Early Colorectal Epithelial Neoplasm in Korea: A Multicenter Survey of Pathologic Diagnosis
Article information
Abstract
Background
The incidence of early colorectal epithelial neoplasm (ECEN) is increasing, and its pathologic diagnosis is important for patient care. We investigated the incidence of ECEN and the current status of its pathologic diagnosis.
Methods
We collected datasheets from 25 institutes in Korea for the incidence of colorectal adenoma with high grade dysplasia (HGD) and low grade dysplasia in years 2005, 2007, and 2009; and early colorectal carcinoma in the year 2009. We also surveyed the diagnostic terminology of ECEN currently used by the participating pathologists.
Results
The average percentage of diagnoses of adenoma HGD was 7.0%, 5.0%, and 3.4% in years 2005, 2007, and 2009, respectively. The range of incidence rates of adenoma HGD across the participating institutes has gradually narrowed over the years 2005 to 2009. The incidence rate of early colorectal carcinoma in the year 2009 was 21.2%. The participants did not share a single criterion or terminology for the diagnosis of adenoma HGD. The majority accepted the diagnostic terms that distinguished noninvasive, mucosal confined, and submucosal invasive carcinoma.
Conclusions
Further research requirements suggested are a diagnostic consensus for the histopathologic diagnosis of ECEN; and standardization of diagnostic terminology critical for determining the disease code.
Colorectal carcinoma is the third most common cancer (the second most common in males and the third in females) and one of the malignant tumors most rapidly increasing in incidence based on 2009 cancer incidence data in Korea.1,2 The National Cancer Screening Program supported by the National Health Insurance Program in Korea includes colonoscopy in adults aged 50 and older; therefore, detection and removal of precancerous lesions, such as colorectal adenoma, as well as effective detection of early colorectal cancer are increasing.3
Accordingly, pathologic diagnosis of adenoma and early carcinoma, including noninvasive, mucosal confined, and submucosal invasive carcinoma, either obtained by colonoscopic or surgical resection, is one of the growing practices in surgical pathology work areas. There is no doubt that pathologic diagnosis not only determines the principles of treatment,4 but also aids clinicians in developing the most effective management strategies, including the interval of post-polypectomy surveillance.5 Currently, pathology reports are also essential in providing collative information regarding the performance of medical procedures as well as determining the appropriate disease code for national and private health insurance registration.6
However, pathologic evaluation and diagnosis of these early colorectal neoplastic lesions, namely early colorectal epithelial neoplasm (ECEN), is not a simple practice as the terminology and diagnostic criteria are not completely established.7 The same problem existed for gastric epithelial neoplasm, and the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists (GPSG-KSP) has been making efforts for a consensus and has suggested guidelines for the differential diagnosis.8-10 To date, few definitions and guidelines have been introduced for colorectal epithelial neoplasm.11,12 A multicenter study or consensus meeting to determine the pathologic criteria for diagnosing ECEN has not been undertaken.
The most recently released World Health Organization (WHO) classification in 2010 attempted to establish definitions and guidelines for the terminology of premalignant lesions of the digestive system.7 Currently, the need for consensus and communication between pathologists and clinicians regarding the pathologic diagnosis of colorectal epithelial neoplasm has been realized.6 For these academic and practical reasons, the members of the GPSG-KSP agreed to undertake research regarding the ECEN.
In pursuit of this goal, knowledge of the current status of pathologic diagnosis and incidence of the ECEN is required, which is the aim of this multicenter survey.
MATERIALS AND METHODS
Participating institutions
Datasheets were collected from the university and general hospitals in Korea, including Inje University Seoul Paik Hospital, Seoul National University Boramae Hospital, Inje University Sanggye Paik Hospital, Seoul National University Hospital, Seoul National University Bundang Hospital, Kangbuk Samaung Hospital, Chonbuk National University Hospital, Soon Chun Hyang University Seoul Hospital, Bundang Jesaeng General Hospital, Yeungnam University Hospital, Jeju National University Hospital, Eulji General Hospital, Seoul Songdo Hospital, Soon Chun Hyang University Bucheon Hospital, Samsung Medical Center, Chosun University Hospital, Kosin University Goespel Hospital, Konkuk University Medical Center, Dankook University Hospital, Inha University Hospital, National Health Insurance Service Ilsan Hospital, Eulji University Hospital, Korea Cancer Center Hospital, Chonnam National University Hospital, and Wonju Severance Christian Hospital.
Data collection
For adenoma, information on the incidence of pathologically confirmed adenoma of the colon and rectum in the years 2005, 2007, and 2009 was collected. In Korea, colorectal cancer screening was first introduced in 2004 and has been included in the National Cancer Screening Program thereafter;13 thus, data from the included years would have little chance to produce a selection bias. In 2006 and 2008, the GPSG-KSP published two important guidelines. One of these showed the histopathologic features of the colorectal adenoma low grade dysplasia (LGD) and high grade dysplasia (HGD),11 and the other recommended the use of a strict diagnostic criteria for colorectal adenoma HGD.12 Pathologists were expected to be fully acquainted with and influenced by each guideline when making the diagnosis of colorectal neoplasm in the following year, and this would be reflected in the 2007 and 2009 data.
The data from each year were independently collected based on the numerical value of individual patients (not the number of adenomas). Even if a patient had more than one adenoma in the same data-collecting year, he or she was counted as one. Each case was assigned to have adenoma with LGD or HGD according to the highest grade adenoma present. If the adenoma had been reported as having focal HGD or LGD to HGD, it was assigned to either LGD or HGD according to the participating pathologist's diagnostic perspective. Each datasheet was constructed on the basis of the electronic operating system of the institution, such as an electronic medical record. There was no need to microscopically review the pathologic material. The exclusion criteria were as follows: 1) cases with concurrent colorectal adenocarcinoma diagnosed in the same data-collecting year; 2) cases only having serrated adenoma; and 3) cases with adenoma but inadequate grading, regardless of the cause of the inadequacy. For adenoma with LGD that had simply been reported as adenoma without further designation (only the adenoma with HGD had been graded by virtue of the institutional pathologist's diagnostic policy), the adenoma was not excluded and was grouped as LGD. The flow chart for completing datasheet for the incidence of colorectal adenoma is depicted in Fig. 1.

Flow chart for completing the datasheet regarding the incidence of colorectal adenoma. LGD, low grade dysplasia; HGD, high grade dysplasia.
For colorectal carcinoma, we collected incidence data for both colonoscopically or surgically resected and newly diagnosed early colorectal carcinoma, including mucosal confined and submucosal invasive carcinoma, as well as the total number of colorectal carcinoma in the year 2009. Cases with recurrent or metastatic carcinoma were excluded.
We also surveyed and investigated the diagnostic form and terminology of ECEN currently used by 25 participating pathologists. The answers to the questionnaires were collected from June 2012 to November 2012.
Ethical considerations
We collected only the final datasheets from the participating hospitals and did not collect any individual patient's data, including name, age, sex, resident or hospital registration number, pathologic diagnosis, or survival.
RESULTS
Colorectal adenoma
The summary of the incidence of colorectal adenoma is presented in Table 1. The annual incidence of the pathologic diagnosis of colorectal adenoma has been continuously increasing, with 1.40 times in 2007 and 1.93 times in 2009 compared to the level in 2005 while the whole number of surgical pathology practice cases has increased 1.12- and 1.36-fold in the corresponding years, respectively (Fig. 2). The proportion of pathologic diagnosis of colorectal adenoma out of all surgical pathology cases has been also increased by 5.56% in 2005, 6.93% in 2007, and 7.90% in 2009.
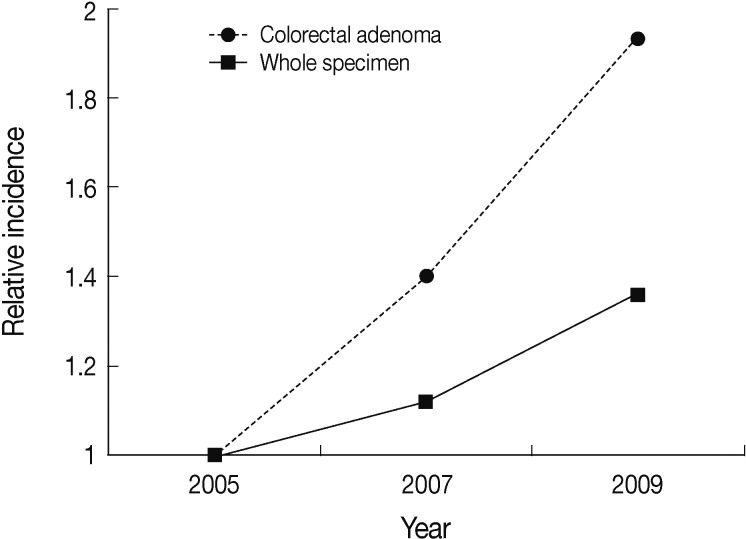
The relative incidence of the number of pathologic diagnoses of colorectal adenoma and whole surgical pathology specimen in the years 2007 and 2009 compared to 2005.
The average percentage of adenoma HGD was 6.94%, 5.02% and 3.38% in the years 2005, 2007, and 2009, respectively. The range of incidence rates of adenoma HGD across the participating institutes was 1.0% to 38.4% in 2005, 1.1% to 15.2% in 2007, and 0.6% to 11.8% in 2009. The distribution of the participating institutes corresponds to each grouped range of incidence rates of adenoma HGD is depicted in Fig. 3. The number of institutes with a less than 5% incidence rate of adenoma HGD increased from 10 to 15, while the number of institutes with a greater than 10% incidence rate of adenoma HGD decreased from 7 to 2 over the years 2005 to 2009.
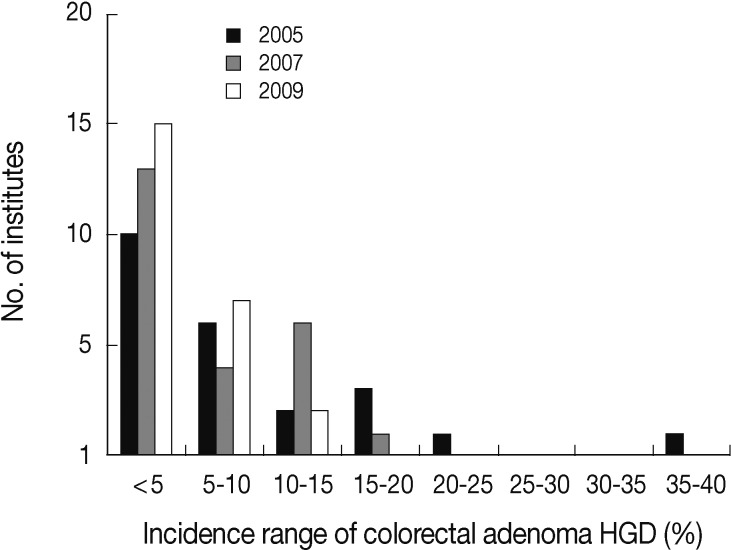
The distribution of the participating institutes corresponding to each grouped range of incidence rates of adenoma with high grade dysplasia (HGD) in the years 2005, 2007, and 2009.
Twenty-one institutes used the term focal HGD or low to HGD with an incidence rate of 0.9%, 1.7%, and 1.7% in the years 2005, 2007, and 2009, respectively.
Early colorectal carcinoma
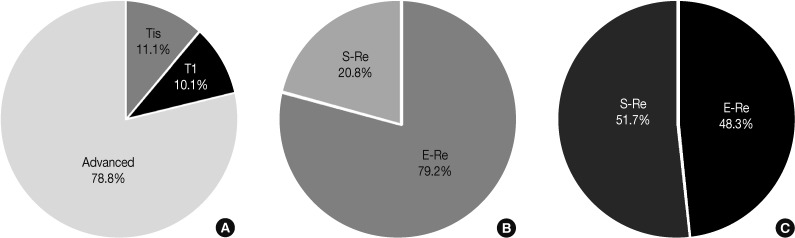
We collected 1,332 early carcinomas out of 6,277 colorectal carcinoma patients, and the incidence rate of early colorectal carcinoma in the year 2009 was 21.2%. There were 697 (11.1%) cases of mucosal confined carcinoma (Tis) and 635 (10.1%) cases of submucosal invasive carcinoma (T1) (Fig. 4). These were initially treated by colonoscopic resection (64.5%) or surgical resection (35.5%). For Tis carcinoma, the colonoscopic resection rate (79.2%) was much higher than the surgical resection rate (20.8%), while the surgical resection rate for T1 carcinoma (51.7%) was slightly higher than the colonoscopic resection rate (48.3%).
Diagnostic form and terminology for early colorectal epithelial neoplasm
The results of the responses from the participating pathologists to the questionnaire survey are summarized in Table 2.
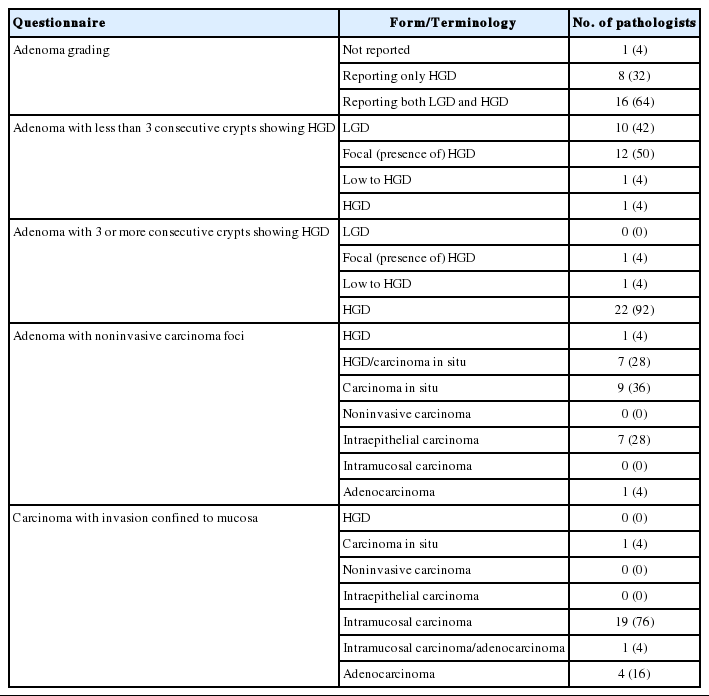
Responses of the participating pathologists to the questionnaire survey regarding the currently using diagnostic forms and terminology for early colorectal epithelial neoplasia
The majority of the participating pathologists (96%) apply a two-tiered grading when making the diagnosis of colorectal adenoma. More than half of the pathologists (64%) complete the diagnosis of colorectal adenoma stringently appending the grade, either LGD or HGD. On the other hand, a number of pathologists (32%) selectively add the grade in the case of adenoma HGD. They use the term adenoma when the lesion demonstrates the features of LGD, instead of further mentioning the grade.
When reporting adenoma with less than 3 consecutive crypts demonstrating features of HGD, half of the pathologists (50%) still use the term "focal" (presence of) HGD, while 42% of the pathologists simply report it as adenoma LGD. For adenoma with 3 or more consecutive crypts demonstrating features of HGD, the majority of the pathologists (92%) agree on using the term HGD. Twenty-one out of the 25 participating institutes have used the term focal HGD or low to HGD; 7 pathologists assigned these to adenoma LGD, whereas the other 13 assigned them to adenoma HGD. The remaining pathologist classified these on a case by case basis (data obtained from the flow chart shown in Fig. 1).
In the cases of the adenoma with noninvasive carcinoma foci, 28% use the term HGD/carcinoma in situ, 36% carcinoma in situ, and a further 28% intraepithelial carcinoma. More than two-thirds of the pathologists (76%) choose the term intramucosal carcinoma when making a diagnosis of the carcinoma with invasion confined to the mucosa, and 16% simply use the term adenocarcinoma.
DISCUSSION
In this survey, we collected the recent pathologic data on the incidence of ECEN with respect to the grade of adenoma and early carcinoma and the responses to questionnaires regarding the currently used diagnostic forms and terms.
There have been remarkable increases in the number and proportion of biopsied or resected colorectal adenoma in surgical pathology practice, reaffirming the importance of this survey. The reason for this increase may be the effective colonoscopic examination supported by the National Cancer Screening Program and the awareness of the importance of health in the general population, as well as an actual increase in colorectal adenoma.
The overall incidence rate of adenoma HGD gradually declined during the survey years. This change may be a positive sign, as it is generally thought that the incidence of adenoma HGD is less than 5% of all colorectal adenoma.14 The range of incidence rates has been narrowing, and the number of institutes with a less than 5% incidence rate of adenoma HGD has increased from 40% to 60%, another favorable trend. The rather low incidence rate of 3.38% adenoma HGD in 2009 may not reflect an actual deficit because the rate of 5% adenoma HGD in western countries includes mucosal confined carcinoma.15,16 The total actual incidence rate of adenoma HGD and mucosal confined carcinoma in 2009 reached 4.90%. These findings suggest that the guidelines proposed by the GPSG-KSP11,12 have been effective in reducing discrepancies in the grading of colorectal adenoma. The correct incidence rate of adenoma HGD is also important because the WHO classification in 2010 introduced new biologic behavior codes, LGD as /0 and HGD as /2. Accordingly, adenoma HGD has different disease code for the national and private health insurance registration, unlike the previous disease code /0 assigned to adenoma as a whole. Still, there are considerable inter-institutional differences in the incidence of adenoma HGD, likely caused by heterogeneous criteria and thresholds of a grading system that remain to be defined. A recent study by GPSG-KSP achieved an encouraging high inter-observer agreement rate for biopsy and endoscopic resection specimens of gastric epithelial neoplasia by extensive review and discussion in serial consensus conferences.10 We could expect a similar result if we make additional efforts to promote diagnostic consensus for the histolopathologic grading of colorectal adenoma.
In the current study, the proportion of early colorectal carcinoma in the year 2009 was 21.2%. The early colorectal carcinoma in the present study is defined by the Japanese rule and includes both mucosal confined and submucosal invasive carcinoma.17 There were 11.1% mucosal confined carcinoma and 10.1% submucosal invasive carcinoma. To our knowledge, this is the first report investigating the overall incidence of early colorectal carcinoma in Korea based on multicenter data collection. More than half of the early colorectal carcinoma cases were initially treated by colonoscopic resection. Even in submucosal invasive carcinoma, the colonoscopic resection rate was quite high and not much different from the surgical resection rate. Our data does not show the number of patients further treated by surgical resection after colonoscopic resection; therefore, the actual rate of each therapeutic method is likely to be corrected. Nevertheless, pathologists are more frequently encountering early colorectal carcinoma resected by colonoscopic procedures. Since the criteria that should be included in the pathologic diagnosis report for colonoscopically resected early colorectal carcinoma are very complicated and usually require histopathologic mapping, and pathologists have to invest enormous amounts of time and effort.4,11 Moreover, early colorectal carcinoma can be detected in small polyps simply resected by colonoscopic polypectomy with no prior clinical suspicion of a frank carcinoma.18 It is preferable to make an upward adjustment of the reimbursement value for the pathologic diagnosis of colorectal neoplastic lesions resected by colonoscopic procedures such as polypectomy or mucosal/submucosal resection.19
In 2011, the GPSG-KSP held a workshop to update the guidelines for cancer registration of gastrointestinal tumors.20 In this workshop, an attempt was made to standardize the representative diagnostic terms. The purpose of the trial was to provide unified information to clinicians, especially when they report a disease code that determines the medical insurance reimbursement as well as enrollment in the national cancer registry data in Korea. This may be a sensitive issue as it would induce certain restrictions on the autonomy of the pathologists' own specialty, while the terminology for the pathologic diagnosis of ECEN is still not completely established.7 Therefore, a minimal recommendation was made to reduce confusion caused by neutral diagnostic terms. In this study we surveyed the diagnostic form and terminology of ECEN currently used by individual participating pathologists. The criterion for the 'presence of 3 or more consecutive crypts showing HGD' when making the diagnosis of adenoma HGD was a previously proposed provision,11,21 and it was agreed on by the majority of the participating pathologists. For adenoma with less than 3 consecutive crypts showing HGD, however, focal (presence of) HGD was preferred for the representative diagnosis, and more than half of the participants actually considered these as adenoma HGD. The participants shared a different perspective on that point, and this criterion is supposed to be a sufficient condition but not a requirement for the diagnosis of adenoma HGD.
In the case of adenoma with noninvasive carcinoma foci, the majority of the participants did not write out the term adenocarcinoma as the ultimate pathologic diagnosis. Most of them favored terms state carcinoma in situ, whereas intraepithelial carcinoma was less frequently used. Similarly, 80% of the participants selected intramucosal carcinoma (including one participant who chose intramucosal carcinoma/adenocarcinoma) instead of simply using the term adenocarcinoma in the case of the mucosal confined carcinoma. This result may reflect the fact that a number of pathologists now accept that noninvasive and mucosal confined colorectal carcinoma should be distinguished from submucosal invasive carcinoma as well as from each other in diagnostic terminology. The GPSG-KSP has recommended the term HGD or intraepithelial carcinoma for adenoma with noninvasive carcinoma foci and intramucosal carcinoma for mucosal confined carcinoma.20 This recommendation was made in accordance with the 2010 WHO classification,16 however, further discussion regarding terminology for the representative pathologic diagnosis that encompasses not only the opinion of pathologists but also feedback from clinicians is needed.
In the present study, we provide recent data regarding the incidence and current status of diagnostic forms and terminology of ECEN provided by the participant pathologists from 25 institutions. The issues and future research requirements raised by this study are: 1) the development and updating of diagnostic consensus for the histopathologic diagnosis of ECEN; and 2) the minimum standardization of the diagnostic terminology critical for determining the disease code. The upcoming research should include a national research project for the benefit of the public that has to be supported by a sustainable budget. We also cordially ask for a profound commitment from the members of the GPSG-KSP and KSP.
Notes
No potential conflict of interest relevant to this article was reported.