Multifocal Osteosarcoma of the Skull: Multiple Primary or Metastatic? A Case Report
Article information
Abstract
Osteosarcoma of the skull is a very rare condition. Moreover, it is extremely rare for osteosarcoma to present as multiple lesions confined to the skull. A 58-year-old woman was admitted with two masses in the parietal area of the skull, accompanied by mild headache and tenderness. Imaging revealed two masses with a heterogeneous consistency in the cranial bones. Excision craniectomy was performed and the pathology was consistent with osteoblastic osteosarcoma. Two nodules in the heart were found on routine follow-up imaging while the patient was undergoing chemotherapy. The nodules were biopsied and found to be metastatic osteosarcoma.
Osteosarcoma is a malignant, bone-forming tumor that usually arises from the metaphyseal plates of the long bones. Primary osteosarcoma of the skull is a rare disease that makes up approximately 2% of all osteosarcomas.1,2 Multifocal osteosarcoma of the skull is exceedingly rare, with only 2 cases reported.3,4 In this paper, we present a case of multifocal osteosarcoma of the skull in a patient without a history of radiation or predisposing conditions such as Paget's disease.
CASE REPORT
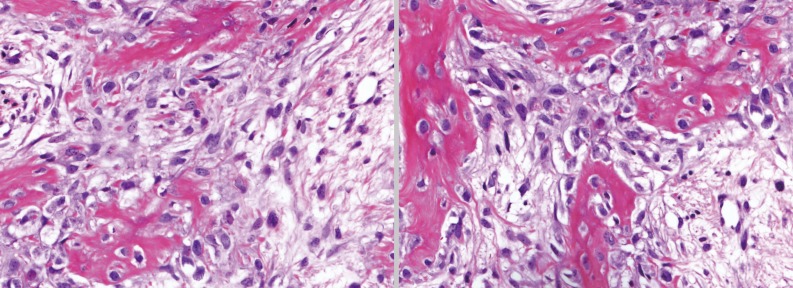
A 58-year-old woman presented to our institution with a tender mass located in the parietal bone. The mass was first discovered 3 weeks prior during a visit to a local clinic. After primary evaluation at a local clinic that included radiologic evaluation through computerized tomography (CT) and magnetic resonance imaging (MRI) she was referred to our institution for further diagnosis and treatment. On admission, she complained of mild headache and tenderness of the lesion was present on exam. She had no neurologic symptoms. All laboratory results were within normal ranges, including alkaline phosphatase. She had no personal history of radiation, malignancy, or family history of malignancy. Physical examination revealed two lesions with mild tenderness on the parietal area of the skull. Simple X-ray of the skull showed two expansile masses with subtle perpendicular periosteal reaction and Codman's triangle, which suggested malignant bone tumors (Fig. 1). A MRI of the skull revealed two masses located in the parietal bones that measured 2.0×2.0 cm (right) and 4.0×3.3 cm (left) (Fig. 2). The distance between the two masses measured 1.7 cm. Both masses showed iso-signal intensity in T1-weighted images and mixed signal intensity in T2-weighted images. The smaller mass on the right was limited to the calvarium, while the larger mass on the left, which appeared as a bulging contour on the scalp, extended to the subgaleal and epidural spaces and exerted a mass effect on the adjacent frontal lobe. After Gd-DTPA enhancement, both masses were well-enhanced, but had areas with cystic components or low-signal intensity that did not enhance well. Fluid attenuation inversion recovery and T2-weighted images showed small areas with high-signal intensity. Positron emission tomography-CT was also performed prior to surgery, but no other lesions were found. Based on these radiologic findings, a preliminary diagnosis of osteosarcoma was made.
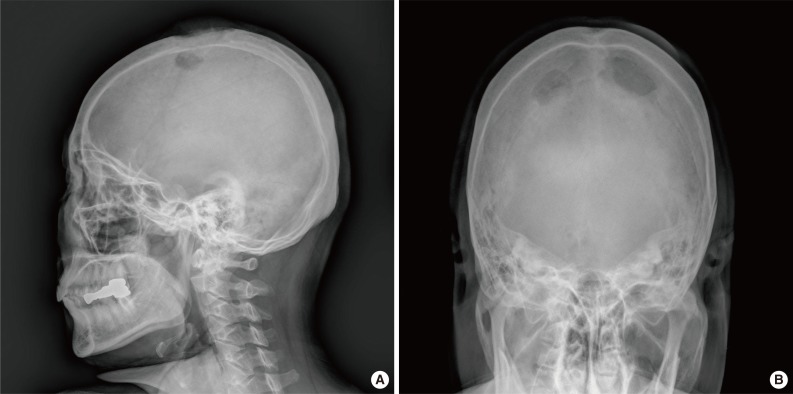
Plain X-ray image of the mass. (A) Sagittal, simple X-ray image of the skull. (B) Town's view simple X-ray image of the skull.
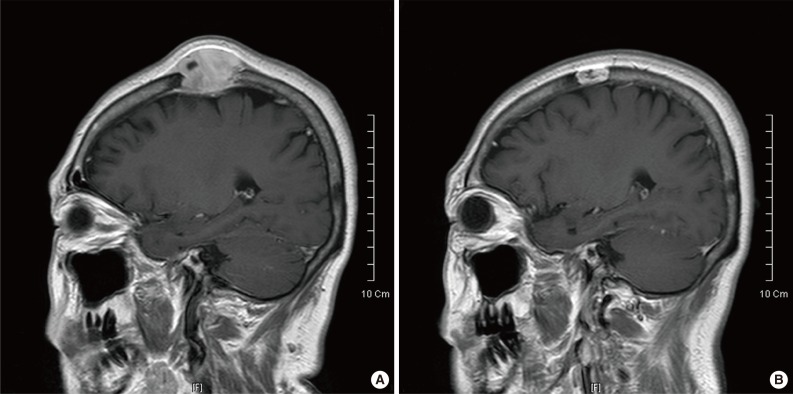
Magnetic resonance imaging (MRI) image of larger and smaller mass. (A) MRI image of the larger mass. Sequence 7/20. (B) MRI image of the smaller mass. Sequence 15/20.
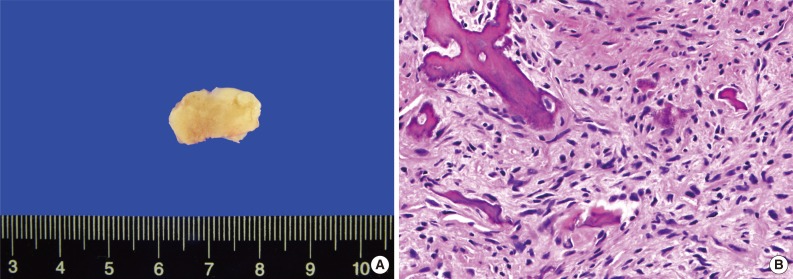
The patient subsequently underwent partial craniectomy without preoperative biopsy. The specimen was made up of fragments of bone and soft tissue approximately 7×7×3.5 cm and 3×2.5×1 cm in size (Fig. 3). Microscopically, the larger mass showed foci of highly cellular areas that contained elongated and round osteoblastic cells, displaying nuclear atypism, pleomorphism, and prominent nucleoli. These cells were producing immature abnormal osteoid (Fig. 4). Mitotic figures were frequently observed. The smaller mass showed moderate cellularity and also showed anaplastic osteoblastic cells with malignant osteoid (Fig. 5). The differential diagnosis for intramedullary osteoid-forming tumors should include some sarcomas and benign lesions like osteoblastomas, osteoid osteomas, and fibrous dysplasia. The presence of so-called malignant osteoid, which consists of anaplastic osteoid-producing cells and an osteoid matrix, and tumor cells showing severe pleomorphism and prominent nucleoli, should rule out those impressions. Therefore, a pathologic diagnosis of high-grade osteoblastic osteosarcoma was made.
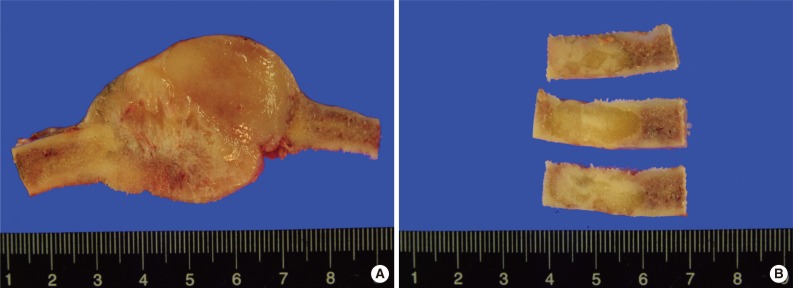
Gross image of larger and smaller mass. (A) Gross cross-sectional view of the larger mass. (B) Gross cross-sectional view of the smaller mass.
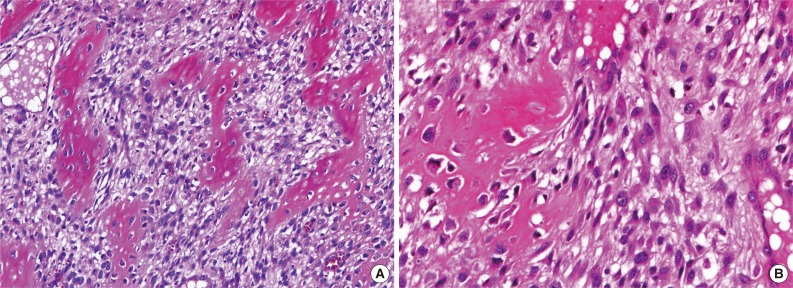
Microscopic images of hematoxylin and eosin slides from larger mass. (A) Microscopic view of the larger mass. Round and spindle cells with moderate atypia are seen. (B) High power view of the larger mass. This area shows high grade osteosarcoma.
Our patient began adjuvant chemoradiotherapy 2 months after surgery, but two masses with heterogeneous consistency were found in the heart, in the left atrium and on the mitral valve, on routine follow-up CT imaging. The larger nodule in the left atrium-a whitish firm mass with calcifications measuring 1.8×1.0 cm (Fig. 6A)-was excised and submitted for pathologic evaluation. Microscopic examination revealed atypical round and spindle-shaped cells forming lace-like osteoid (Fig. 6B). The diagnosis was metastatic osteosarcoma. Bone scintigraphy with Tc-99m was performed 4 months after the surgery; however, no specific lesion was found. At the time of writing, the patient was undergoing systemic chemotherapy with close follow-up without evidence of disease recurrence or progression.
DISCUSSION
Osteosarcoma is a malignant, bone-forming neoplasm. The age-adjusted incidence rate for all bone and joint malignancies for all ages and populations is 0.9 per 100,000 persons per year. Osteosarcoma comprises approximately 35% of these cases, making it the most common form of bone and joint malignancy, followed by chondrosarcoma (25%), and Ewing sarcoma (16%).2 Although osteosarcoma can occur in any bone, it most often occurs near the metaphyseal plates of the long bones. The most common sites are the femur (42%, with 75% in the distal femur), tibia (19%, with 80% in the proximal tibia), and humerus (10%, with 90% in the proximal humerus). Other common sites of occurrence are the craniofacial bones (8%) and pelvis (8%), while the incidence rate of primary osteosarcoma of extragnathic craniofacial bones is 2% of all osteosarcomas.2,5,6 Osteosarcoma has a bimodal age distribution. The first peak occurs during adolescence and the second peak occurs in adults older than 65. In the latter age group it is more likely to be a secondary malignancy, commonly related to Paget's disease.2 Our patient did not have any history of Paget's disease and had a normal alkaline phosphatase level on admission.
A multifocal osteosarcoma of the skull is an even rarer entity among cases of extragnathic osteosarcoma. While multifocal osteosarcoma is reported in 1% to 3% of cases,7 we found only two cases of multifocal osteosarcoma involving only the skull at the time of diagnosis.3,4
There is debate over whether multifocal osteosarcoma consists of multiple primary tumors or metastatic lesions. Multifocal osteosarcoma is thought to consist of multiple primary tumors if several symmetric bone lesions are discovered simultaneously, and are similar in size and histology. Multiple primary tumors are also more likely when there is another bony lesion and an absence of metastasis to the lung, suggesting that there is no obvious route by which metastasis can occur.7,8 However, the most recent reported cases of multifocal osteosarcoma are thought to be metastatic for several reasons. Typically, when a larger dominant tumor exists, the largest lesion tends to be the primary tumor. Bone-to-bone metastasis can occur through Batson's venous plexus or marrow sinusoid, and lymphatic spread is also possible. Finally, in these cases, there was a correlation between the dominant lesion and other lesions in terms of response to chemotherapy.7 In our case, with features such as obvious distant metastasis and presence of a dominant lesion, the process is thought to be metastatic rather than multiple primary tumors.
The classification suggested by Amstutz9 is commonly used for multifocal osteosarcoma. It classifies multifocal osteosarcoma into types I and II, which are further subdivided into child/adolescent high grade and adult low grade. Metachronous cases are classified as type III.9 Our case would be classified as type II by the age and synchronicity of the multifocal lesions, but it also bears a number of features that do not fit the characteristics of the category. Type II cases are described as extraskeletal sclerotic masses of low grade osteosarcoma without distant metastatic lesions, while our case was an intraskeletal mass of high grade osteosarcoma with metastatic lesions in the heart.
This is a case of multifocal osteosarcoma with an unusual patient age and metastatic location. Our patient is considered to have metastasis rather than multiple primary tumors, and distant metastatic lesions of the heart were also found. Therefore, when clinicians diagnose multifocal osteosarcoma with a dominant mass, the possibility of the presence of distant metastasis must be considered and thorough work-ups should be performed.
Notes
No potential conflict of interest relevant to this article was reported.