Characteristics of Cutaneous Lymphomas in Korea According to the New WHO-EORTC Classification: Report of a Nationwide Study
Article information
Abstract
Background
Previously, cutaneous lymphomas were classified according to either the European Organization for the Research and Treatment of Cancer (EORTC) or the World Health Organization (WHO) classification paradigms. The aim of this study was to determine the relative frequency of Korean cutaneous lymphoma according to the new WHO-EORTC classification system.
Methods
A total of 517 patients were recruited during a recent 5 year-period (2006-2010) from 21 institutes and classified according to the WHO-EORTC criteria.
Results
The patients included 298 males and 219 females, and the mean age at diagnosis was 49 years. The lesions preferentially affected the trunk area (40.2%). The most frequent subtypes in order of decreasing prevalence were mycosis fungoides (22.2%), peripheral T-cell lymphoma (17.2%), CD30+ T-cell lymphoproliferative disorder (13.7%), and extranodal natural killer/T (NK/T) cell lymphoma, nasal type (12.0%). Diffuse large B-cell lymphoma accounted for 11.2% of cases, half of which were secondary cutaneous involvement; other types of B-cell lymphoma accounted for less than 1% of cases.
Conclusions
In comparison with data from Western countries, this study revealed relatively lower rates of mycosis fungoides and B-cell lymphoma in Korean patients, as well as higher rates of subcutaneous panniculitis-like T-cell lymphoma and NK/T cell lymphoma.
Cutaneous lymphoma represents 4% of the total number of malignant lymphoma cases in Korea.1 Lymphoma may involve the skin as the primary and only site of involvement or as a secondary site of disease. Some lymphomas are present only in the skin, where they resemble their nodal counterparts histologically but nevertheless represent distinct entities.2 Currently, cutaneous lymphomas are classified according to either the European Organization for the Research and Treatment of Cancer (EORTC) or the World Health Organization (WHO) classification systems. Following a consensus meetings of the two organizations, a joint WHO-EORTC classification was developed.2,3 Compared with 2001 WHO classification system, primary cutaneous aggressive epidermotropic CD8-positive cytotoxic T-cell lymphoma, primary cutaneous γδ T-cell lymphoma, and primary cutaneous small/medium CD4-positive T-cell lymphoma are included as provisional entities, and variants of diffuse large B-cell lymphoma (DLBCL) are also described. In addition, the 4th edition of the WHO classification system includes blastic plasmacytoid dendritic cell (BPDC) neoplasms previously categorized as blastic natural killer (NK)-cell lymphoma.2,4
To date, several large scale studies on cutaneous lymphoma have been performed in Western countries.3,5,6 However, literature on Korean cutaneous lymphomas is limited because of the rarity of cases and thus the inability to study large numbers of patients. In the present study, we analyzed the incidence of cutaneous lymphoma in Korean patients according to the new WHO-EORTC classification system.
MATERIALS AND METHODS
A total of 517 cases of cutaneous lymphoma diagnosed at 21 institutes in Korea between January 2006 and December 2010 were enrolled in our study. The cases were reviewed by hematopathologists and re-classified according to the new WHO-EORTC classification.2,3,4 Clinical data including age, sex, site of involvement, and primary or secondary disease were obtained. The histologic and clinical results were compared with those of previous Western studies.
RESULTS
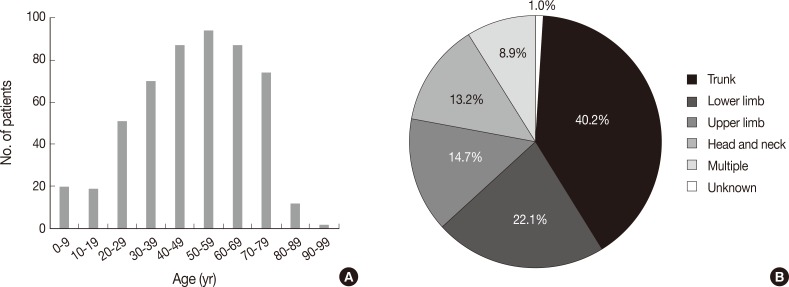
Patients were aged between 1 and 91 years (mean, 49 years). Although any age group may be involved, cutaneous lymphoma was most common in patients in their fifth, sixth, and seventh decades, with a peak incidence at approximately 60 years of age (Fig. 1A). Patients included 298 males (57.6%) and 219 females (42.4%) (male:female ratio, 1.4:1). Lesions could be present at any site, but the trunk was the most common anatomic site (40.2%) (Fig. 1B).
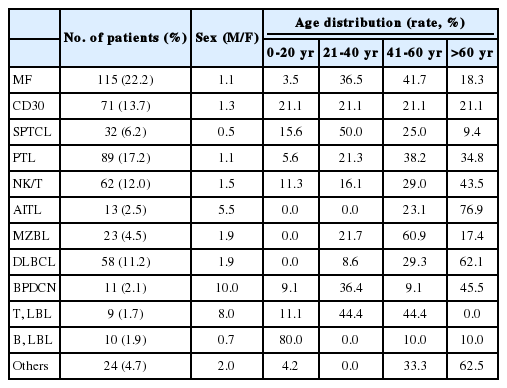
The overall incidence of cutaneous lymphoma according to the WHO-EORTC classification is summarized in Table 1. Among a total of 517 cases of cutaneous lymphoma, primary and secondary cutaneous lymphomas accounted for 73.1% and 26.1%, respectively, while only 0.8% of cases were undetermined. Among all 517 patients, the relative frequencies of mature T-cell lymphoma, mature B-cell lymphoma, immature hematopoeitic malignancy and Hodgkin's lymphoma were 74.3%, 18.0%, 5.8%, and 0.2%, respectively. Further, for the 378 cases of primary cutaneous lymphomas, the proportion of T-cell lymphoma (82.3%) increased when compared with the proportion of total cases.
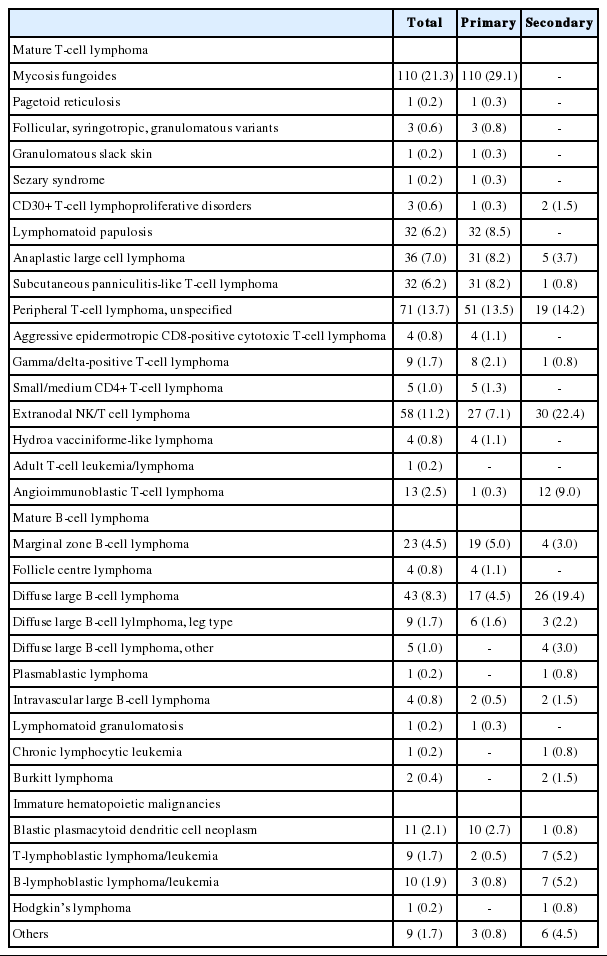
Incidence of cutaneous lymphoma according to WHO-EORTC classification in Korea between 2006 and 2010
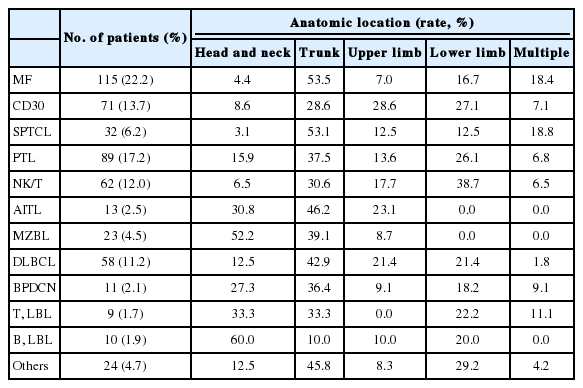
The most frequent subtypes, in decreasing order of prevalence, were mycosis fungoides (MF) including its variants (22.2%), peripheral T-cell lymphoma (PTCL) including subtype (17.2%), CD30+ T-cell lymphoproliferative disorder (CD30+ LPD) (13.7%), and extranodal NK/T cell lymphoma, nasal type (12.0%), respectively (Fig. 2A). MF variants including pagetoid reticulosis or folliculotropic were rarely described. Of the CD30+ LPD, there were 32 (6.2%) cases of lymphomatoid papulosis (LyP) and 36 (7.0%) cases of anaplastic large cell lymphoma (ALCL). Three cases could not be subclassified, and ALCL included five systemic cases. Half of the NK/T cell lymphoma cases were secondary lymphoma. Other cutaneous T-cell lymphoma included subcutaneous panniculitis-like T-cell lymphoma (SPTCL) (6.2%), angioimmunoblastic T-cell lymphoma (AITL) (2.5%), and T lymphoblastic lymphoma (1.7%). Adult T-cell leukemia/lymphoma was rarely observed (0.2%). With respect to primary cutaneous lymphoma, the proportion of MF, CD30+ LPD and SPTCL was increased (Fig. 2B). Among B-cell lymphomas, the DLBCL was the most common lymphoma and accounted for 11.2% of cases, although half were secondary cutaneous involvement. Cutaneous marginal zone B-cell lymphoma was the second most common B-cell lymphoma (4.5%), and other types of B-cell lymphoma accounted for less than 1% of cases. Immature hematopoietic malignancies included BPDC neoplasm (11 cases, 2.1%), T-lymphoblastic leukemia/lymphoma (9 cases, 1.7%) and B-lymphoblastic leukemia/lymphoma (10 cases, 1.9%).
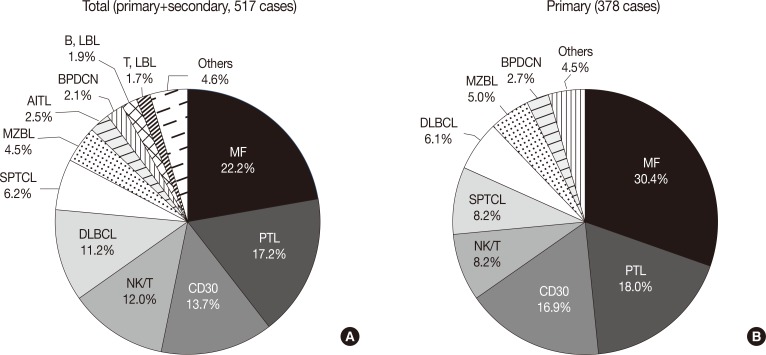
(A, B) Relative frequency of cutaneous lymphoma according to subtype. MF, mycosis fungoides; PTL, peripheral T-cell lymphoma; CD30, CD30+ T-cell lymphoproliferative disorder; NK/T, NK/T cell lymphoma, nasal type; DLBCL, diffuse large B-cell lymphoma; SPTCL, subcutaneous panniculitis-like T-cell lymphoma; MZBL, marginal zone B-cell lymphoma; AITL, angioimmunoblastic T-cell lymphoma; BPDCN, blastic plasmacytoid dendritic cell neoplasm; LBL, lymphoblastic lymphoma.
The DLBCL and PTCL subtypes were rarely observed. Of the 68 primary cutaneous peripheral T-cell lymphomas, 4 cases were primary cutaneous aggressive epidermotropic CD8-positive cytotoxic T-cell lymphoma, 8 cases were gamma/delta-positive T-cell lymphoma, and 5 cases were small/medium CD4-positive T-cell lymphoma. Of the 23 cases of primary cutaneous DLBCL, 6 were categorized as DLBCL, leg type.
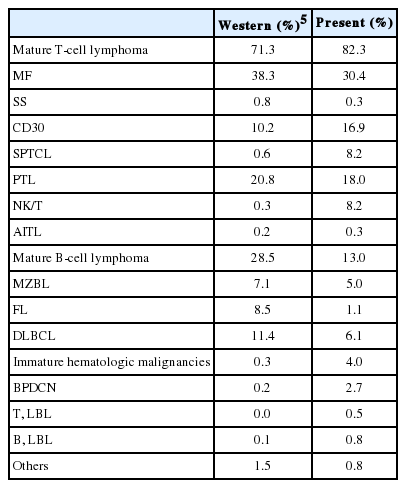
Comparison of lymphoma subtype with sex and age revealed that BPDC neoplasm and T lymphoblastic lymphoma was predominantly associated with males, while CD30+ LPD, SPTCL, and lymphoblastic lymphoma occurred more often in younger individuals (Table 2). Likewise, comparison of lymphoma subtype with the involved anatomical site revealed that marginal zone B-cell lymphoma and B lymphoblastic lymphoma occurred more frequently in the head and neck (Table 3). In addition, the relative incidences of CD30+ LPD, NK/T cell lymphoma, SPTCL, and immature hematopoietic malignancies were higher while those of MF and B-cell lymphoma was lower when compared with one Western study (Table 4).5
DISCUSSION
In the present study we analyzed the incidence rate of Korean cutaneous lymphoma according to the new WHO-EORTC classification. To our knowledge, only a few nation-wide studies of Korean cutaneous lymphoma exist, all of which have several limitations. Specifically, one report focused on systemic lymphoma,1 reporting an incidence of lymphoma subtype very different from the results observed in this study, such as SPTCL being the most common cutaneous lymphoma. One possible explanation for this difference is that the previous report was based on the 2001 WHO classification and described a very limited set of lymphoma subtypes. Other reports have similar limitations.7
With respect to lymphoma subtype and sex, the results of our study were consistent with previous reports.5,8,9 Specifically, we observed a male predominance for the majority of lymphoma subtypes, especially BPDC neoplasm and T lymphoblastic lymphoma, and a female predominance for SPTCL. We also found that most patients were elderly, with a peak incidence around 60 years. As with other systemic lymphomas, aging and age-related effects such as chronic inflammation and diminished immune surveillance may contribute to lymphomagenesis.10
Our study included primary and secondary cutaneous lymphomas. However, the distinction between primary and secondary can be difficult because of incomplete clinical evaluation. Although undetermined cases accounted for only 0.8% of the study population, more problematic cases involving distinction between primary and secondary cutaneous lymphoma may exist. Secondary cutaneous involvement was relatively frequent in NK/T cell lymphoma, AITL, DLBCL, and lymphoblastic lymphoma. Furthermore, almost all of the patients in our study with AITL had systemic lymphoma, indicating secondary cutaneous involvement. AITL skin lesions are nonspecific subtle perivascular lymphoid cell infiltrates without atypia. Further, it is not clear whether such cutaneous manifestations are due to the tumor cell itself or secondary cytokine effects. Thus, immunohistochemical staining for follicular helper T cell markers such as PD-1 and CXCL13 may be helpful in making decisions.
In our study, T cell lymphoma comprised the majority (74.3%) of cutaneous lymphomas, similar to studies conducted in Western countries.3,8,11 MF was the most common primary cutaneous lymphoma. MF displays various histologic appearances mimicking ALCL and PTCL if it transforms into large cells and progresses to the tumor stage from the plaque or patch stage. Before diagnosing ALCL or PTCL, a thorough patient clinical history and physical examination is needed. In the present study, among primary cutaneous lymphomas, the incidence of MF was 30.4%, which was lower than reported for Western and Japanese studies.12,13 The reason for the relatively low incidence of MF in our study was probably due a result of not considering patient's clinical findings. Specifically, some PTCL cases may have belonged to the tumor stage of MF. Of the CD30+ LPD cases, there was disagreement with respect to LyP and ALCL between pathologists. Indeed, distinction of LyP from ALCL requires careful evaluation of clinical parameters and relative percentages of large atypical cells, which is a subjective parameter.
We found that there was a significant difference in incidence compared with Western countries, especially concerning NK/T cell lymphoma and SPTCL. These differences in incidences between countries were very likely the result of viral infection, especially Epstein-Barr virus (EBV) and human T-lymphotropic virus (HTLV). Indeed, EBV positivity is the most important finding in diagnosing NK/T cell lymphoma. Likewise, adult T cell leukemia/lymphoma is associated with HTLV infection and is endemic in several areas of the world, especially in Japan,14 but was rarely observed in the present study.
Two possibilities for the rarity of the incidence of the PTCL subtype can be suggested. First, this study selected cases from 2006. Compared with the 2001 WHO classification, primary cutaneous aggressive epidermotropic CD8-positive cytotoxic T-cell lymphoma, primary cutaneous γδ T-cell lymphoma, and primary cutaneous small/medium CD4-positive T-cell lymphoma were included as a provisional entity in the new WHO-EORTC classification. Thus, the hemato/dermatopathologist would likely miss these cases. Second, it was difficult to differentiate the PTCL subtype from other cutaneous T-cell lymphomas. For example, primary cutaneous gamma-delta T-cell lymphoma was previously described as SPTCL with a gamma/delta phenotype that shares common morphologic and immunophenotype features. The most important immunophenotype marker for this type of disease is TCRδ, for which detection has recently become available. As such, negativity for βF1 favors a diagnosis of gamma/delta T-cell lymphoma if TCRδ is not appropriate.15 More immunohistochemical staining results for βF1 and TCRδ are needed in cases of PTCL and SPTCL.
Subtypes of DLBCL were rarely observed in this study. Primary cutaneous DLBCL, leg type, presents on the leg, although other cutaneous sites may be involved. Furthermore, tumor cells of DLBCL, leg type, typically express Bcl2, Bcl6, and MUM1, although approximately 10% of cases do not express either Bcl2 or MUM1.16 By definition, DLBCL comprises all other cases other than those belonging to DLBCL, leg type, and to date only one marker, Bcl6, has been found to be useful in distinguishing between these two subtypes. One study investigated chromosomal aberrations in two subtypes of DLBCL and found similar aberrations irrespective of anatomical site, cell morphology, and Bcl2 expression.17 Among cases of cutaneous B-cell lymphoma, marginal zone B-cell lymphoma was relatively common while follicular lymphoma was rare; these findings were correlated with the results of previous lymphoma studies performed on Korean1 and Japanese populations.13
In addition PTCL and DLBCL subtypes, it is also important to pay attention to BPDC neoplasm, which is newly described and included in 4th edition of WHO classification. BPDC neoplasm is a subset of acute myeloid leukemia, related to precursor neoplasms,4 and is a clinically aggressive tumor derived from the precursors of plasmacytoid dendritic cells and characterized by a diffuse infiltration of blastic cells with irregular nuclei, fine chromatin and small nucleoli. BPDC neoplasm frequently involves the skin, and has also been described as blastic NK-cell lymphoma.2 Immunohistochemical staining for CD4, CD56, and CD123 is essential to confirm the diagnosis.
Regretfully, we were unable to evaluate patient outcome associated with the new WHO-EORTC classification system. Thus, further studies concerning patient prognosis and efficacy of different treatment modalities are needed. However, our data were collected from many hospitals where hematopathologists involved in a large number of cases performed the reviews, and included all kinds of cutaneous lymphoma subtypes. In spite of limitations such as absence of comprehensive review of submitted cases, this study may represent the current status of cutaneous lymphoma subtypes in Korea according to new WHO-EORTC classification.
In conclusion, compared with Western countries, mature T-cell lymphoma was found to be more frequent in Korean patients because of the frequent occurrence of CD30+ LPD, SPTCL, and NK/T cell lymphoma. Conversely, there were fewer cases of B-cell lymphoma, especially follicular lymphomas. The new WHO-EORTC classification system is expected to contribute to uniform diagnosis in cutaneous lymphoma, and thus pathologists and dermatologists should recognize and adapt their diagnoses accordingly.
Acknowledgments
This research was supported by a grant from The Korean Society of Pathologists.
Notes
No potential conflict of interest relevant to this article was reported.