Bilateral Stafne Bone Cavity in the Anterior Mandible with Heterotopic Salivary Gland Tissue: A Case Report
Article information
Stafne bone cavity is a well demarcated defect of the mandible, usually asymptomatic and located in the posterior portion of the bone.1 Most cases have been reported in male patients between the age of 50 and 70 years.2 This lesion has been labeled with various terms, including ectopic salivary gland, idiopathic defect, mandibular salivary gland inclusion, Stafne bone cavity and cyst.2 The cavities are often filled with normal salivary gland tissue, but occasional cases showed cavity contents that included skeletal muscle, fibrous connective tissue and adipose tissue.1,2 Bilateral Stafne bone cavity of the anterior mandible is extremely rare and only seven such cases have been reported previously.2 Herein, we report a case of bilateral Stafne bone cavity of the anterior mandible.
CASE REPORT
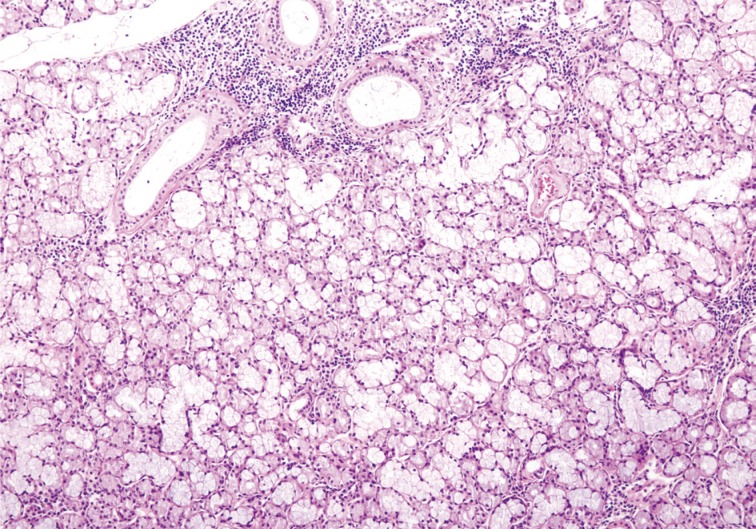
Two well demarcated ovoid radiolucent lesions (right, 3.9×1.5 cm and left, 2.9×1.1 cm) were found incidentally in the anterior mandible of a 44-year-old female patient on her panoramic dental X-ray (Fig. 1). The patient did not show any symptom of radiolucencies. The radiological findings were interpreted as radicular cysts. Two fragments of tissue from the cavities were submitted for histological diagnosis. The biopsied tissue fragments showed normal salivary gland tissue with mixed serous and mucinous cells. These findings were otherwise unremarkable, except for the small amount of lymphoid cell infiltration that was discovered (Fig. 2). The clinical, radiological, and pathological findings were consistent with Stafne bone cavity.
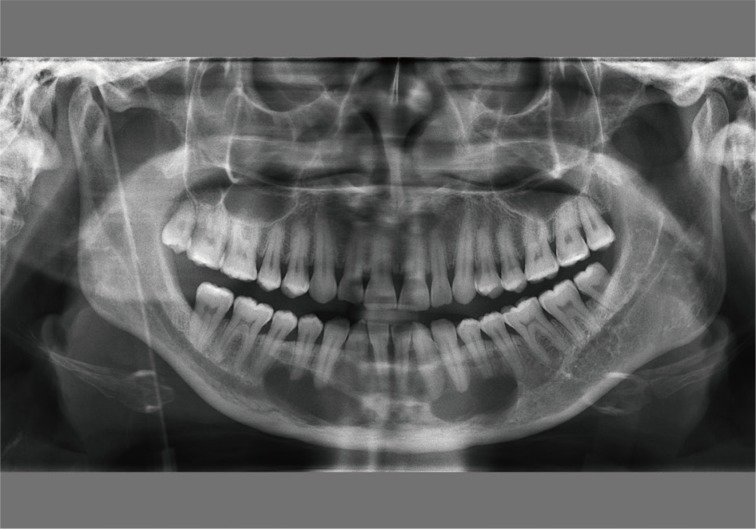
Panoramic dental X-ray shows two radiolucencies beneath the apices of the canine and premolars in the right and left anterior mandible.
DISCUSSION
Since Stafne bone cavities were first reported in 1942, most cases have been found in the posterior mandible.3 However, these cavities were found also in the anterior portion of mandible in 1957 by Richard and Ziskind.4 Until now, only approximately fifty cases of anterior Stafne bone cavities have been reported.2
Similar to Stafne bone cavities located elsewhere in the mandible, anterior lesions show a wide age range (18 to 68 years) and higher prevalence in males (3:1, males:females).2 Most Stafne bone cavities are diagnosed on radiology, and only clinical follow-up with additional radiographic examination is sufficient unless there are symptoms or progression. The rarity of anterior Stafne bone cavities causes confusion and can hinder accurate and prompt diagnosis of this condition. Because the cavities resemble other periapical radiolucencies, they can appear similar to other cysts or tumors.2,5,6 The differential diagnosis of bilateral lesions includes, salivary gland tumors, fibro-osseous lesions, traumatic bone cysts, central giant cell lesions, hyperparathyroidism, ameloblastoma, eosinophilic granuloma, hemangioma, myxoma aneurysmal bone cyst, multiple myeloma, benign neurogenic tumors and arteriovenous fistula. Unlike tumors or the cysts, most Stafne bone cavities are asymptomatic and are therefore found accidentally.
In most cases, the content of the cavities was salivary gland tissue, and these lesions were sometimes referred to as heterotopic salivary glands. The salivary gland tissue contents suggeseted congenital malformation theory for the pathogenesis of the cavities,1 which states that the salivary gland tissue is congenitally entrapped within the mandible. Pressure from adjacent structures, including the hypertrophied salivary glands and facial arteries, has also been suggested as a possible pathogenic cause of Stafne bone cavities.7 A large-scale study of mandibular marrow tissue revealed the presence of intraosseous salivary gland tissue.8 As the authors of the article pointed out, such intraosseous heterotopias can serve as a pathogenic explanation and this finding can be interpreted as evidence supporting the former pathogenic theory of Stafne bone cavity formation. Our case lacks previous history and therefore, we were not able to determine the cavity's pathogenic cause. However, lymphocytic infiltration, which has been suggested as one of the causes of hypertrophied salivary glands in the pressure-induced acquired pathogenesis theory, is present in our case and therefore might be interpreted as a backup evidence for the theory.3
Although most Stafne bone cavities generally do not present any complications, there is one report of a Stafne bone cavity harboring pleomorphic adenoma.9 If a surgical specimen of the Stafne bone cavity is acquired, histological examination of the entire specimen is preferable for the detection of a possible salivary gland tumor within the specimen.
Because anterior Stafne bone cavity is very rare, accurate diagnosis of the lesion is challenging for clinicians.10 Pathologists should be aware of this lesion, because biopsies are performed in some cases and the cavity can harbor a salivary gland tumor.
Notes
No potential conflict of interest relevant to this article was reported.