Cytotoxic Variant of Mycosis Fungoides with CD8+ CD56+ Phenotype: A Case Report and Review of Literature
Article information
Mycosis fungoides (MF) is the most common cutaneous Tcell lymphoma. Approximately 50% of all primary cutaneous lymphomas are MF[1]. These lymphomas are comprised of epidermotropic collections of small- to medium-sized T lymphocytes with cerebriform nuclei. The neoplastic cell shows a mature CD3+, CD4+, CD45RO+, CD8– memory T-cell phenotype. However, rarely, MF with a CD4–, CD8+ cytotoxic T-cell phenotype has been reported[2-5]. The World Health Organization (WHO)-European Organization for Research and Treatment of Cancer (EORTC) classification for cutaneous lymphomas describes three types of cutaneous lymphomas that express CD56: 1) subcutaneous panniculitis-like T-cell lymphoma, 2) extranodal natural killer (NK)/T-cell lymphoma, nasal type, and 3) CD4+/CD56+ hematodermic neoplasm (blastic NKcell lymphoma)[1]. However, the report does not mention, MF with CD56 expression. Earlier in 2003, a report by the EORTC cutaneous lymphoma task force workshop described cytotoxic/natural killer cell cutaneous lymphomas and divided them into eight categories[6]. One of these categories was the CD56+, cytotoxic variant of MF. This report presents a rare CD8+, CD56+ variant of MF having the cytotoxic phenotype.
CASE REPORT
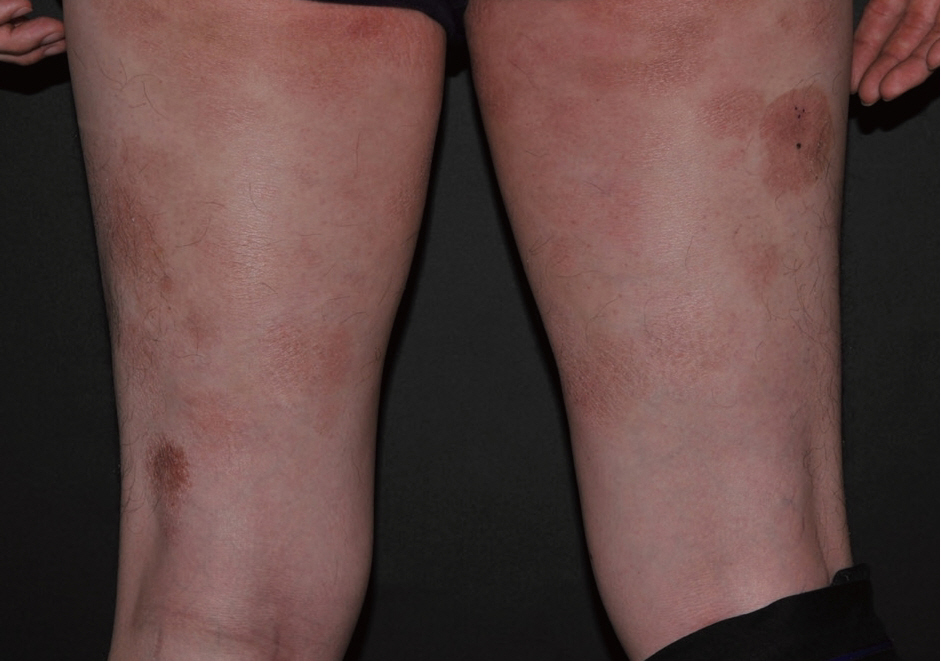
A 40-year-old male presented with a 5-year history of multiple round erythematous to dusky, brownish scaly patches with mild pruritus (Fig. 1). The skin involvement measured about 30% of total body surface. The lesions appeared first on the buttock and thigh, and lately on the upper arm. The skin lesions did not respond to topical corticosteroid treatment, at which time, he visited our hospital. A skin biopsy was taken from the thigh. The specimen showed a prominent band-like lymphocytic infiltration in the superficial dermis with epidermotropism (Fig. 2A). The epidermotropic lymphocytes were small- to medium-sized with an irregular nuclear membrane and coarse chromatin (Fig. 2B). The immunophenotype of the cells in the epidermis and a few cells in the superficial dermis were CD3+, CD4–, CD8+, CD56+, CD30–, and CD20– (Fig. 2C, D). The majority of lymphocytes in the superficial dermis were not atypical, in contrast to the epidermotropic lymphocytes, and were positive for CD4 and CD8. The neoplastic cells were positive for beta F1 (a marker of alpha/beta T lymphocytes) and granzyme B. An Epstein-Barr virus–encoded small non-polyadenylated RNA-1 (EBER-1) signal was not detected. Lactate dehydrogenase was elevated to 432 IU/L (range, 200 to 400 IU/L). Laboratory blood tests revealed an elevated, total cholesterol level of 235 mg/dL (range, 125 to 220 mg/mL). Complete blood cell count and other results of blood chemistry were within the normal range. The chest X-ray and positron emission tomography–computed tomography revealed no abnormal findings and there was no lymphadenopathy. The patient was diagnosed as having the stage IB, CD8+, CD56+ cytotoxic immunophenotype variant MF. He was treated with narrowband ultraviolet B therapy and his condition was stabilized.
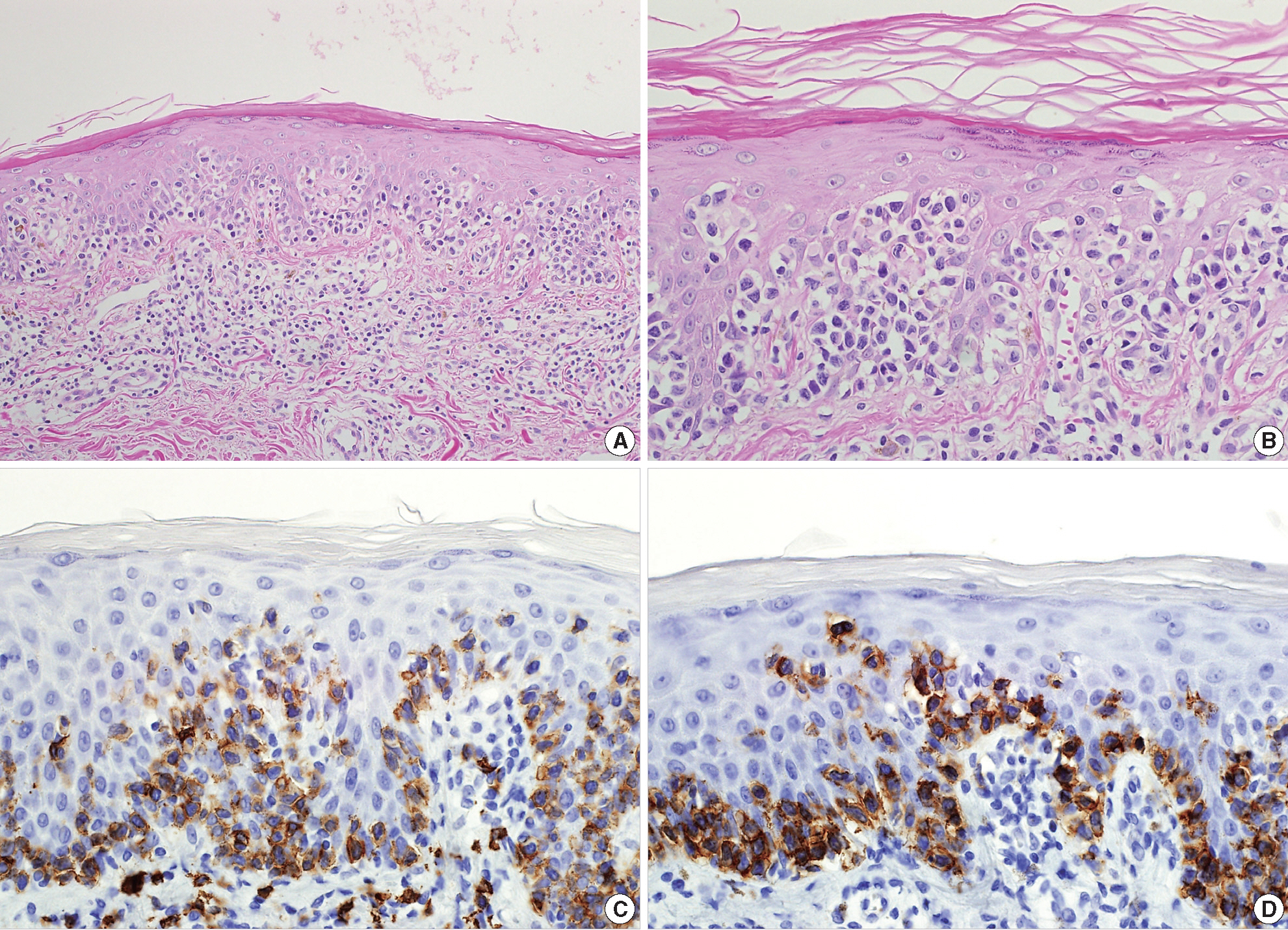
(A) The specimen shows a prominent band-like lymphocytic infiltration with epidermotropism. (B) The epidermotropic lymphocytes are small- to medium-sized with an irregular nuclear membrane and coarse chromatin. These cells display the cytotoxic phenotype, showing CD8 (C) and CD56 (D) immunoreactivity.
DISCUSSION
Prognosis of classic MF depends on stage, and, in particular, on the type and extent of skin lesions, as well as the presence of extracutaneous disease[1]. Patients with limited patch/plaque-stage MF have a similar life expectancy to an age, sex, and race-matched control population[1]. However, the prognosis of MF with the cytotoxic phenotype, especially when it express CD56, is not well established.
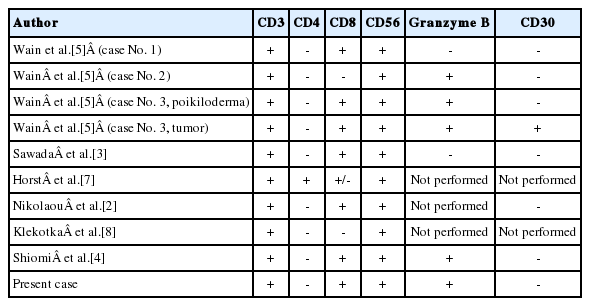
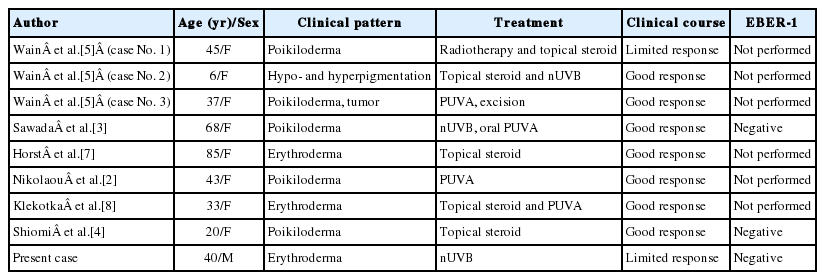
To date, there are 8 cases of CD56-expressing MF reported in the current literature, and our case is the ninth case report. The immunohistochemical and clinical characteristics of these cases are summarized in Tables 1 and 2. Among the nine cases, six cases co-expressed CD8 in a majority of the neoplastic cells, one co-expressed CD8 in a minority of neoplastic cells, and two were negative for CD8. One out of nine cases was positive for CD4. Age range was broad, from 6- to 85-years-old. Eight cases were females and our case was the only male case. Poikiloderma was the most frequent clinical feature at the time of diagnosis. Seven cases showed good response to the therapy while two cases, including our case, showed limited response. None of the cases, including our case, had an aggressive clinical course. This result suggests that CD56+ MF is a disease with good prognosis similar to classic MF.
Several reports of MF with CD8+ and/or CD56+ expression have suggested that this variant would have no prognostic difference compared with classic MF[2,3,5,7-10]. Massone et al.[9] analyzed 73 biopsy specimens from 68 patients with early MF and divided them into four groups based on the immunophenotype. They stated that there was no statistical difference between the survival curves of the four groups, and therefore concluded that cytotoxic phenotype does not have any prognostic significance.
In our case, with the observed immunophenotype, we considered different diagnoses including primary cutaneous aggressive epidermotropic CD8+ cytotoxic T-cell lymphoma, primary cutaneous gamma/delta T-cell lymphoma, and extranodal NK/T-cell lymphoma, nasal type. We were able to rule out these different diagnoses based on the following: clinical course and presentation, beta F1 positivity, and EBER-1 negativity.
In conclusion, we present a case of a cytotoxic variant of MF with a CD8+, CD56+ immunophenotype. MF with cytotoxic immunophenotype is characterized by a typical clinical presentation, histology, and course of MF. Clinical presentation and course should be a primary consideration in diagnosis. We emphasize that it is important to recognize this rare variant of MF and to distinguish it from other aggressive cutaneous lymphomas to avoid aggressive treatment.
Notes
No potential conflict of interest relevant to this article was reported.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011-0012351).