Histopathologic Predictors of Lymph Node Metastasis and Prognosis in Tonsillar Squamous Cell Carcinoma
Article information
Abstract
Background
Risk factors for lymph node metastasis in tonsillar squamous cell carcinoma (TSCC) need to be established to determine the degree of surgery required to achieve high curative rates. However, little is known currently about the histopathological features predicting prognosis, specifically in TSCC.
Methods
This study included 53 patients who underwent surgical resection with neck dissection. Clinicopathological factors investigated included age, gender, alcohol use, tobacco consumption, tumor stage, adjacent structure involvement, cell differentiation, squamous dysplasia, in situ carcinoma associated with primary invasive cancer, carcinoma in situ skip lesions, necrosis, invasive front, depth of invasion, and lymphatic, muscle, or perineural invasion.
Results
Contralateral cervical metastasis was associated with higher T stages and soft palate invasion. Lymphatic and muscle invasion were associated with ipsilateral cervical metastasis. Advanced T stage, invasion to the base of tongue, and skip lesions were associated with decreased disease-free survival. Advanced T stage and skip lesions were associated with worse overall survival.
Conclusions
Advanced T stage and soft palate invasion may predict a high risk of contralateral nodal metastasis. T stage and skip lesion are worse prognostic factors in TSCC and should be commented in pathology reports.
Tonsillar squamous cell carcinoma (TSCC) is the most common malignant oropharyngeal cancer, representing 70-80% of all malignancies in this region.1,2 The incidence of TSCC has increased significantly over the last 2 decades, from 0.6 to 1.45 cases per 100,000 people, especially amongst men and adults between 40 and 59 years.3 The clinical course of TSCC is aggressive with frequent local or regional recurrence and early dissemination, consequently, 60-80% of TSCC patients are found to have cervical lymph node metastasis at initial diagnosis.4 Various treatment strategies have been attempted for managing tonsil cancers according to stage and lymph node status, the latter being particularly important because of the need to treat metastatic lymph nodes in oropharyngeal cancers.5 Therapeutic neck dissection or irradiation are the mainstay treatments for nodal metastasis. Elective neck dissection for a clinically node-negative neck remains controversial, even though occult cervical metastasis is estimated to be 24-35%.1,6 Despite advances in surgical procedures and combined modality treatment, the survival of patients with TSCC remains poor with 37% survival at 5 years.3,7 The aggressive behavior of TSCC is not only related to tumor stage, but also lymph node involvement. The resected specimen, therefore, needs to be examined thoroughly to determine whether there is a clinically significant risk of lymph node metastasis that would warrant additional surgery.
Clinical factors associated with adverse outcomes in tonsillar cancers include tobacco and alcohol consumption.8 There have been many studies attempting to predict lymphatic spread based on features of the oral cavity and the primary oropharyngeal cancer.5,9-11 However, those studies included different oropahryngeal cancers with a variety of tumor sites in the oral cavity without focusing on tonsil cancer specifically. As a result, there is still relatively little known about the potential histopathological factors associated with lymph node metastasis and prognosis in TSCC.
The purpose of this study was to determine clinical and histopathological predictive and prognostic factors associated with ipsilateral or contralateral cervical nodal metastasis and survival outcomes in TSCC.
MATERIALS AND METHODS
Patients
This is an retrospective analysis of 53 consecutive TSCC patients who underwent surgical treatment of their primary tonsil lesions with simultaneous neck dissection between January 2000 and August 2008 at the Ilsong Memorial Institute of Head and Neck Cancer, Hallym University Medical Center, Seoul, Korea. Inclusion criteria included the diagnosis of primary TSCC, no prior treatment, complete medical records, and the availability of all histopathological slides of resected specimens.
Clinical information including age, gender, alcohol and tobacco consumption, tumor location, stage, treatment modality, survival and recurrence, together with the involvement of the base of the tongue, soft palate, pterygoid muscle, posterior pharyngeal wall, or nasopharynx, were analyzed using medical records and radiological results. Tumor stage was reclassified based on the 7th edition of the American Joint Committee on Cancer (AJCC). Smoking history was measured in pack-years and was divided into 2 categories based on a 20 pack-years cut off.12 Alcohol consumption was classified into 2 categories based on a 14 drinks per week cut off.12
Postoperatively, 23 patients had no further therapy and 30 patients received adjuvant therapy: 18 received adjuvant radiotherapy and 12 received adjuvant chemoradiation therapy. This study was approved by the Institutional Ethics Committee of Hallym University Medical Center (Seoul, Korea).
Histopathological evaluation
All surgically resected TSCC specimens were serially sectioned and embedded for tumor mapping in the Department of Pathology. The hematoxylin and eosin-stained glass slides were reviewed by 2 pathologists blinded to all clinical information in this study. Pathological features including tumor differentiation, presence of squamous dysplasia adjacent to the tumor, presence of in situ carcinoma connected to the main invasive squamous cell carcinomas (SCC), skip lesions of the in situ carcinoma unconnected with main tumor, intratumoral necrosis, growth pattern of the invasive front, depth of invasion, lymphatic invasion, superior constrictor muscle invasion, perineural invasion, and extracapsular spread in the ipsilateral cervical lymph nodes were analyzed. Positive surgical margin status was considered to be any involvement of squamous dysplasia, carcinoma in situ, or invasive carcinoma. Diagnosis and histological classification were based on the World Health Organization (WHO) classification.13 Depth of tumor invasion was measured from the surface of the mucosa to the maximal depth with an ocular micrometer.14 For exophytic tumors, the measurement was taken from the height of the surface of the adjacent intact mucosa to the deepest point of infiltration.15 Depth of invasion was classified into 2 categories based on a 2 cm cut off, a modification from our prior study.16 The tumor growth pattern at the invasive front was assessed as either cohesive or non-cohesive, the former being a well-defined pushing margin with large tumor islands, and the latter consisting of scattered, small, irregular cords or single tumor cells with a poorly defined infiltrating margin.14,17 Extracapsular spread was defined as carcinoma penetrating the lymph node capsule and infiltrating extracapsular tissue.13
Statistical analysis
The chi-squared test or 2-tailed Fisher exact test were used to determine associations between clinical or pathological variables and ipsilateral or contralateral cervical lymph node metastasis. Disease-free survival was defined as the time from first surgery until documented relapse, including locoregional recurrence and distant metastasis. Overall survival was defined as the time from first surgery until death. All survival times were based on patient status in January 2011. Survival differences among groups were calculated using the Kaplan-Meier method with a log-rank test. The Cox proportional hazards model was used for multivariate analyses of overall and disease-free survival. SPSS ver. 18 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. p<0.05 were considered statistically significant.
RESULTS
Clinical characteristics and their association with cervical nodal metastases
A total of 53 patients (48 men and 5 women) with a median age of 54 years (range, 36 to 75 years) were included in this study. Ten (18.9%) patients underwent elective neck dissection and 43 (81.1%) underwent therapeutic neck dissection. Seventeen (32%) patients were under 50 years of age at the time of diagnosis, and the remaining 36 (67%) patients were older. Thirty two (60%) tumors were located on the right side of the tonsil and 21 (40%) on the left side of the tonsil. Ten (19%) tumors were classified as T1, 28 (53%) as T2, 11 (21%) as T3, and 4 (7%) as T4. Base of the tongue invasion was present in 31 (57%) patients, and soft palate and posterior pharyngeal wall invasion were identified in 26 (49%) and 11 (21%) patients, respectively. Pterygoid muscle and nasopharynx invasion were present in 9 (17%) and 3 (6%) patients, respectively.
Ipsilateral cervical lymph node metastasis was present in 42 patients, and contralateral lymph node metastasis was identified in 9 patients. Those 9 patients with contralateral cervical lymph node metastasis also had ipsilateral lymph node metastasis. Patients without ipsilateral lymph node metastasis having contralateral lymph node metastasis were not identified in this study. Clinical features associated with ipsilateral and contralateral cervical lymph node metastases are summarized in Table 1. Contralateral cervical node metastatic status was significantly associated with a higher T stage and soft palate invasion (p=0.046 and p=0.011, respectively), while ipsilateral cervical node metastasis was not associated with any clinical features, including tobacco or alcohol consumption.
Histopathological characteristics associated with cervical nodal metastases
The average TSCC tumor size was 3.1±1.5 cm (range, 0.3 to 7.2 cm). Surgical margins for all cases did not involve squamous dysplasia, carcinoma in situ, or invasive carcinoma. The nearest distance from the surgical margin was 0.84±0.55 cm. Ten TSCC tumors (18.9%) were well differentiated, 28 (52.8%) were moderately differentiated, 15 (28.3%) were poorly differentiated, and 26 (49.1%) cases had squamous dysplasia adjacent to the main mass. Squamous dysplasia was further classified into 12 mild, 10 moderate, and 3 severe dysplasia cases. Squamous dysplasia tended to be accompanied by poorly differentiated TSCC, rather than well or moderately differentiated tumors (p=0.017) (data not shown in Table). Among the total 53 TSCC cases, 29 (54.7%) had the in situ SCC connected to the main invasive mass, whereas 25 (47.2%) had a skip lesion of the in situ SCC unconnected to the main invasive mass. The mean tumor depth of invasion was 1.53±1.08 cm.
The relationship between histopathological factors and ipsilateral or contralateral nodal metastases are summarized in Table 2. Lymphatic invasion (p<0.001) and muscle invasion (p=0.002) were significantly associated with ipsilateral cervical lymph node metastasis. Other histopathological features were not correlated with ipsilateral or contralateral lymph node metastases.
Clinical and pathological characteristics as markers of survival and prognosis
We analyzed the prognostic relevance of clinical and pathological features with respect to overall and disease-free survival of patients with TSCC (Table 3). Based on univariate analyses, patients with higher T stage, tumor invasion to the base of the tongue, and carcinoma in situ skip lesions had shorter disease-free survival periods (mean, 47 months, 54 months, and 49 months) than those without them (mean, 88 months, 100 months, and 94 months) (p=0.046, p=0.033, and p=0.039, respectively). Overall survival of patients with advanced T stage TSCC (mean, 47 months) and carcinoma in situ skip lesions (mean, 54 months) were significantly worse than those of patients without advanced T stage (mean, 91 months) or skip lesions (mean, 93 months) (p=0.012 and p=0.049, respectively) (Fig. 1).
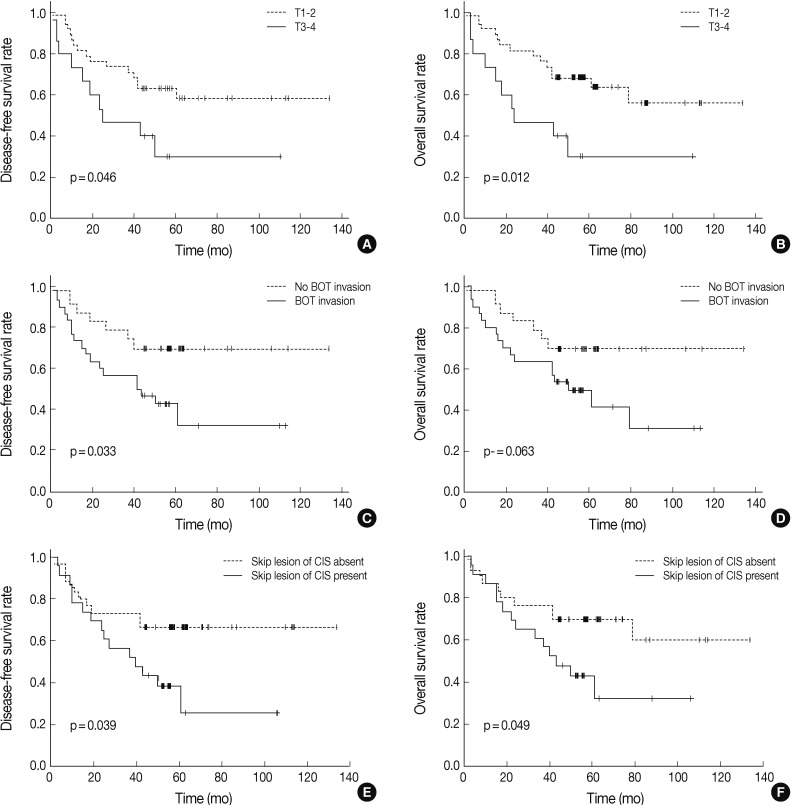
Kaplan-Meier curves for survival with respect to T stage (T1-2 vs T3-4) (A, B), invasion to base of tongue (C, D), and skip lesions of carcinoma in situ (CIS) (E, F). Patients who have tonsillar squamous cell carcinoma with higher T stage or skip lesion of CIS have lower overall survival rates, whereas those with higher T stage, invasion to the base of the tongue, or skip lesions of CIS show decreased disease-free survival. BOT, base of tongue; CIS, carcinoma in situ.
Those variables that correlated significantly with overall or disease-free survival on univariate analyses were further analyzed by multivariate analyses using a Cox regression (Table 4). Presence of skip lesions was the only independent prognostic factor predicting decreased disease-free survival (p=0.048; hazard ratio, 2.189; 95% confidence interval [CI], 1.975 to 4.914). T stage (T1,2 vs T3,4) was an independent prognostic factor associated with overall survival (p=0.019; hazard ratio, 3.060; 95% CI, 1.071 to 8.746).
DISCUSSION
Tonsil cancers can spread beneath an intact and apparently normal surface, giving rise to a larger area of tumor involvement than that suggested by gross inspection.10 They can also invade deeply into the underlying tissues, the base of tongue, and the lateral pharyngeal wall, and have a tendency to extend upwards into the nasopharynx as well.10 Furthermore, due to the abundant plexus of lymphatic vessels distributed around the palatine tonsils and the tonsillar fossa, tonsil cancers frequently give rise to nodal metastasis,6 compared to other oropharyngeal cancers.18 These aggressive characteristics have increased the urgency of finding predictive and prognostic factors that are specific to TSCC.
The optimal management of TSCC patients with clinically-node negative status in the ipsilateral or contralateral neck remains controversial. If it were possible to elucidate potential clinicopathologic predictors for lymph node metastasis, they could be used to identify patients eligible for treatment by elective neck dissection. In this study, we found that lymphatic and muscle invasion were important histopathological factors associated with ipsilateral cervical lymph node metastasis, while a higher T stage and soft palate invasion were clinical factors associated with contralateral cervical nodal metastasis. These findings are supported by a previous study by Lim et al.,6 which found advanced T3-4 stages to be associated with contralateral nodal metastasis in TSCC. The authors advocated performing elective contralateral neck treatment for TSCC patients with ipsilateral node metastases because the risk of contralateral occult neck involvement was 21%.1 Rusthoven et al.19 found that tongue base and soft palate involvement were associated with contralateral nodal metastasis in TSCC, which they suggested may be due to high levels of lymphatic drainage in the soft palate.19 Moreover, the degree of differentiation, pattern of invasive front, as well as vascular and perineural invasion have been found to correlate with nodal metastasis in SCC of the oral cavity.9,20,21 Poorly differentiated tumors have higher incidence of neck involvement than well-differentiated tumors.20 SCC patients with a cohesive, diffuse, invasive front have a higher incidence of neck metastasis and poorer prognosis than those who had non-cohesive, well-defined borders.21 However, the parameters mentioned above were not statistically correlated with neck metastasis in this study. Although involvement of the tongue base and posterior pharyngeal wall invasion did not reach statistical significance in this study, there was an increased tendency of contralateral cervical lymph node metastasis. Therefore, the microscopic confirmation of lymphatic invasion, muscle or soft palate invasion, involvement of the tongue base, and posterior pharyngeal wall invasion may help to determine the extent of neck dissection and decrease morbidity associated with unnecessary surgery or irradiation.
T stage, nodal status, histological grade, and pattern of invasion have been suggested to correlate with prognosis in oropharyngeal cancers.22,23 However, the relationship between prognosis and histopathological features in TSCC has not been fully explored. Previously, only small numbers of TSCC patients (included in a series of oral cavity and oropharyngeal cancers) have been analyzed. In this study, advanced T stage proved to be a major risk factor that adversely influenced overall survival, which is consistent with findings for other oropharyngeal cancers.22 Severe dysplasia and carcinoma in situ have been reported in about 2-17.5% in oropharyngeal cancers, with variation between studies likely resulting from different methods and attention to detail used in pathological examinations of surgical specimens. In this study, we undertook a comprehensive analysis of dysplasia adjacent to the tumor, in situ carcinoma connected to the main invasive SCC, and skip lesions of the in situ SCC unconnected with the main tumor, as they were all considered to be potential sites of local recurrence. Squamous dysplasia, SCC in situ connected to the main tumor, and skip lesions of the carcinoma in situ were present in 49.1%, 54.7%, and 47.2% of the 53 TSCC cases, respectively. The increased incidence of these lesions was revealed by intensive tumor mapping. Interestingly, the skip lesion of the carcinoma in situ proved to be an independent prognostic factor for worse overall survival. Although precursor lesions are believed to be an important indicator of malignant potential, no good data exists regarding tonsillar precursor lesions. Because precursor lesions may appear clinically normal, there is the danger that they may not be completely excised thereby increasing the risk of disease recurrence.10 This is reflected by high recurrence rates at the primary site (25-40%) in head and neck SCC,23,24 which may be due to a failure to excise skip or other precursor lesions.24
In summary, advanced T stage and soft palate invasion were associated with a high rate of contralateral nodal metastasis. Advanced T stage had clear prognostic significance in predicting overall survival among tonsil cancer patients in our study. Skip lesions of the carcinoma in situ were associated with worse disease-free survival. Therefore, when skip lesions are encountered in a surgically resected TSCC specimen, they should be commented on in the pathology report to raise clinician awareness about the potential for worse prognosis. Integrating information regarding clinicopathological factors with therapeutic principles is important to improving our overall assessment of tonsil cancer.
Acknowledgments
The authors would like to thank Moon Sook Oh for her excellent technical assistance.
Notes
No potential conflict of interest relevant to this article was reported.



