Cytologic Findings of Clear Cell Adenocarcinoma of the Urethra: A Case Report
Article information
Abstract
Clear cell adenocarcinoma of the urethra is a rare disease entity with an uncertain histogenesis. Here, we present a case of primary clear cell adenocarcinoma of the female urethra with its cytological findings. A 54-year-old woman presented with a painless gross hematuria lasting 3 months. On vaginal sonography, there was a sausage-like, elongated mass in the urethra, measuring 3.8×4.3 cm. The voided urine cytology revealed small clusters of rounded or papillary cells. The necrotic debris and inflammatory cells were present within some clusters of tumor cells. These tumor cells were enlarged and had abundant clear or granular cytoplasm with cytoplasmic vacuoles. The nucleus was granular and contained vesicular chromatin with prominent nucleoli. The hobnail cells and hyaline globules were also present as in a histologic section. The histologic findings were compatible with clear cell adenocarcinoma. The tumor showed distinctive cytological features. Cytologically, however, it is necessary to make a differential diagnosis from other adenocarcinoma or high-grade urothelial carcinoma.
Clear cell adenocarcinoma (CCA) of the urethra is a rare disease entity. To date, it has been described on several case reports or a small series of collective cases have been reported.1-5 It commonly occurs in women aged between 35 and 80 years (mean, 58 years).1 Its histological findings are well known and are identical to those of the female genital tract. However, the cytological findings have been less described and only two cases have been reported in the English literature.6,7 Here, we report cytological findings of the CCA of the female urethra with a review of literatures.
CASE REPORT
A 54-year-old woman presented with a painless, gross hematuria lasting three months. The patient had undergone a hysterectomy 24 years previously because of the uterine cancer. The patient had frequency, residual urine sensation, nocturia and edema of the left leg. On vaginal sonography, there was a 3.8×4.3 cm sized solid mass in the urethra which bulged to the wall of the urinary bladder (Fig. 1A). The upper part of the lumen of the urinary bladder was clear. The computed tomographic urography revealed a 4-cm low attenuated mass with a cystic portion adjacent to the vaginal stump (Fig. 1B). Many metastatic lymph nodes of 0.5-3 cm in size were present in both the paraaortic space and the pelvic cavity. Based on urine cytology findings, the patient diagnosed with adenocarcinoma. On the surgical field, the patient had a lobulated tumor mass of about 3 cm in diameter in the urethra and had the clear urinary bladder.
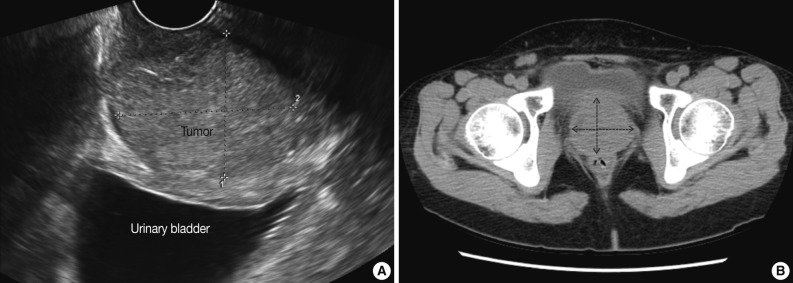
(A) Vaginal sonography. There is a 3.8×4.3 cm-sized solid mass in the urethra which bulges to the urinary bladder wall. (B) The computed tomographic urography. There is a 4-cm low attenuated mass with cystic portion adjacent to the vaginal stump (arrows).
Cytological findings
The voided urine cytology revealed moderate cellularity with small clusters of globular or papillary cells in the inflammatory background (Fig. 2A). The necrotic debris and inflammatory cells were present within some clusters of tumor cells (Fig. 2B). These tumor cells were enlarged and had abundant clear or granular cytoplasms with cytoplasmic clear vacuoles. Some clusters showed hobnail features (Fig. 2C). The nucleus showed granular or vesicular chromatin with prominent nucleoli. It was enlarged and had a round shape with folded, irregular nuclear membrane. It showed a moderate nuclear pleomorphism (Fig. 2C). Small globular hyaline bodies were present in clusters of tumor cells (Fig. 2D). Benign urothelial cells were rarely observed.
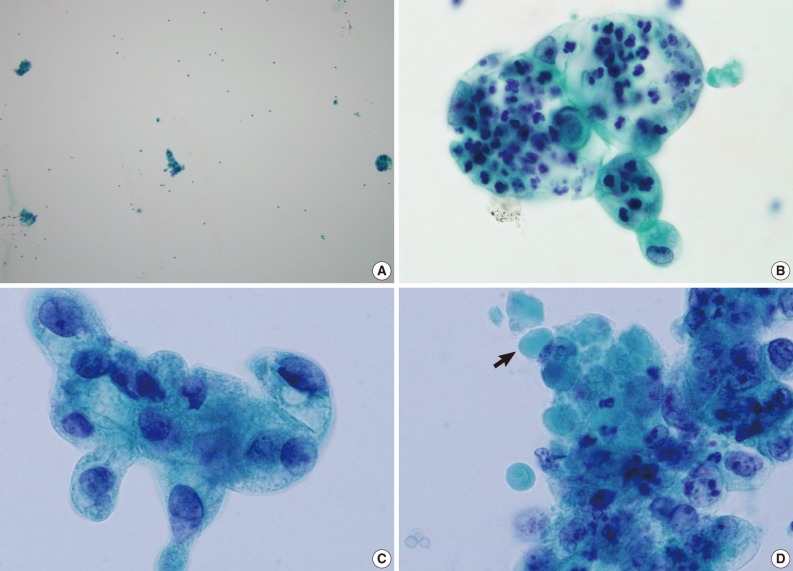
The voided urine cytology. (A) There are small clusters of globular or papillary tumor cells in the inflammatory background. (B) The necrotic debris and inflammatory cells are present within the cluster of tumor cells. (C) The tumor cells show an abundant, clear or granular cytoplasm with clear vacuoles as well as large irregular nuclei with vesicular chromatin pattern and prominent nucleoli. Some clusters show cells with hobnail features. (D) Small globular hyaline bodies (arrow) are present in the cluster of tumor cells.
Histological findings
A histological section showed a tubulo-papillary pattern with solid portions (Fig. 3A). The cells had an abundant clear or granular cytoplasm. The cells were cuboidal or columnar and hobnail cells were often present. The nucleus was vesicular with prominent nucleoli. Nuclear pleomorphism ranged from moderate to severe (Fig. 3B). Several eosinophilic, round hyaline bodies were scattered in the tumor (Fig. 3B). These histological findings were identical to those of the CCA of the female genital tract. The tumor cells were positive for cytokeratin (CK) 7 and P504S but negative for CK 20, p63 and prostatic-specific antigen (PSA) (Fig. 4).
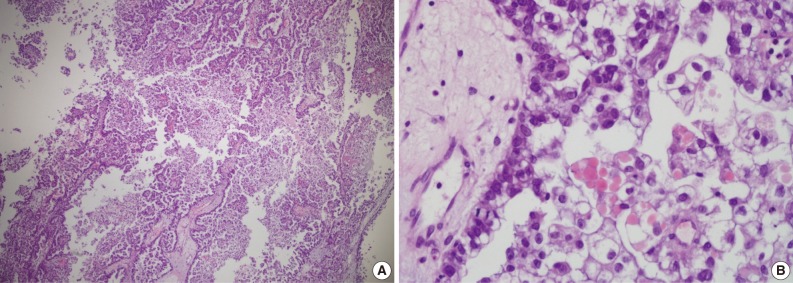
Histological findings. (A) A histological section shows a tubulo-papillary pattern with solid portions. (B) The tumor cells have an abundant, clear or granular cytoplasm with eosinophilic hyaline globules.
DISCUSSION
The CCA of the urethra is a rare disease entity and it accounts for approximately 1% of total cases of male urethral cancers and 15% of those of female urethral cancers.1 Some collective reviews and case reports attempt to describe the CCA. In the English literature, however, there are few articles about its cytological findings.6,7 Here, we reported a case of CCA of the urethra whose cytological and histological findings were identical to those of CCA of the female genital tract. The CCA cytology of female genital tract showed a clear or necrotic background, papillary and cystic patterns, anisonucleosis, distinct nucleoli, abundant and clear cytoplasm, and cells with a hobnail pattern.8 According to previous reports about the cytology of CCA of urethra and urinary bladder,7 the cytological key features include enlarged tumor cells with an abundant, clear cytoplasm with distinct vacuoles, hobnail and signet ring cells, and prominent nucleoli. In addition, scattered hyaline globules were found in the tumor cell nests of the current case. This finding has not been described in previous reports. The hyaline globules are distinct features of the CCA, which can be useful in ruling out other malignancies such as conventional adenocarcinoma or high-grade urothelial carcinoma on urine cytology.
Cytological differential diagnoses of the CCA of the urinary tract include high-grade urothelial carcinoma with glandular differentiation, conventional adenocarcinoma and nephrogenic adenoma. The conventional high-grade urothelial carcinoma shows a high nuclear-cytoplasmic ratio with hyperchromatic irregular nuclei. In most cases of high-grade urothelial carcinoma with glandular differentiation, the nucleoli are prominent, the glandular component shows globular shape or three dimensional ball structures and its cytoplasm has vacuoles. The metastatic or primary adenocarcinoma also reveals an abundant cytoplasm with vacuoles. It has an enlarged, hyperchromatic nucleus or vesicular chromatin pattern with prominent nucleoli. These findings are similar to CCA. In the conventional adenocarcinoma or high grade urothelial carcinoma with glandular differentiation, however, hobnail cells, hyaline globules and inflammatory cells in the tumor nests are not usually observed. On cytologic findings of nephrogenic adenoma, the cells are shed singly or in papillary cell clusters in the inflammatory background. The tumor cells can have enlarged vacuolated cytoplasm as in CCA. In contrast to the CCA, however, cytoplasmic vacuoles do not indent the nuclei, the nuclei show fine granular chromatin patterns and nuclear atypia is mild or absent. The nuclei are eccentrically located with a regular nuclear membrane.9
The histogenesis of CCA of the lower urinary tract is still controversial. In the past, it has been hypothesized to be of a mesonephric or Müllerian origin. Drew et al.2 reported that the tumor cells were positive for cancer antigen 125, a marker of Müllerian differentiation, and showed morphological similarities to the CCA of the female genital tract. In addition, it has also been hypothesized to be of a periurethral duct origin. One study suggested that CCA originated from the Skene's ducts because the tumor cells were positive for PSA.3 In the current case, however, the tumor cells were negative for PSA. Even in cases of PSA negative-CCA, however, it is still assumed to originate from the Skene's gland because the tumor mucin (salivary gland type) and its immunohistochemical findings are identical to those of the Skene's gland.4 Furthermore, it has also been hypothesized to be of a urothelial origin. Considering the fact of focal presence of conventional urothelial carcinomas in some cases, and occasional occurrences in male patients, and with some similarity of immnunohistochemical profiles and chromosomal changes, one can assume that urothelial origin might be another possibilityle.10 However, the tumor cells of CCA are commonly negative for CK 20 and p63, which is uncommon in cases of high-grade urothelial carcinomas. In addition, other study showed that CCAs were positive for P504S but negative for p63 and these findings are not compatible with urothelial origin tumors.5 P504S is also called α-methylacyl-CoA racemase, an enzyme involved in β-oxidation of branched-chain fatty acids in the mitochondria and peroxisomes. It is also expressed in some tumors and these include prostatic adenocarcinoma, colorectal adenocarcinoma, papillary renal cell carcinoma, and nephrogenic adenoma. In the current case, the tumor cells were also negative for CK 20 and p63 but positive for P504S. It is hypothesized that the CCA might also originate from the nephrogenic adenoma or metaplasia. Nephrogenic adenoma shows histologic and immunohostochemical resemblances those being P504S positive and p63 negative. It has also been reported that there were identical genetic changes between nephrogenic adenoma and CCA.11
The CCA has a stage-dependent prognosis. A deeply invasive tumor is highly aggressive and a non-invasive tumor can have a good prognosis.
In conclusion, the CCA showed cytologic distinctive features including enlarged tumor cells with an abundant, clear cytoplasm with distinct vacuoles, cells with hobnail pattern, prominent nucleoli and hyaline globules. Still, however, the histogenesis of CCA remains uncertain.
Acknowledgments
This study was granted by Inha University Research Grant.
Notes
No potential conflict of interest relevant to this article was reported.
