Granular Cell Astrocytoma: Report of a Case
Article information
Abstract
We report here a rare case of granular cell astrocytoma. A 75-year-old man was admitted to Inha University Hospital with a three-month history of language deterioration. In a magnetic resonance imaging, a 6.5 cm-sized heterogeneous enhancing mass was seen in both the frontal lobes and the anterior genu of the corpus callosum. A stereotactic biopsy was performed. The tumor was composed of large and small round cells with abundant intracytoplasmic granules. The nuclei were bland, round to oval, and often eccentrically located. The cytoplasm of the tumor cells was positive for glial fibrillary acidic protein and S-100 protein.
Granular cell astrocytoma (GCA) is a very rare tumor, arising in the cerebral hemisphere and, rarely, in the cerebellum. It was first described by Markesbery et al.1 in 1973 as a granular cell tumor (GCT) in the central nervous system. The tumor was found to be a highly aggressive neoplasm, which is contrary to the benign nature of GCT in other parts of the body. Furthermore, the tumor was positive for glial fibrillary acidic protein (GFAP) and was considered a rare variant of glial neoplasm with granular cell changes,2 the so called GCA. We report a case of GCA in a 75-year-old man in order to discuss its intraoperative smear cytology, morphologic spectrum and immunoreactivities.
CASE REPORT
A 75-year-old man was admitted to Inha University Hospital with a three-month history of language deterioration. He was also presenting gait disturbance and urinary and fecal incontinence. He had an eight-year history of hypertension and had undergone stent insertion for myocardial infarction five years previously. In computed tomography (CT) and magnetic resonance imaging, a 6.5 cm-sized heterogeneous enhancing mass with central necrosis was seen in both the frontal lobes and the anterior genu of the corpus callosum. Radiologically, the mass was suspected to be lymphoma or glioblastoma multiforme, and a stereotactic biopsy was therefore performed. A piece of the biopsy sample was sent for frozen section evaluation. The cytologic crush material was composed mainly of large single cells with indistinct cytoplasmic borders in a granular background. The tumor cells had abundant eosinophilic granular cytoplasm and round oval nuclei with prominent nucleoli. Some tumor cells with mild nuclear atypia were also discerned (Fig. 1). No endothelial proliferation or mitosis was identified.
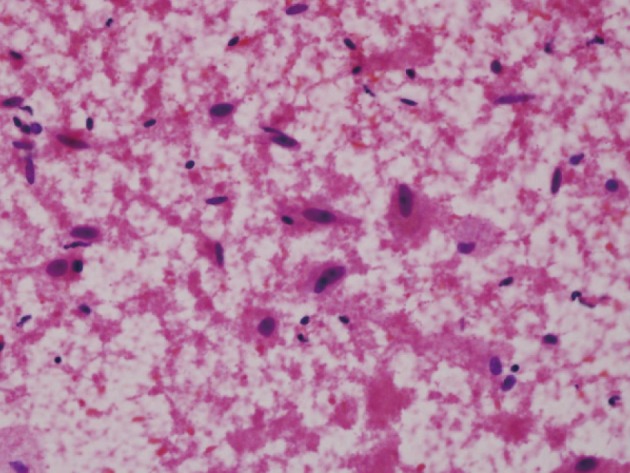
The squash preparation shows scattered large granular tumor cells with oval nuclei in an eosinophilic granular background.
The biopsy samples for permanent section consisted of three pieces of brain tissue. They showed cellular lesions predominantly composed of infiltrates of large round cells without endothelial proliferation. Reticulin deposition was seen only in the endothelial cells. The tumor cells had abundant intracytoplasmic eosinophilic granules, either dispersed uniformly or confined to the cell periphery (targetoid appearance) (Fig. 2). The granules were positive for periodic acid-Schiff (PAS) and resistant to diastase digestion. The nuclei were bland, round to oval, varied in size and often eccentrically located. Occasionally, mild atypical nuclei and small nucleoli were observed. In the entire field, no mitosis or necrosis was identified.
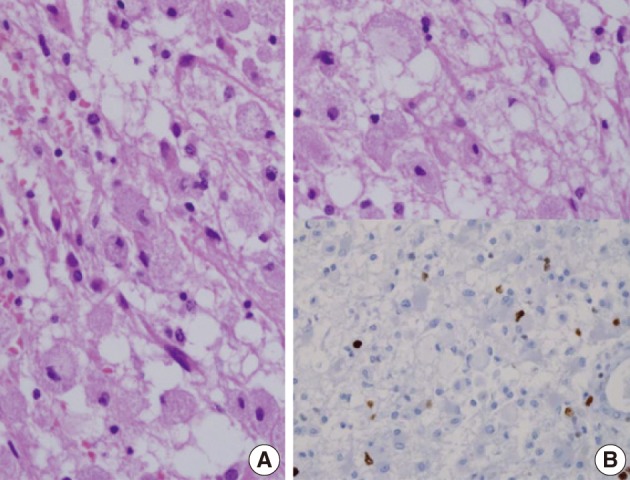
The large tumor cells have abundant intracytoplasmic granules, uniformly distributed or confined to the cell periphery (A), and the Ki-67 labeling index is approximately 5% (B).
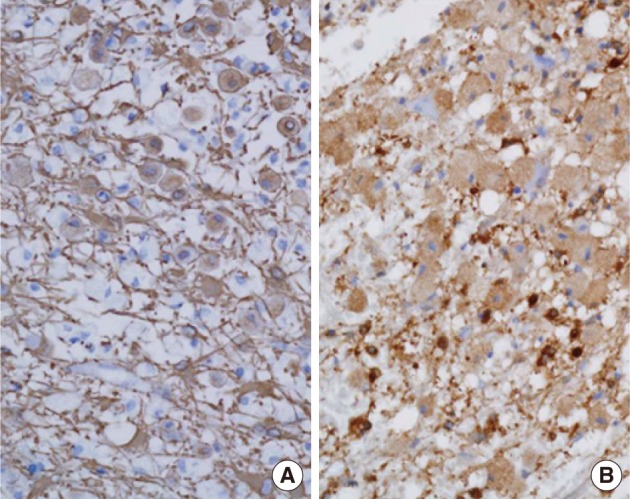
The granular cells were diffusely and strongly immunoreactive with GFAP showing cytoplasmic staining and targetoid appearance. The S-100 protein showed diffuse strong cytoplasmic immunoreactvity (Fig. 3). The tumor cells overexpressed the p53 protein and showed positive immunoreactivity for CD68 (KP), but were negative for CD68 (PGM). Epithelial membrane antigen (EMA), lysozyme, CD43, and albumin were not expressed. The Ki-67 labeling index was 5%. The patient was discharged without additional management.
DISCUSSION
GCT were first described by Abrikossoff in 1926.1 It is now generally accepted that the origin is from the Schwann cell, based primarily on S-100 positivity. GCT has been seen in innumerable locations; the tumor cells are large and their cytoplasm is highly granular. The large majority of the granular tumors pursue a benign clinical course.1 However, GCAs are a distinctive morphologic variant of infiltrative astrocytomas characterized by large, atypical, PAS-positive granular cells featuring GFAP immunopositivity.2-7
The intraoperative frozen diagnosis of GCA is challenging and should be distinguished from a reactive condition. The cytologic features of GCA were described in only one report in the literature.7 Arvanitis et al.7 asserts that the cytologic crush presentation was composed of small cells with indistinct cell borders and large cells with abundant eosinophilic granular cytoplasm. Our case study showed mainly large cells with abundant eosinophilic cytoplasm. The previous case showed a mild nuclear pleomorphism and endothelial proliferation. The latter case showed mild nuclear atypia and prominent nucleoli.
GCA is confused with reactive conditions such as multiple sclerosis, progressive multifocal leukoencephalopathy, and infarction, because the granular cells resemble macrophages. GCAs not only show a significant degree of nuclear enlargement and atypia but often also show prominent eosinophilic nucleoli, features not typical of macrophages in reactive central nervous system lesions.3 Also, the presence of a conventional infiltrating astrocytoma component and tumor cells that are larger than macrophages is helpful to distinguish GCA from other conditions. Finally, granular cells have granular cytoplasm packed with eosinophilic PAS-positive lysosomes. In this case, the granular cells were PAS-positive and larger than macrophages, and, occasionally, mild atypical nuclei and small nucleoli were observed.
GFAP-positive cells having a targetoid appearance are the most characteristic, and the granular cells also show positive immunoreactivity for EMA, S-100 protein, and CD68 in most cases.3 In the current case, the tumor cells exhibited positive immunoreactivity for GFAP, S-100 protein and CD68 but were negative for EMA. Furthermore, the tumor cells over expressed the p53 protein. Rickert et al.2 reported p53 positivity in 6/9 cases.
The clinical course of GCA is known to be very aggressive. A study of 22 cases of GCA reported that the patients' survival duration was less than one years.4 Although this tumor could be of any grade, from World Health Organization (WHO) grade II to IV, the prognosis for this subtype is worse than that for conventional infiltrative astrocytomas. In the present case, the nuclear atypia was mild and there was neither necrosis nor endothelial proliferation. Mitosis was not identified. According to the 2000 WHO criteria, the tumor was grade II. However, there is a possibility of a higher grade because of the presence of necrosis in CT, and because the diagnosis was conducted by biopsy and not by surgical resection.
In conclusion, we report a case of GCA, which is a rare variant of astrocytoma; the GFAP positivity and other immuno-markers all suggest that GCAs are of an astrocytic nature.
Acknowledgments
This work was supported by Inha University Research Grant.
Notes
No potential conflict of interest relevant to this article was reported.