A Giant Peritoneal Loose Body
Article information
Abstract
Peritoneal loose bodies (PLBs) are usually discovered incidentally during laparotomy or autopsy. A few cases of giant PLBs presenting with various symptoms have been reported in the literature. Here, we describe a case of a giant PLB incidentally found in the pelvic cavity of a 50-year-old man. Computed tomography revealed a free ovoid mass in the pelvic cavity that consisted of central dense, heterogeneous calcifications and peripheral soft tissue. The mass was an egg-shaped, hard, glistening concretion measuring 7.5×7.0×6.8 cm and weighing 160 g. This concretion consisted of central necrotic fatty tissue surrounded by concentrically laminated, acellular, fibrous material. Small PLBs usually do not require any specific treatment. However, if PLBs cause alimentary or urinary symptoms due to their large size, surgical removal may be recommended. It is essential for clinicians to be aware of this entity and its characteristic features to establish the correct diagnosis.
Peritoneal loose bodies (PLBs) are usually discovered during laparotomy or autopsy. It is generally agreed that these bodies are derived from the epiploic appendices via sequential processes of torsion, infarction, saponification, and calcification.1 In most cases, PLBs are asymptomatic and are no larger than a pea; they have little or no clinical significance and do not require any specific treatment.2 However, they occasionally grow to larger dimensions and cause symptoms such as intestinal obstruction and urinary retention.3-5 Here, we describe a case of a giant PLB incidentally found in the pelvic cavity of a 50-year-old man and its associated problems, and discuss how such a large body could develop.
CASE REPORT
A 50-year-old man underwent a routine medical examination, at which time multiple gallstones and an incidental pelvic mass were detected on computed tomography (CT) scanning of the abdomen and pelvis. An ovoid, well-defined mass in the pelvic cavity was detected consisting of central dense, heterogeneous calcifications and peripheral soft tissue (Fig. 1A). The mass compressed the bladder wall (Fig. 1B). There was a distinct fat plane around the mass, which did not appear to originate from or invade any of the adjacent organs. The patient denied any symptoms and the presence of any past medical problems. Laboratory tests were all within the normal range. Based on the radiologic findings, a preoperative diagnosis of peritoneal calcifying fibrous pseudotumor was suggested. On laparoscopic exploration, a well-circumscribed, fist-sized, hard, and free mass was found in the pelvic cavity. In addition, some of the epiploic appendices attached to the sigmoid colon were calcified with constricted stalks and were on the verge of becoming detached. All other abdominal and pelvic viscera were unremarkable. Laparoscopic cholecystectomy and pelvic mass removal were performed.
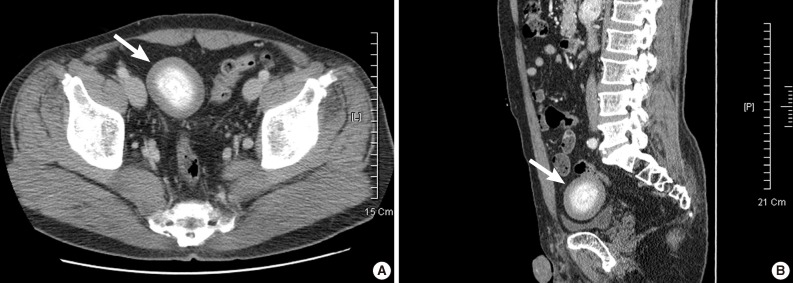
Abdominopelvic computed tomography findings. (A) Axial image shows a large, oval-shaped mass (arrow) consisting of peripheral soft tissue and central dense, heterogeneous calcifications. There is a distinct fat plane separating the mass from the adjacent organs. (B) Sagittal image reveals that the mass (arrow) compresses the bladder wall.
Grossly, the pelvic mass measured 7.5×7.0×6.8 cm and weighed 160 g; it was a white-to-pale yellow, hard, glistening concretion that looked like a boiled egg with the shell removed (Fig. 2A). The cut surface of the concretion revealed a central 1.5 cm-diameter nucleus of a creamy, cheese-like material surrounded by white-to-yellow lamellar structures (Fig. 2B). Microscopically, the concretion consisted of central necrotic fatty tissue (Fig. 2C) surrounded by many layers of concentrically laminated, eosinophilic, acellular, fibrous material (Fig. 2D) with scattered blue-to-black lakes of microcalcifications (Fig. 2E). Masson's trichrome stained the fibrous material blue, indicating an abundance of collagen (Fig. 2F). There were variable-sized vacuoles and empty clefts interspersed among the laminated material that could have represented vestiges of aged fat necrosis. The surface was partially lined by mesothelial cells. No inflammatory or foreign body reactions, parasites, polarizable substances, or identifiable tumor tissues were present in the specimen. These histopathological findings were characteristic of a giant PLB. The patient had an uneventful recovery. He was discharged from the hospital five days after surgery.
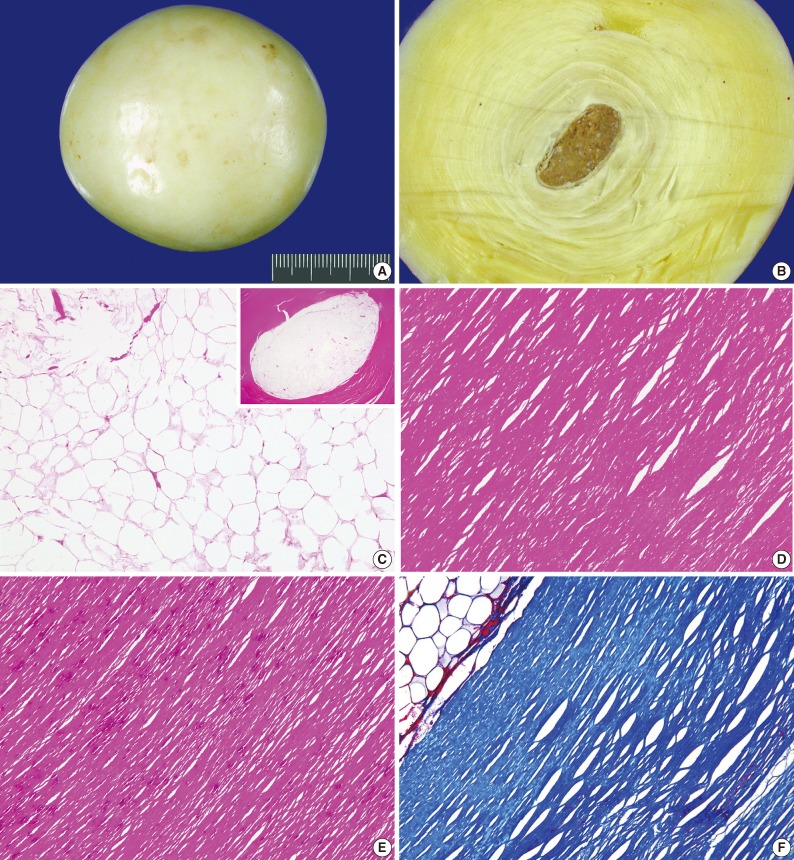
Gross and histologic findings. (A) Grossly, the mass is an egg-shaped, white-to-pale yellow, hard, glistening concretion, measuring 7.5×7.0×6.8 cm, weighing 160 g, and resembling a boiled egg. (B) The cut surface of the concretion reveals a 1.5 cm diameter central portion of gray-to-yellow, creamy material surrounded by concentrically lamellar structures. (C) Microscopically, the central portion (inset) of the concretion consists of necrotic fatty tissue. (D) The peripheral portion consists of many layers of laminated, acellular, fibrous material. (E) Scattered blue-to-black lakes of microcalcifications are also identified in the peripheral portion. (F) Masson's trichrome staining shows intensely staining collagen at the periphery.
DISCUSSION
Although many possible etiologic factors have been proposed to explain the appearance of PLBs, it is widely believed that the most common cause of PLB is the chronic torsion of the epiploic appendix.1,6 The appendix may be attached by a thin pedicle that undergoes torsion, leading to infarction or aseptic fat necrosis. Thereafter, saponification and calcification of the fatty contents occur and the pedicle then atrophies. The epiploic appendix finally detaches from the colon and becomes a PLB. Over the years, the PLB becomes enlarged due to peritoneal reactions to this freely moving epiploic appendix as well as the depositions of peritoneal serum upon it. The center of the PLB thus contains necrotic fatty tissue with outer concentric zones of microcalcification surrounded by densely laminated, hyalinized, acellular fibrous tissue. In support of this hypothesis, previous reports have demonstrated that the size of PLB gradually increases. Donald and Kerr7 generated "peritoneal mice" in the laboratory by taking periuterine fat from guinea pigs. The "peritoneal mice" were placed in the peritoneal cavity of the same animals and typical PLBs were generated. The fibrous capsule of the PLBs was thicker in animals killed after 6 months than in animals killed after 12 days, indicating the slow growth of calcified layers around the necrotic center. In addition, Mohri et al.8 reported that the size of the PLB increased from 7.3×7.0 cm to 9.5×7.5 cm in a patient in a span of 5 years.
The clinical features of previously published cases are summarized in Table 1. The patients with PLB ranged in age from 2 months to 79 years at the time of diagnosis. Although there was no predilection for the location, the PLBs were mostly found to be free-floating in the pelvic cavity and tended to gravitate to the most dependent part of the abdominal cavity. The clinical presentation of the PLBs included small bowel obstruction, urinary tract infection, acute urinary retention, intermittent constipation, pelvic pain, and abdominal discomfort. Although the majority of PLBs range from 0.5 to 2.5 cm in diameter and generally cause no symptoms,7 they can reach a diameter of 5 to 9.5 cm and are then termed "giant" PLBs. Because of the limited room in the pelvic bowl, giant PLBs can compress pelvic structures, resulting in intestinal obstruction, incomplete bowel emptying, and urinary retention.3-5,9 The most common radiological finding of a PLB is an oval-shaped mass with a central calcification and a low-intensity area. On plain abdominal films, the appearance of a PLB has been described as a round or oval calcified mass with a mobile nature.6 CT scanning often reveals a concentric, round or oval well-defined mass with a central calcificationand surrounded by peripheral soft tissue.10 The correct diagnosis was preoperatively suggested in only one case,8 possibly due to the rarity of this entity. All but one patient underwent laparoscopic or open surgery for mass removal, and none of the patients developed a recurrence of the the PLB during the follow-up period.
Obviously, it is important to distinguish PLBs from other mobile lesions of the pelvic cavity such as calcified uterine leiomyomas, peritoneal calcifying fibrous pseudotumors, foreign body granulomas, desmoid tumors, teratomas, metastatic lesions of ovarian cancer, spontaneously amputated ovaries, fecaliths, lymphatic glands in the mesentery, nodal calcifications, tuberculosis, ecchinococcal cysts, urinary stones, and gallstones. Calcified uterine leiomyomas and peritoneal calcifying fibrous pseudotumors are especially hard to differentiate from PLBs because they also appear as round or oval masses in the pelvic cavity with soft tissue density and irregular calcifications. Furthermore, on magnetic resonance imaging, a PLB appears as a low-intensity mass on both T1- and T2-weighted images, and has the same intensity as muscle tissue or collagen fiber.11,12 However, unlike PLBs, both leiomyomas and calcifying fibrous pseudotumors are enhanced with contrast, which can discriminate these lesions from PLBs. In addition, since PLBs are freely mobile, additional scanning with the patient in the prone position or a follow-up imaging study can demonstrate a change of mass location, facilitating the diagnosis with higher confidence. Surgical removal with histological examination can definitively confirm the diagnosis based on the characteristic morphological features of PLBs.
To date, a few cases of giant PLBs have been reported in the literature.2-5,8,9,11-13 Even though these patients were asymptomatic, surgery was performed to remove the suspected neoplasm. Considering the nature of the lesion, no specific treatment is required in asymptomatic patients. However, if there is a pelvic mass of obscure origin, or if it becomes associated with alimentary or urinary symptoms due to its large size, surgical exploration and removal may be recommended. It may be better to treat these patients laparoscopically.
In summary, we describe a case of a giant PLB found incidentally and discuss its diagnostic features. Even though giant PLBs are extremely rare, they should be considered in the differential diagnosis of a mobile lesion in the pelvis and abdomen. If they cause alimentary or urinary symptoms due to their large sizes, surgical removal may be recommended. It is important for radiologists and clinicians to be aware of this rare entity and its characteristic features to establish the correct diagnosis.
Acknowledgments
The views and opinions expressed in this article are those of the authors and do not reflect the official policy or position of the Republic of Korea Air Force or Republic of Korea Ministry of National Defense.
Notes
No potential conflict of interest relevant to this article was reported.
