between 40 and 85 years. There was a significant predominance of males at about a 5:1 ratio (24 male and 5 female patients). The histological features of most metastatic carcinomas were similar to those of primary tumors (Fig. 1A-C), however, some cases showed non-specific histological features such as scattered atypical cells (Fig. 1D). In 15 cases, immunohistochemical staining was needed to make a diagnosis (Fig. 1E-H). The most common primary sites among patients were the liver (10 cases, 34%) and lung (10 cases, 34%), followed by the stomach (3 cases, 10%), colon (2 cases, 7%), breast (2 cases, 7%), prostate (1 case, 3%), and kidney (1 case, 3%). For females, the commonest primary site was the breast (2 cases), followed by the lung (1 case), stomach (1 case), and colon (1 case). All oral/oropharyngeal metastases from the liver, prostate, and kidney were diagnosed in males in our patient group (Table 1).

Histological and immunohistochemical features of metastatic tumors. (A-C) Metastatic carcinomas are similar to those of primary tumors. (A) Metastatic adenocarcinoma of colonic origin. (B) Metastatic clear cell renal cell carcinoma. (C) Metastatic invasive ductal carcinoma. (D) Scattered atypical cells are identified in stroma that are diagnosed as metastatic hepatocellular carcinoma. (E, F) Immunostaining for hepatocytes demonstrates strong positivity, consistent with metastatic hepatocellular carcinoma (E, H&E; F, hepatocyte immunostain). (G, H) Immunostaining for thyroid transcription factor-1 (TTF-1) demonstrates strong positivity, consistent with metastatic adenocarcinoma from a primary lung tumor (G, H&E; H, TTF-1 immunostain).

Primary sites, histologic types, and metastatic subsites of tumors metastatic to the oral cavity and oropharynx (n=29)
The most common metastatic subsite was the gingiva (10 cases), followed by the tonsil/pillar (6 cases), mandible (4 cases), tongue (2 cases), tongue base (2 cases), hard palate (2 cases), mouth floor (1 case), buccal mucosa (1 case), and tongue and gingiva (1 case). One patient with HCC had two metastatic masses in the gingiva and tongue simultaneously (Table 1). Five out of 10 liver cancers metastasized to the gingiva, while only 2 out of 10 lung cancers metastasized to the gingiva. Among 4 cases of mandibular bone metastasis, 3 cases came from the lung, and 1 case came from the liver. A disparity between the metastatic subsites of lung and liver primary tumors did exist, but this did not reach a statistical significance (Fisher's-exact test, p=0.19).
Symptoms of oral/oropharyngeal metastases were non-specific and included foreign body/mass sensation (21 cases), pain (5 cases), and bleeding (3 cases). Most metastatic carcinomas were diagnosed after primary tumor detection, except for one case of tonsillar metastasis that was discovered one month earlier than the primary tumor, which was a neuroendocrine carcinoma of the lung. The intervals between detection of primary tumors and oral/oropharyngeal metastases were variable (range, -1 to 104 months). As one of the shortest examples, 2 cases of metastatic adenocarcinomas from the stomach and lung were both found simultaneously with the primary tumor. Lung cancers generally showed faster oral/oropharyngeal metastases than other tumors. The differences in the time intervals from primary tumor detection to oral metastases between pulmonary (median, 35 days) and non-pulmonary origins (median, 549 days) had statistical significance (p=0.004).
Ten patients (34%) with metastases from the lung (7 cases), liver (1 case), stomach (1 case), and kidney (1 case) manifested with oral/oropharyngeal metastases as a first sign of a systemic metastasis (Table 2). In the remaining 19 patients, systemic metastases in the bone (especially the spine), brain, lung, liver or adrenal gland preceded or accompanied the oral/oropharyngeal metastases. Patients received wide excision (5 cases), chemotherapy (14 cases) and/or radiotherapy (7 cases) for the treatment of oral/oropharyngeal metastatic tumors. Three patients received only supportive care.
The clinical outcomes for most patients with oral/oropharyngeal metastases were poor. Twenty-five patients (86%) died within one year of developing oral/oropharyngeal metastases. In addition, and for unexplained reasons, the survival time after detection of oral/oropharyngeal metastases was significantly different between those of pulmonary (median, 212 days) and non-pulmonary origins (median, 55 days) (p=0.008). Only 3 patients with HCC (2 cases) or a renal cell carcinoma (1 case) were alive at the time of writing, and one of these individuals shows no evidence of disease for 68 months after wide excision of a tonsilar metastasis of HCC.
DISCUSSION
Because of the rareness of oral/oropharyngeal metastases, their diagnosis is challenging for both the clinician and the pathologist. An awareness of the incidence, common primary site, common metastatic subsite, and metastatic course or pattern is helpful in diagnosis of metastatic carcinomas. Reports on metastatic carcinomas of the oral cavity from various origins have consisted mainly of isolated cases or small series.3,4 In addition, the knowledge that is based on isolated cases might possess some bias because the cases could comprise more unusual tumor types or manifestations. Studies on metastatic oral/oropharyngeal cancers from one institute have not been published in Korea, except for the report by Roh et al.,5 which reported 6 cases (0.05%) of head and neck metastases among 12,602 patients with HCCs, who are not included in the present collection.
According to some metaanalyses, the gender distribution of oral metastases is either predominantly male (Hirshberg et al.,3 approximately 2:1, respectively) or almost equal (approximately 1.1:1, respectively).2,4 The latter study included rare primary tumors of the female genital organs (choriocarcinoma, leiomyosarcoma, germ cell tumor, etc.). In our present study, there was a significant male predominance. In the Western literature, the most commonly reported primary site is the lung for males and the breast for females.2,3 In a Korean study, Lim et al.4 determined that the most common primary site for males is the liver. We also observed that the liver was the most common primary site and that HCC was the most common primary tumor. This phenomenon could be attributed to the high incidence of HCC in Korea. However, considering the rarity of oral metastasis of stomach cancer, which is the most common malignancy in Korea, the affinity for the oral mucosa, especially gingiva, of HCC could not be ignored. However, the 0.05% incidence of HCC metastasising to the upper aerodigestive tract is difficult to estimate as either high or low, since there are no such statistics on other tumors.5
Most carcinomas may spread via lymphatics or hematogenous routes. The mechanism of most oral/oropharyngeal metastases is through hematogenous dissemination. Understandably, the liver and the lungs are the most frequently involved organs in hematogenous dissemination. Gastrointestinal carcinomas preferentially metastasize hematogenously to the liver. In our current study, all patients with stomach and colon cancers had hepatic metastasis before or simultaneously with oral metastases. Hematogenous routes to the oral/oropharyngeal area are through the cava venous system and vertebral venous system.7 Pulmonary carcinomas are of course more likely to develop hematogenous metastases to unusual sites via the cava venous system.6 In our present study, 7 of 10 patients with pulmonary carcinoma manifested with oral/oropharyngeal metastases as a first sign of systemic metastasis, while only 3 of 19 patients with a non-pulmonary carcinoma had shown oral/oropharyngeal metastasis before systemic spread. The improved outcome of pulmonary carcinoma patients with oral/oropharyngeal metastases can be attributed to their less progressed systemic metastasis.
No metastatic sarcomas were identified in our present patient series. Searching the literature revealed that, other than the cases we reported, tumors that showed oral/oropharyngeal metastases include uterine tumors and cervical cancer,8-10 carcinomas of the urinary bladder,11 leiomyosarcoma,12 alveolar soft part sarcoma,13 poorly differentiated carcinoma of the thyroid gland,14 medullary thyroid carcinoma,15 liposarcoma,16 and cutaneous carcinosarcoma.17 There are more published cases of jawbone metastases than of the oral soft tissues.2-4,18,19 However, in this study, mandibular metastases (4 cases) were less common than oral soft part metastases (25 cases). Currently, this phenomenon remains difficult to explain. Among oral soft tissue subsites, the gingiva is the most common site. Malignant cells may be entrapped by the rich capillary network of the gingiva or the hematopoietic marrow of the mandible.
We found three cases of oral/oropharyngeal metastases that were diagnosed either simultaneously or before the primary tumor. Similar findings are noted in the literature. Seoane et al.20 analyzed 39 oral metastases and found that 25% (10/39 cases) of the metastatic tumors had been found before the primary tumors. In these cases, oral/oropharyngeal metastases could be suspected to be primary oral/oropharyngeal tumors. Moreover, symptoms of oral/oropharyngeal metastases are variable and are not pathognomonic. Clinicians often consider these lesions to be a benign lesion such as a granuloma or granulation tissue. Benign looking cysts and an exophytic lesion on the gingiva can be the first sign of metastatic pulmonary adenocarcinoma to the oral mucosa.21,22 Therefore, when an oral lesion is found, even considering a benign condition, a biopsy should be mandatory, especially in patients with a known malignant disease. In addition, pathologists should consider the possibility of a metastatic cancer when examining an oral/oropharyngeal mass, even if the patient does not have a known primary tumor. The histopathological features of the oral metastasis could provide a clue as to the origin of note, however some oral/oropharyngeal metastases can mimic primary oral tumors. Primary ductal carcinoma of the salivary gland and metastatic breast carcinoma, or primary squamous cell carcinoma and metastatic squamous cell carcinoma from the lung may be indistinguishable.23 With an increased alertness by pathologists, appropriate diagnostic methods, including immunohistochemistry, should be carried out and potentially unnecessary medical procedures should be prevented.
Notes
No potential conflict of interest relevant to this article was reported.