Micropapillary Mucinous Adenocarcinoma of the Lung: A Brief Case Report
Article information
In 2011, the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) classification added micropapillary predominant adenocarcinoma of the lung as a new histologic subtype and reclassified the former mucinous bronchioloalveolar carcinoma (BAC) as a variant of invasive mucinous adenocarcinoma.1
Recent studies regarding epidermal growth factor receptor (EGFR) and K-ras mutations in lung cancer demonstrated that BAC with a lepidic or hobnail growth pattern is more typically associated with EGFR mutation, while mucinous differentiation is more common in cases with K-ras mutation.2 - 4 However, these studies were based on the 2004 World Health Organization (WHO) classification, and there had been a few reports on the micropapillary pattern of this disease and its correlation with EGFR and K-ras mutations.4,5 According to the report of the IASLC,1 micropapillary predominant adenocarcinoma is known to be related to K-ras (33%), EGFR (20%), and BRAF (20%) mutations. Hypothesizing that micropapillary predominant adenocarcinoma with mucinous differentiation may be correlated with K-ras mutation, we performed a histological review of a case of micropapillary mucinous adenocarcinoma with associated K-ras mutation.
CASE REPORT
A 69-year-old woman presented with persistent cough for one month previously. The patient had a 13 pack-year smoking history and hypertension. Chest computed tomography revealed predominant ground glass opacity with patchy consolidation occupying almost the entire left lower lobe of the lung (Fig. 1A). It was histologically confirmed as adenocarcinoma of the lung by transbronchial lung and lymph node biopsy. Analysis of EGFR and K-ras mutation by polymerase chain reaction-sequencing was performed on tissue from the lymph node biopsy, which revealed missense mutation of K-ras in the 12th codon, c.34G>T (p.G12C), without EGFR mutation. After neoadjuvant concurrent chemoradiation, a left lower lobectomy was performed. The gross examination revealed a poorly defined, large, mass-like lesion with scattered dilated bronchus, which was similar in appearance to lobar pneumonia and well correlated with radiologic findings (Fig. 1B).
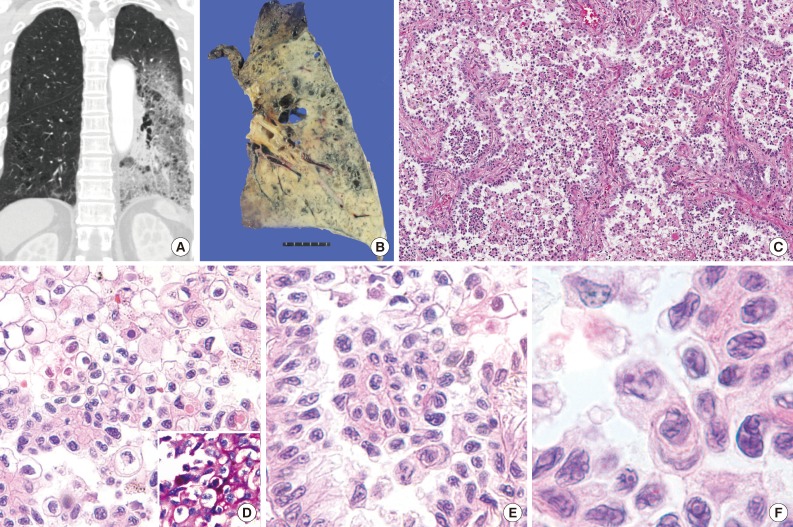
Clinicohistological features of micropapillary mucinous adenocarcinoma. (A) On chest computed tomography, almost the entire left lower lobe of the lung has diffuse ground glass opacity with patchy consolidation, which is often present in invasive mucinous adenocarcinomas. (B) The tumor occupies almost the entire left lower lobe with a diffusely consolidated appearance, similar to lobar pneumonia. (C) At the low power view, the tumor consists of predominant micropapillary tufts floating within air spaces lined by tumor cells. (D) Tumor cells of the micropapillary tufts have abundant clear or amphophilic cytoplasm with a distinct cell border, with irregular hyperchromatic nuclei. The cytoplasm of a few tumor cells shows positivity on periodic acid Schiff stain (inset). (E) The lining cells of septa are same with those of micropapillary tuft and show hobnail appearance. (F) The nuclei of the tumor cells are large and hyperchromatic, with a distinct crumpled nuclear membrane and frequent macronucleoli.
Microscopically, the tumor demonstrated a predominantly micropapillary growth pattern in the alveolar cavity and a lepidic growth pattern along the septa with hobnail features (Fig. 1C). Neoplastic cells with abundant clear or amphophilic cytoplasm intermingled with each other (Fig. 1D). Special stains (periodic acid Schiff, mucicarmine, and Alcian blue pH 1.0 and 2.5) revealed positivity in the cytoplasm of a few tumor cells (Fig. 1D, inset). Tumor cells had well-defined cell borders and large, pleomorphic nuclei (Fig. 1E), with occasional horse-shoe shaped nuclei and perinuclear clearing. Their nuclei had a contorted prominent membrane, similar to the raisinoid appearance induced by human papillomavirus infection, and had frequent prominent macronucleoli (Fig. 1F).
No complications were noted in the two-month follow-up period after discharge.
DISCUSSION
Due to the scarcity of publications regarding the micropapillary subtype of lung adenocarcinoma and the problem of the undefined threshold for classification of micropapillary adenocarcinoma, the incidence rate of this disease is not well known, but is estimated to represent approximately 6% of all lung adenocarcinomas (6.8% in Warth et al.6 and 6.0% in Solis et al.7) with no available data in the Korean population. Recent reports have described it as having a poor prognosis similar to solid-type lung adenocarcinomas.7
Considering the usefulness of EGFR-tyrosine kinase inhibitors, the importance of confirming the existence of EGFR or K-ras mutations cannot be emphasized enough. EGFR and K-ras mutations are virtually mutually-exclusive and directly related to targets of different subsets of lung adenocarcinomas.8 Therefore, it is important to decide, using relevant findings, which test is the priority for the limited specimens obtained from percutaneous needle biopsy or bronchoscopic biopsy. For example, if histologic findings are more indicative of K-ras mutation, we can potentially prevent an unnecessary test for EGFR mutation.
De Oliveira Duarte Achcar et al.5 analyzed the molecular profile of 15 primary micropapillary adenocarcinomas for K-ras, EGFR, and BRAF mutations after dividing them into three groups by histologic features: nonmucinous hobnail configuration or terminal reserve unit-type micropapillary adenocarcinoma, tumors with predominant columnar or polygonal cell configuration, and tumors of mixed type. In their study, tumors with nonmucinous hobnail pattern and those with columnar or polygonal pattern showed no significant differences in EGFR, K-ras, and BRAF mutation tests, and both K-ras and EGFR mutations could occur in mucin-producing tumors. Therefore, they concluded that there was no clear association between these mutations and morphologic features.
However, Inamura et al.4 reported a significant association between the hobnail cell type and EGFR mutation, in the setting of lung adenocarcinomas categorized into hobnail, columnar, and polygonal cell type. Ninomiya et al.9 also reported that the hobnail cell type and micropapillary morphology predicted a higher incidence of EGFR mutation in lung adenocarcinomas and speculated that distinct micropapillary features reflect a step of tumor progression from a well-differentiated papillary adenocarcinoma of the hobnail cell type to a less differentiated state.
When cytological features, rather than growth pattern, are a priority for consideration, micropapillary adenocarcinoma with mucinous features should be regarded as mucinous adenocarcinoma. This might also correspond with the results of other studies that suggest K-ras mutation is related to mucinous BAC of the lung.2
Considering our case, which demonstrated a hobnail or lepidic growth pattern with mucinous differentiation in combination with K-ras mutation, further study is needed to clarify the relationship between the presence of mucinous features of micropapillary predominant adenocarcinoma and K-ras mutation.
Notes
No potential conflict of interest relevant to this article was reported.