Tumor-to-tumor metastasis: metastatic invasive lobular carcinoma of the breast within adenocarcinoma of the lung
Article information
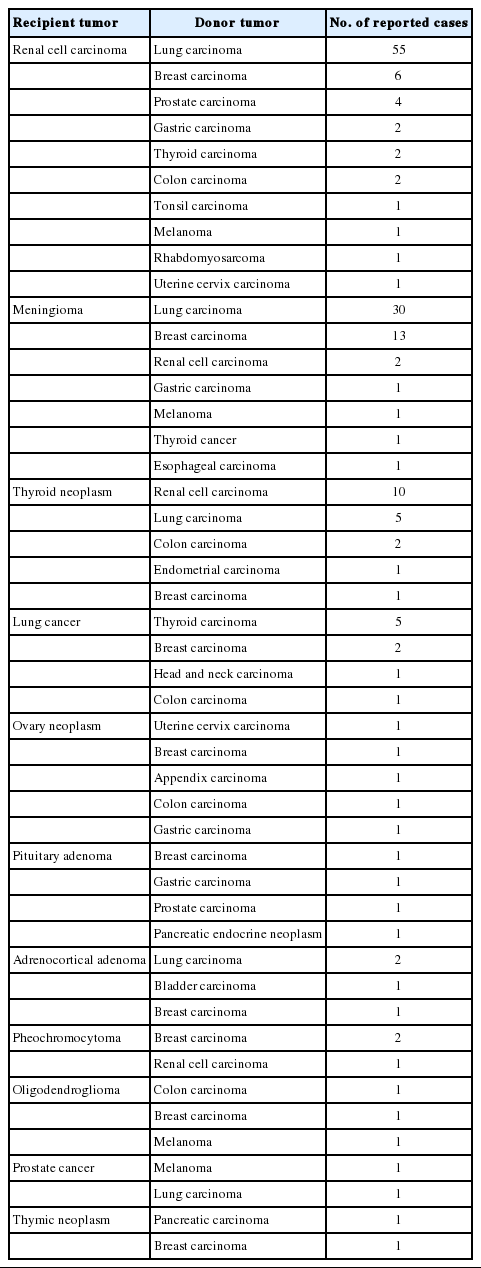
Tumor-to-tumor metastasis (TTM) is an extremely rare phenomenon in patients with multiple synchronous or metachronous primary malignancies. Previous studies reported that renal cell carcinoma and meningioma are the most common recipients of TTM, whereas the most prevalent donors are lung and breast carcinomas [1]. Although the lung is one of the organs most vulnerable to metastases, a lung carcinoma is one of the most rare recipients of TTM. To the best of our knowledge, only two cases of lung carcinoma harboring metastatic breast carcinoma have been reported in English literature [2]. Herein, we report another TTM case in which an invasive lobular carcinoma of the breast metastasized to a lung adenocarcinoma.
CASE REPORT
A 52-year-old woman’s medical check-up and ultrasonography revealed a 6.2-cm-sized mass in the right breast, which was diagnosed as invasive lobular carcinoma by needle biopsy. Before surgery, the patient underwent a full-body evaluation. Computed tomography revealed a mass in the right lung, which was diagnosed as pulmonary adenocarcinoma by needle biopsy (Fig. 1). Since the patient was suspected to have synchronous primary carcinomas in her lung and right breast with no sign of metastasis, she underwent right lower lobectomy for the lung adenocarcinoma and right mastectomy for the invasive lobular carcinoma of the right breast. The lung mass measured 2.3 cm in diameter. Microscopically, most of the lung mass exhibited typical growth patterns of lung adenocarcinoma. However, in one focus, the tumor cells showed a different arrangement and cytology; the tumor cells had minimal cytoplasm without nucleoli in a compact trabecular pattern. The typical adenocarcinoma cells were positive for thyroid transcription factor-1 (TTF-1) and E-cadherin and negative for estrogen and progesterone receptors. In contrast, tumor cells in the morphologically different focus expressed immunoreactivity for estrogen and progesterone receptors while they were negative for TTF-1 and E-cadherin (Fig. 2). Based on these findings, we concluded that the invasive lobular carcinoma of the patient’s right breast had metastasized to the lung adenocarcinoma. This study was approved by the Institutional Review Board of Jeonbuk National University Hospital with a waiver of informed consent (IRB No. 2019-05-027).
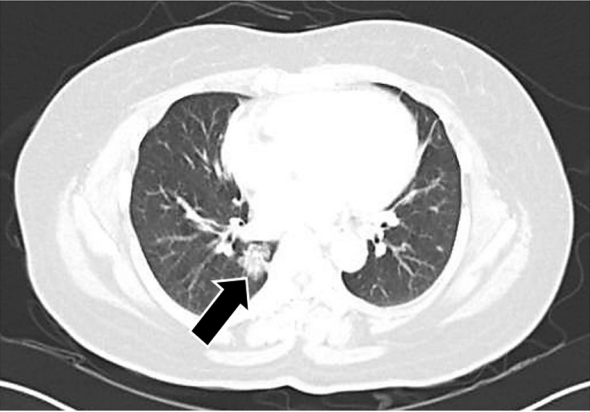
High resolution view of computed tomography scan shows pulmonary mass (arrow). The mass is located at right lower lobe of the lung and shows ground glass opacity.
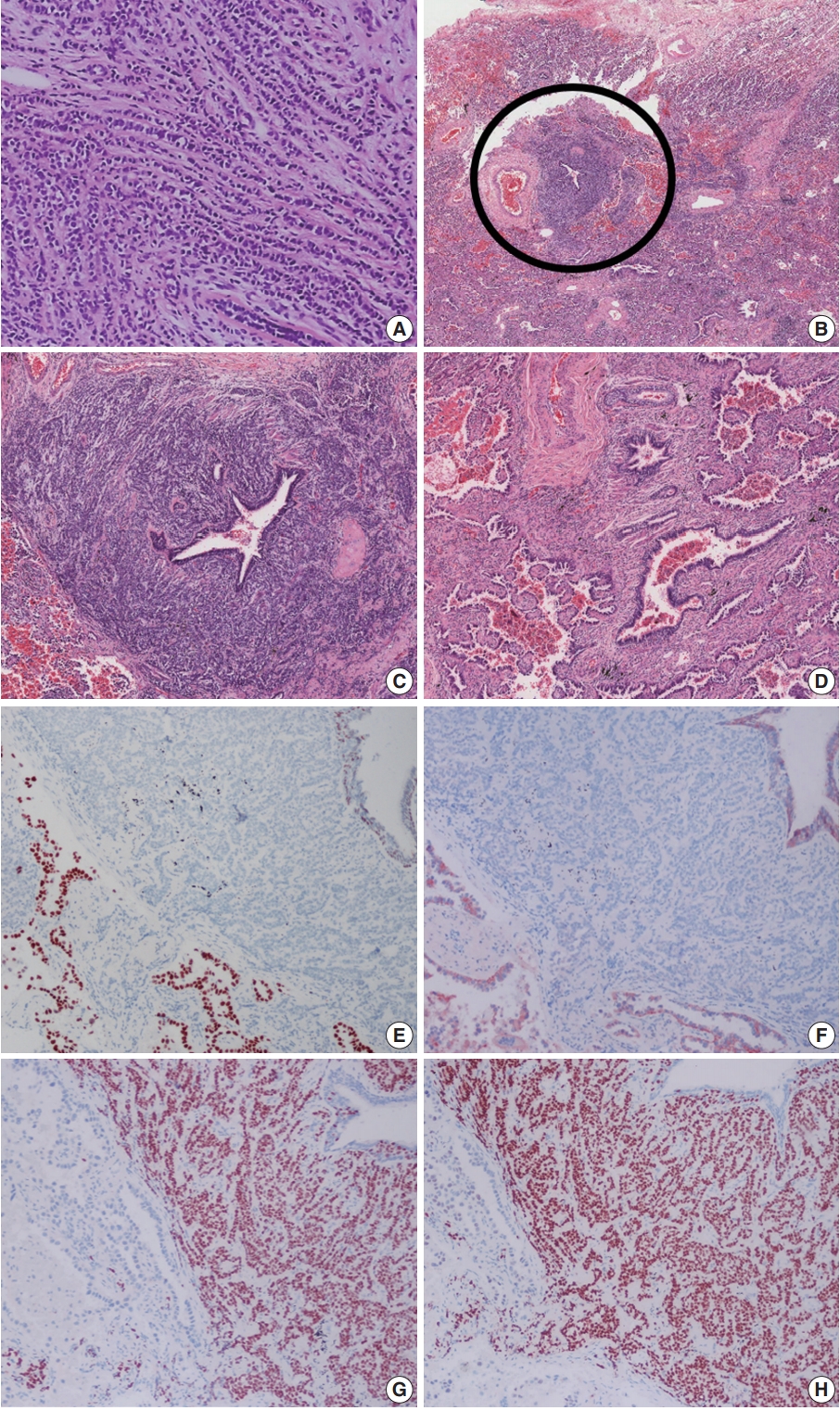
Histologic features of the breast needle biopsy and resected lung mass. (A) The tumor cells of the breast mass are arranged in infiltrating single linear cords. (B) Scan view of the pulmonary mass shows dimorphic growth pattern (circular area vs. other region). (C) Higher magnification of the circular area of Fig. 2B. The tumor cells are arranged in compact trabecular pattern with minimal cytoplasm. (D) Other region of the lung mass showing typical acinar growth pattern. The tumor cells of the circular area of panel B are negative for thyroid transcription factor-1 (E) and E-cadherin (F) and positive for estrogen (G) and progesterone receptor (H).
DISCUSSION
TTM is an extremely rare phenomenon. Moreover, only approximately 180 cases have been reported in English literature. The most referenced and used criteria to diagnose TTM were proposed by Campbell et al. [3] as follows: (1) more than one primary tumor must be present; (2) the recipient tumor must be a true benign or malignant neoplasm; (3) the metastatic neoplasm must be a true metastasis with established growth in the host’s tumor, not the result of contiguous growth (‘collision tumor’) or embolization of tumor cells; and (4) tumors that have metastasized to the lymph nodes with existing lymphoreticular malignant tumors are excluded.
According to previous reports, renal cell carcinoma and meningioma are common recipient tumors of TTM (Table 1) [1]. They are both rich in vasculature and have high cytoplasmic lipid and glycogen content [4]. These conditions might be able to serve as a favorable microenvironment for disseminated cancer cells to metastasize. The lung is one of the most frequent sites of metastasis for extrathoracic malignancies. However, lung carcinomas are extremely rare to serve as a recipient tumor in a TTM phenomenon [1,2,5-7]. A possible explanation for this paradox is that lung carcinomas, when compared with normal lungs, are often accompanied by fibrosis and are lacking in the rich network of thin-walled vasculature [6,8]. Additionally, most lung carcinomas grow rapidly; therefore, they are less likely to provide enough nutrition for the immigrant cancer cells than renal cell carcinoma or meningioma [8].
A lung mass detected in a patient with a history of prior cancer proves to be a big challenge to clinicians, radiologists, and pathologists. Even worse, in TTM cases like our patient, it is nearly impossible for a radiologist to detect the metastatic lesion located inside the primary tumor. Besides, the needle biopsy, if not containing both primary and metastatic tumors of the mass, could be of no use. In our study, we interpreted the needle biopsy of the lung mass as a primary lung adenocarcinoma. Even after evaluation of the resection specimen, it is not an easy task to detect the metastasis whose focus is small and embedded in the recipient tumor. Therefore, if pathologists identify a histologically different focus in a morphologically typical primary lung tumor of a patient with two different primary cancers, they should always take TTM occurrence into consideration despite the slim chance.
In conclusion, we report a rare case of an invasive lobular carcinoma of the breast metastasizing to a lung adenocarcinoma. To avoid an incorrect diagnosis of a tumor with dimorphic appearance, the TTM phenomenon should be considered as a possibility. Moreover, it is of great importance to identify metastases because metastatic and non-metastatic tumors require different treatments.
Notes
Author contributions
Conceptualization: KMK, MJC.
Data curation: ARA, KMK.
Investigation: ARA, KMK.
Writing: MJK, KMK.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding
No funding to declare.