Rosai-Dorfman Disease in the Breast with Increased IgG4 Expressing Plasma Cells: A Case Report
Article information
Abstract
Rosai-Dorfman disease (RDD) can present in any anatomic site, but breast involvement is rarely reported. Recently, a relationship between RDD and IgG4-related sclerosing disease has been suggested. Here we report another case of RDD with overlapping features of IgG4-related sclerosing disease occurring in a right breast of a 62-year-old female. On microscopic examination, the mass demonstrated a characteristic zonal pattern of proliferation of large polygonal histiocytes and lymphoplasma cells with stromal fibrosis. Emperipolesis was observed in histiocytes with abundant cytoplasm, which showed immunoreactivity for S-100 protein and CD68; the diagnosis of RDD was made. Sheets of plasma cells in the fibrotic stroma demonstrated positive reactions for IgG and IgG4. The mean count of IgG4-positive plasma cells was 100.2/high power field, and the ratio of IgG4/IgG was 56.7%. Additional findings of stromal fibrosis and obliteration of preexisting breast lobules suggested overlapping features with IgG4-related sclerosing disease.
Rosai-Dorfman disease (RDD) is a proliferative lesion of histiocytes and its etiology has not been elucidated.1 It usually shows a self-limiting clinical course but rare fatal cases with systemic involvement have been reported.1,2 The characteristic histologic finding in the lymph node is dilatation of sinuses filled with numerous histiocytes accompanied by lymphoplasma cell infiltrates. The large polygonal histiocytes have voluminous eosinophilic cytoplasm and various inflammatory cells are trapped within the cytoplasm, so-called emperipolesis. The histiocytes express S-100 protein in addition to a classic macrophage marker, CD68.
IgG4-related sclerosing disease is an idiopathic chronic inflammatory disease characterized by an elevated serum IgG4 level, tissue infiltrates of IgG4-secreting plasma cells, and various degrees of fibrosis often associated with obliterative phlebitis. IgG4-related sclerosing disease was originally described in autoimmune pancreatitis; since then, its involvement of various organs as a systemic disease has been reported.3
Although RDD has primarily been described in the lymph node, extranodal cases make up nearly half of the reported cases. Rarely, RDD presents as a mass lesion in a breast; 26 cases have been reported in the English literature to date.4 Recently, it has been reported that a high proportion of plasma cells in RDD, especially in extranodal RDD, expresses IgG4, and a relationship between RDD and IgG4-related sclerosing disease has been suggested.5-8 Herein, we report a case of RDD presenting as a palpable mass in a female breast. This case exhibited characteristic histiocyte proliferation as well as diagnostic findings of IgG4-related sclerosing disease including fibrotic stroma and numerous IgG4-expressing plasma cell infiltrations, suggesting that there is a relationship between these two rare idiopathic chronic inflammatory diseases.
CASE REPORT
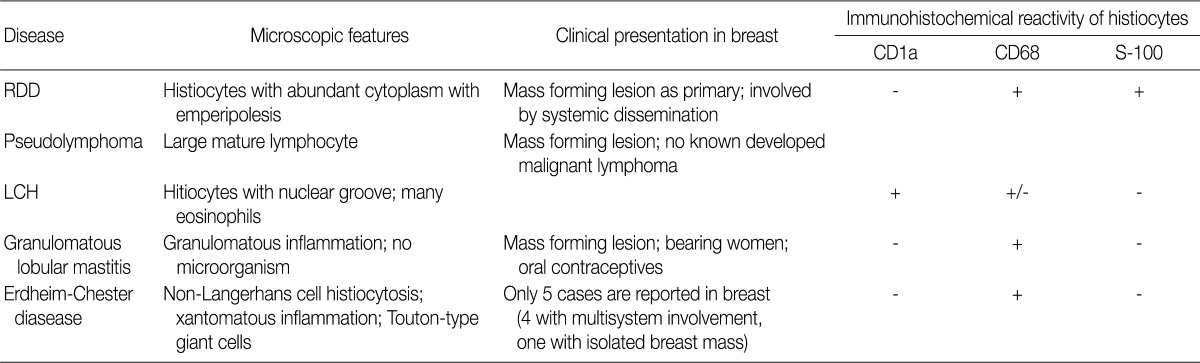
A 62-year-old woman presented with a palpable mass in the right breast. Mammography (Fig. 1A) and ultrasonographic evaluation demonstrated a hyperechoic nodule in the right lower portion. Radiology suggested the diagnostic possibility of a benign lesion such as fat necrosis. A needle biopsy of the breast nodule was performed, and the following diagnosis was made: "prominent aggregation of foamy histiocytes associated with diffuse infiltration of lymphoplasma cells, neutrophils, and lymphoid follicles." The possibility of xanthogranulomatous mastitis, plasma cell mastitis, and the like was suggested. Periodic acid-Schiff staining with prior diastase treatment (D-PAS) and Ziehl-Neelsen staining for identifying microorganisms were all negative. Cytokeratin staining for epithelial lesions was totally negative.
Mammography revealing an ill-defined mass in the right lower breast (A). Numerous histiocytes showing pink, abundant cytoplasm (B) containing intact inflammatory cells (emperipolesis, arrows) (C). Nuclear and cytoplasmic S-100 protein expression of histiocytes highlighting the entrapped inflammatory cells in their cytoplasm, which are negative for S-100 protein (D). Histiocytes expressing CD68 in cytoplasm (E).
Six months later, a follow-up sonographic examination showed no changes in the size or echo-density of the nodule. Axillary lymphadenopathy was absent. The skin of the overlying area showed inflammatory change, and the patient underwent surgical excision.
The excised specimen was a lump of breast tissue. It was firm in consistency, and a 2.8 cm×2.5 cm ill-defined lobulated mass-like lesion was found on sectioning.
Microscopic examination revealed dense lymphoplasmacytic infiltration in the mass-forming area. Fibrosis and histiocytic infiltrates in a storiform fashion were observed under low-power microscopic examination. Most breast parenchyma was replaced by histiocytes, inflammatory cells, and fibrosis, and these inflammatory cell infiltrates extended into the adjacent fat tissue (Fig. 1B). Diffusely scattered lymphoid follicles were found. Obliterative phlebitis was not present.
The most prominently recognizable cells were histiocytes with large vesicular nuclei and abundant, clear cytoplasm. Furthermore, some of the histiocytes had intact lymphocytes, plasma cells, and red blood cells within the cytoplasm (Fig. 1C). The infiltrating histiocytes showed strong immunoreactivity for S-100 protein (1:2,000, polyclonal, Dako, Carpinteria, CA, USA) in their nuclei and cytoplasm (Fig. 1D). CD68 (1:100, clone PGM1, Dako) on the histiocytes demonstrated a granular cytoplasmic staining pattern (Fig. 1E). CD21 (1:50, clone 1F8, Dako) highlighted a follicular dendritic cell meshwork in the scattered germinal centers of reactive lymphoid follicles.
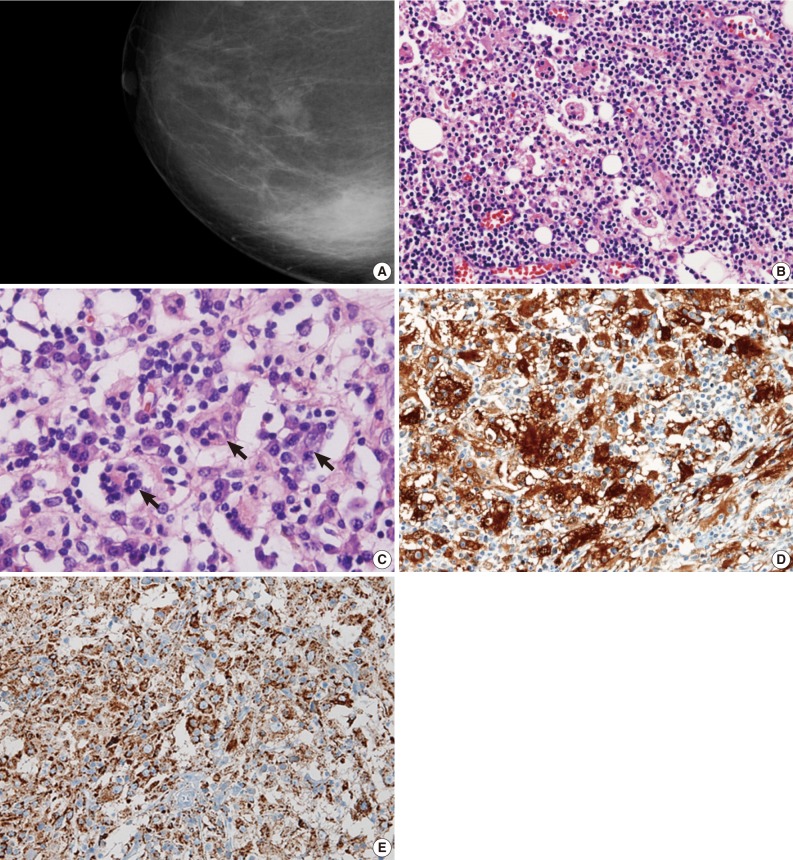
Immunohistochemical staining for IgG (1:200, clone A57H, Dako) and IgG4 (1:200, clone HP6025, Invitrogen, Carlsbad, CA, USA) (Fig. 2) revealed a high proportion of plasma cells in the stroma. IgG4- and IgG-positive plasma cells were estimated by counting the most significantly infiltrative areas. More specifically, the number of IgG4- and IgG-expressing plasma cells in five high power fields (HPF) were counted, added together, and then divided by 5 to obtain the mean count. The IgG4/IgG ratio was also calculated from the mean count of IgG4 and IgG.
Normal breast lobules are not identifiable due to sclerotic, fibrous stroma (A). Many IgG-expressing plasma cells (B) also showing reactivity for IgG4 (C).
Since the surgical excision, the patient has been in good general condition without a recurrent mass lesion in the breast for more than 10 months. Serum IgG and IgG4 levels were not evaluated before or after the excision. She has visited for follow-up, including a regular sonographic examination of her treated breast, every 6 months since the excision. No further treatments, such as steroid therapy, have been conducted, and no other masses have been detected.
DISCUSSION
RDD was initially described as sinus histiocytosis with massive lymphadenopathy.1 It usually presents in children and young adults with bilateral cervical lymphadenopathy, and shows typical histologic features, including fibrosis, marked dilatation of sinuses with mixed inflammatory cells, and numerous histiocytic infiltration.9 In particular, infiltrating histiocytes have one large nucleus, conspicuous central nucleoli, and abundant clear and/or acidophilic cytoplasm. Emperiopolesis of lymphocytes, plasma cells, and red blood cells by large histiocytes is evident. Immunohistochemically, the histiocytes show reactivity for S-100 protein and CD68, which is helpful to verify the diagnosis of RDD. Extranodal manifestations can be present in any part of the body, including the breast. Compared to nodal RDD, extranodal RDD demonstrates more fibrosis, infrequent typical histiocytes, and a lesser degree of emperipolesis. To the best of our knowledge, 26 cases of RDD in the breast have been reported in the English literature,4 and the present case is the first report in Korea.
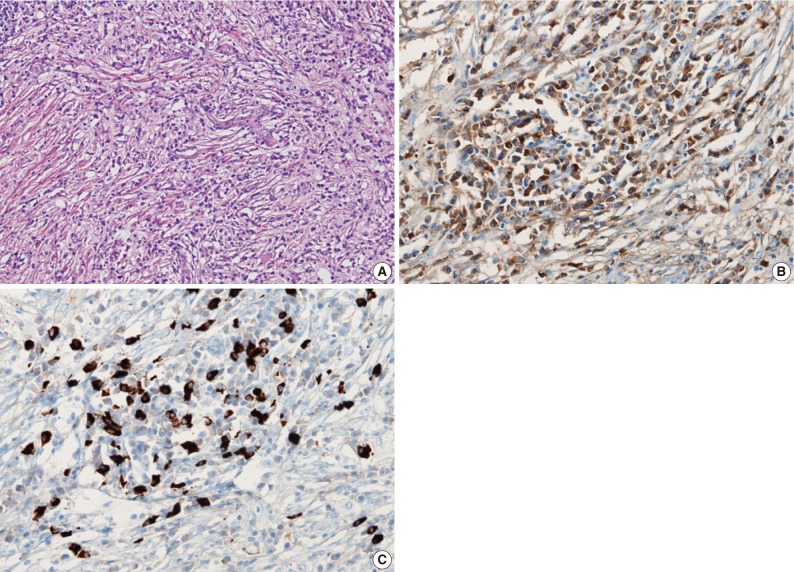
Mass-forming lesions in breast, as manifestations of inflammatory infiltration, are occurred in variable diseases. With hitiocytic infiltration, several differential diagnoses can be considered, including Langerhans' cell histiocytosis, granulomatous lobular mastitis, extranodal RDD, and Erdheim-Chester disease, which are summarized in Table 1.
Previously reported breast RDDs have included mammary manifestation of systemic RDD as well as primary RDD in mammary parenchyma and subcutis. In one case of mammary manifestation of systemic RDD, the patient had a history of RDD in the thigh and inguinal lymph node, and a mammary lesion consisting of numerous tiny nodules measuring up to 0.5 cm was found during routine screening.10 Primary RDDs of breast have been found in women of various ages, presenting as a painless, palpable mass for a few months duration.4 They were initially regarded as malignancies clinically and radiologically, and in all cases, excision or core needle biopsies were performed for diagnostic treatment. Among reported 26 cases, 3 patients had local recurrence ranging from 5 months to 2.5 years, and 1 died of disseminated RDD after 2 months post-operation. To date, all reported cases of RDD have shown characteristic histological findings. None of them exhibited IgG and/or IgG4 immunohistochemical staining for infiltrating plasma cells. Our case showed storiform sclerosing fibrosis with plasmacytic infiltration, rendering obliteration of preexisting normal breast lobules. These features somewhat overlap with IgG4-related sclerosing disease. More than 50 IgG4+ plasma cells/HPF or over 40% IgG4/IgG can be considered highly specific diagnostic criteria for IgG4-related sclerosing disease.3
Recently, both secondary breast involvement of a systemic IgG4-related sclerosing disease and primary IgG4-related sclerosing mastitis have also been reported.3
Five cases of primary IgG4-related sclerosing disease of the breast have been reported in the English literature.11,12 Ogiya et al.8 reported the first such case; the patient suffered from bilateral swelling of the breast and elevated serum IgG4, and was successfully treated by steroid therapy.11 Cheuk et al.11 subsequently described four cases of IgG4-related sclerosing disease in the breast, and proposed the term IgG4-related sclerosing mastitis.12 In that report, the patients presented with painless masses in the breast, and underwent surgical excision without recurrence. Compared with lymphocytic mastitis and granulomatous mastitis, IgG4-related mastitis shows denser IgG4+ plasmacytic infiltration (272-495/HPF) with higher IgG4/IgG ratios in the range of 49-85%.
A possible link between RDD and IgG4-related sclerosing disease has been suggested because they have some overlapping histological features. In 2009, Kuo et al.10 described a cutaneous RDD with numerous IgG4-positive plasma cells, which was the first report of overlapping findings between the two diseases.5-7,13 Plasmacytic infiltration is a relatively consistent finding in RDD, and fibrosis is also common in extranodal cases. Our case also demonstrated features of IgG4-related sclerosing lesions such as fibrosis and many IgG4-positive plasma cells in the lesion in addition to the typical histological findings of RDD. In the present case, the mean count of IgG4-positive cells was 100.2/HPF, and the ratio of IgG4-positive plasma cells to IgG-positive plasma cells was 56.7%, which met the diagnostic criteria of IgG4-related sclerosing disease histologically. To the best of our knowledge, this is the first case of RDD in the breast associated with prominent IgG4-positive plasmacytic infiltration and fibrosis.
Although the diagnostic criteria of IgG4-related sclerosing disease are established, diagnosis should be made carefully, considering clinical, laboratory, radiologic, and histological features. IgG4-related sclerosing disease is now considered an immunity matter, and steroid therapy is known to be effective. Some authors have suggested that steroid therapy, which is now considered the choice of treatment for IgG4-related sclerosing disease, could be a useful treatment modality for RDD with features of IgG4-related sclerosing disease.6 To clarify the pathogenic relationships between these two diseases, comprehensive studies that consider clinical, laboratory, radiologic, and histopathologic features are required.
Notes
No potential conflict of interest relevant to this article was reported.