Cellular Pseudosarcomatous Fibroepithelial Stromal Polyp of the Vagina during Pregnancy: A Lesion That Is Overdiagnosed as a Malignant Tumor
Article information
Abstract
Fibroepithelial stromal polyp (FSP) is a benign lesion that can occur at various sites, including the lower female genital tract. In rare cases, however, it may exhibit hypercellularity, bizarre cytomorphological features, and atypical mitoses resulting in an overdiagnosis as a malignant tumor despite its benign clinical course. Recently, we experienced one case of a 30-year-old pregnant woman with cellular pseudosarcomatous FSP that was initially diagnosed as a malignant fibrous histiocytoma at a primary clinic. In addition to describing the rare features of this case, we wish to increase awareness about this benign lesion which will be essential for avoiding unnecessary radical surgery or chemoradiation treatment.
Fibroepithelial stromal polyps (FSPs) are unusual benign lesions that occur in the vagina,1,2 vulva,3 endometrium, cervix,4 and genitourinary tract.5 Although FSPs of the lower female genital tract have been well-recognized since their initial description,6 they still cause diagnostic difficulties mainly owing to their variable histological appearances and rarity. Nucci et al.2 described a subset of FSPs designated as cellular pseudosarcomatous FSPs that are histologically characterized by stromal hypercellularity, cytological atypia, and increased mitoses. The presence of strikingly atypical histological features within the polyp may frequently lead to its misdiagnosis as a sarcoma. Many cases in the literature were associated with pregnancy, suggesting that stromal changes can be induced by hormones. Recently, we experienced a case of a 30-year-old pregnant woman with cellular pseudosarcomatous FSP in the vagina that was initially diagnosed as a sarcoma. Herein, we describe the histological and immunohistochemical findings of a cellular pseudosarcomatous FSP with a review of the literature to emphasize the fact that the presence of atypical stromal cells accompanied by frequent abnormal mitoses does not necessarily indicate a malignant tumor, especially in pregnant women.
CASE REPORT
A 30-year-old, previously healthy, pregnant woman was found to have a polypoid protruding mass in her vaginal wall during a routine antenatal examination at 30 weeks of gestation. The mass was ovoid, measuring approximately 3.0 cm in its greatest dimension, soft to rubbery in consistency, and had a smooth external surface. It was attached laterally to the vaginal mucosa with a short stalk. Neither the patient nor the obstetrician was aware of the onset of the mass. The mass was resected at the time of delivery at an outside hospital and was histologically diagnosed as a sarcoma. The patient visited our hospital to confirm the diagnosis and undergo further treatment. On gynecological examination, we did not find any residual mass and other abnormalities on a whole-body positron emission tomography scan.
Grossly, the soft polyp measured 3.0×1.6×1.2 cm. Histologically, the mass was covered with the squamous epithelium of the vagina (Fig. 1A). The stromal component was focally edematous and hemorrhagic near the overlying mucosa, and showed variable cellularity from area to area (Fig. 1A). The peripheral portion showed less cellularity compared with the central portion, and the stromal component showed markedly increased cellularity, nuclear pleomorphism, and numerous atypical mitoses (more than 3/high power field) (Fig. 1B). The cells formed short, intersecting fascicles mimicking a smooth muscle tumor or a malignant fibrous histiocytoma, and featured abundant pale cytoplasm with prominent nucleoli and coarse chromatin. Scattered stellate, bizarre multinucleated giant cells extending to the overlying mucosa were also observed. Capillaries, polymorphonuclear leukocytes, and lymphocytes were intermixed with the stromal cells.
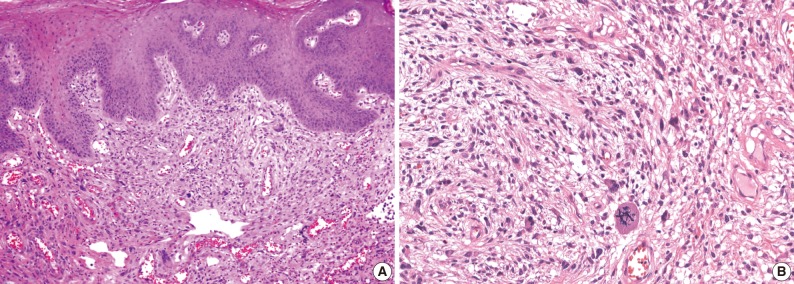
Microscopic findings of a cellular pseudosarcomatous fibroepithelial stromal polyp. (A) This fibroepithelial polyp of the vagina shows a single pedunculated mass covered with squamous epithelium. The stromal component shows variable cellularity from area to area. The subepithelial stroma is composed of atypical spindle cells with abundant blood vessels. There are also scattered stellate, bizarre multinucleated giant cells extending into the overlying mucosa. (B) The tumor cells of the pseudosarcomatous area show abundant pale cytoplasm with prominent nucleoli, coarse chromatin, nuclear pleomorphism, and numerous atypical mitoses.
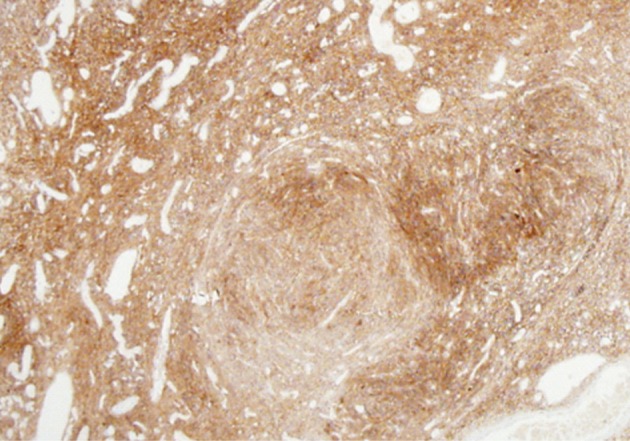
Immunohistochemically, the stromal cells were diffusely and strongly positive for vimentin (1:200, Zymed, San Francisco, CA, USA), CD10 (1:50, Novocastra, Newcastle, UK) (Fig. 2) and the progesterone receptor (PR; 1:200, Neomarkers, Fremont, CA, USA), as well as focally positive for α-smooth muscle actin (SMA; 1:500, Dinova, Seoul, Korea). However, the stromal cells were negative for the estrogen receptor (ER; 1:200, Neomarkers), desmin (1:200, Dako, Glostrup, Denmark), S-100 protein (1:500, Zymed), and CD34 (1:500, Immunotech, Marseille, France). The Ki-67 labeling index (1:200, Zymed) was significantly higher in the centrally located hypercellular area (approximately 60%) than in the less cellular stroma (approximately 10%) at the periphery.
DISCUSSION
Current studies indicate that pseudosarcomatous cellular FSP in the lower female genital tract includes lesions previously reported as pseudosarcoma botryoides as well as fibroepithelial polyps with atypical stromal cells. These polyps characteristically have atypical stromal cells with or without mitoses or atypical mitoses. Similar to pseudosarcomatous cellular FSP in the lower female genital tract, such polyps have recently been reported in the renal pelvis5 and cutaneous lesions.6
In a review of the English literature describing such cases (Table 1),2,4,7-16 75 patients aged 15-75 years were diagnosed with pseudosarcomatous FSPs. Of these patients, 19 were pregnant; 53 patients had lesions in the vagina; 14 in the vulva; and 8 in the endocervix. Multiple lesions were observed in 14 patients. Occasional mitoses were present in 28 cases with atypical mitoses. Local excision was used to treat 70 lesions; wide local excision, partial vulvectomy, and biopsy were used to treat each; and incomplete excision was used to treat 2 lesions. Follow-up information with an average duration of 21 months (range, 2.0 to 192 months) was available for 60 patients. During follow-up, 6 lesions recurred locally. Three of the patients with incomplete resection experienced recurrence. Two cases of recurrence were related with recurrent pregnancy; 1 lesion recurred after menopause. None of the lesions that recurred showed locally aggressive behavior. There was no evidence of metastasis in any of the patients.
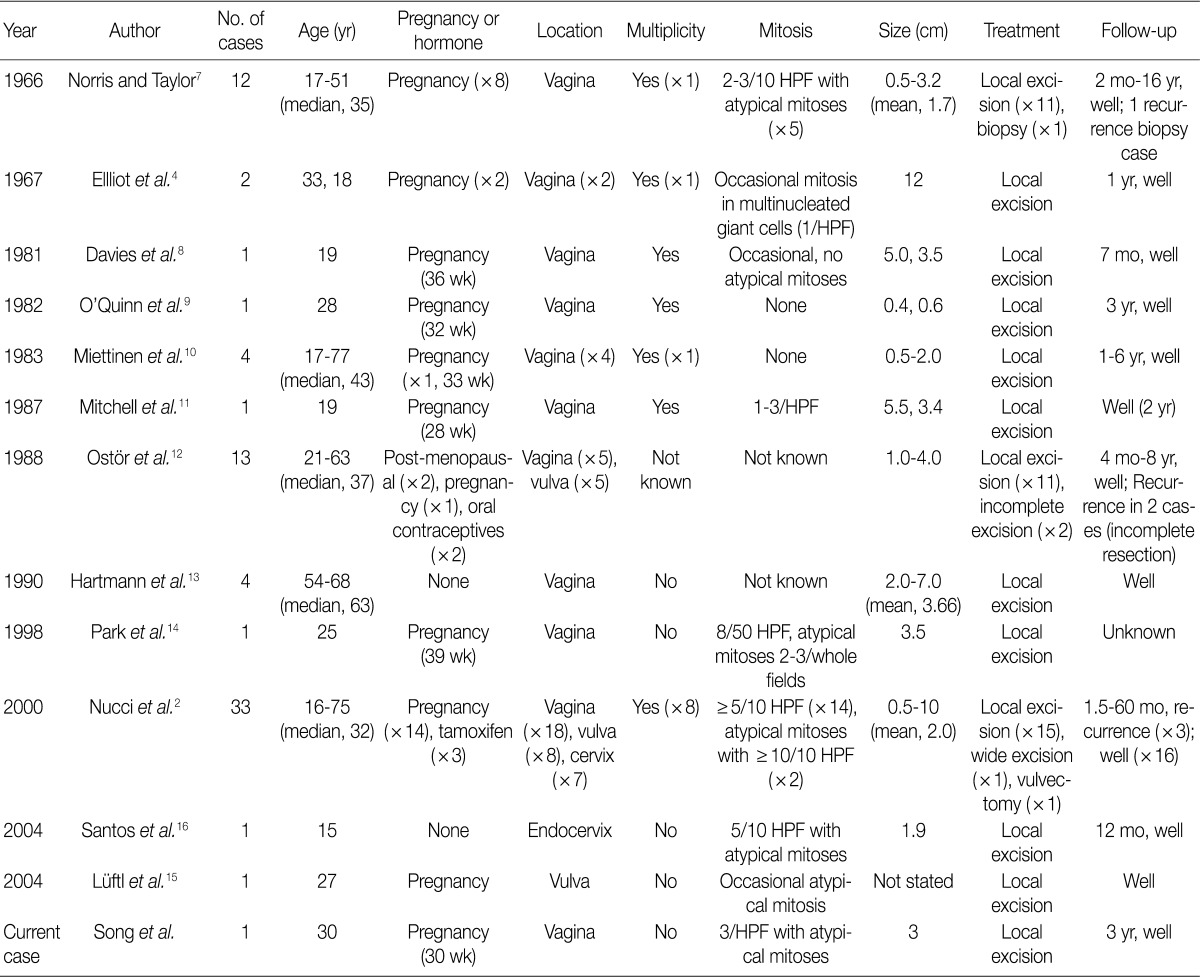
Summary of clinicopathological findings in previously reported cases of pseudosarcomatous fibroepithelial polyp in the female genital tract
Four2,13,14,16 of 12 reports described results of immunohistochemistry performed on the lesions, with all of excised samples showing positive staining for vimentin. Two13,16 of 313,14,16 studies reported immunopositivity for the ER and the PR while 32,13,16 of the 4 studies detailed immunopositivity for desmin. Interestingly, Hartmann et al.13 reported that the patients showing immunopositivity for the ER and the PR were postmenopausal women not receiving hormone replacement treatment.
Although the pathogenesis of FSP is not well understood, it likely represents a reactive hyperplastic process involving the subepithelial stroma rather than a true neoplasm.2 This assertion is based on the fact that these lesions have no clearly defined margins.2 Another hypothesis is based on the finding that the stromal cells of FSPs can express ER and the PR, suggesting that hormonal influences could play a role in the pathogenesis of this lesion.2 Notably, in the study of Nucci et al.,2 14 out of 33 patients were pregnant, while 4 others were taking hormonal agents such as tamoxifen or oral progesterone. In this case report involving a pregnant woman, we observed diffuse immunopositivity, although weakly expressed, for the PR in the entire stromal cell population, corroborating the latter hypothesis.
To our knowledge, there has been no previous report of CD10 immunopositivity in pseudosarcomatous FSPs. Our case showed diffuse and strong immunopositivity for CD10 and focal positivity for SMA, providing evidence of endometrial or mullerian differentiation with smooth muscle differentiation.
In a review of relevant literature, the Ki-67 labeling index was analyzed in 1 study16 and was found to be approximately 30% in non-pregnant 15-year-old women. In contrast, our case showed a very high Ki-67 labeling index (approximately 60% in the cellular area). Intense Ki-67 staining has been linked to malignant transformation.17 Although a high Ki-67 labeling index is definitely a sign of possible malignant transformation, based on the clinical course and the disease entity, however, we think that this phenomenon represents a pregnancy-related hormonal change rather than malignant transformation. Therefore, overdiagnosis of FSPs as a malignant tumor should be avoided by taking into account the the high Ki-67 labeling index that is observed in this case.
Moreover, cellular pseudosarcomatous FSPs should be distinguished from sarcomas, including leiomyosarcoma, rhabdomyosarcoma, low-grade endometrial stromal sarcoma (ESS), and malignant fibrous histiocytoma. Cellular FSPs can occasionally exhibit a fascicular architecture, which, in combination with an increased mitotic rate, atypical cells, and/or atypical mitoses, can be suggestive of leiomyosarcoma. Nevertheless, leiomyosarcomas do not display a clear boundary between the lesional cells and the overlying epithelium, and a polypoid or pedunculated appearance. In addition, the neoplastic cells of leiomyosarcomas tend to exhibit features of smooth muscle differentiation with elongated nuclei in a characteristic "box-car" or "cigar" shape, as well as abundant eosinophilic cytoplasm. Meanwhile, the stromal cells of cellular FSPs are commonly desmin positive2,13,16 and, occasionally, actin positive;16 therefore, the immunophenotype must be interpreted in light of the morphological features on hematoxylin and eosin staining. Moreover, FSPs occasionally show a grape-like or botryoid appearance, mimicking botryoid rhabdomyosarcoma.4 However, the latter occurs in young children, grows rapidly with greater mitotic activities, and shows skeletal muscle differentiation both histologically and immunohistochemically.
With regard to CD10 immunopositivity, differential diagnosis for ESS should be included. Diffuse CD10 immunoreactivity is usually observed in cases of uterine stromal tumors.18 ESS, like cellular FSP, can be polypoid and is characteristically highly vascular. However, the vessels observed in ESS typically resemble spiral arterioles, whereas the vessels observed in cellular FSP are more often variable in size, can be thick-walled, and are often hyalinized. The presence of a central vascular core, which is often observed in cellular FSP, is also lacking in ESS. Although variable amounts of stromal hyalinization can be observed in cellular FSP, thick bands of hyalinized collagen organized in a starburst pattern, a characteristic feature found in some ESSs, are not observed in cellular FSP. In addition, the stromal atypia commonly observed in FSP is not a feature of ESS. Immunoperoxidase staining may be useful in the differential diagnosis given that some ESSs are desmin and/or keratin positive in a dot-like perinuclear pattern-findings not observed in cellular FSPs.
Furthermore, aggressive angiomyxoma and angiomyofibroblastoma (AMF) are also included as differential diagnoses. Aggressive angiomyxoma is a nonpolypoid lesion that is subcutaneous and typically sizeable by the time it is recognized.1 In addition, it tends to have myoid bundles that cuff the vascular component,2 which is not observed in cellular FSP. AMF has peculiar histomorphological features, including superficial subepithelial location; good margination; multi-patterned growth of uniform, spindled, and stellate-shaped cells; blood vessels of variable sizes; as well as highly collagenous and focally myxoid stroma. The stromal cells of AMF characteristically cluster around the vasculature-a feature that is not prominent in cellular FSP.2 Although plump epithelioid cells and multinucleate cells can be observed in either cellular FSP or AMF, nuclear atypia is usually absent in AMF.2 This distinction between the 2 entities is important, because the sarcomatous transformation of AMF has rarely been reported.19 In the cellular FSP cases in the literature,2 3 patients had local recurrences, but none of them experienced metastasis. Therefore, it is regarded as pseudosarcomatous proliferation of the stromal cells instead of true sarcoma.
In summary, cellular pseudosarcomatous FSP is an under-recognized lesion characterized by bizarre cytological features with numerous atypical mitoses that may lead to its overdiagnosis as a sarcoma. Indeed, an awareness that the disease is a benign lesion rather than a malignant tumor is crucial in order to avoid unnecessary surgical or medical overtreatment. On a final note, our patient did not show any evidence of recurrence or malignant transformation on follow-up, 16 months after the resection of the mass.
Notes
No potential conflict of interest relevant to this article was reported.