Inflammatory Pseudotumor-like Follicular Dendritic Cell Tumor of the Spleen with Extensive Histiocytic Granulomas and Necrosis: A Case Report and Literature Review
Article information
Inflammatory pseudotumor (IPT)-like follicular dendritic cell tumor (FDCT) has been recently designated1 and characterized by proliferation of Epstein-Barr virus (EBV)-positive follicular dendritic cell (FDC) and commonly occurs in the liver and spleen.2-9 Histologically, it is characterized by spindle cell proliferation admixed with abundant inflammatory cells, mainly lymphocytes and plasma cells. At present, the preferred term 'inflammatory myofibroblastic tumor' is used, because it has been shown that the proliferating spindle cells show a myofibroblastic phenotype in many cases.1 About 20 cases have been reported,2,9 although only one case has been reported in Korea.9 We present here a rare case of IPT-like FDCT of the spleen with extensive histiocytic granulomas and necrosis, including a brief literature review.
CASE REPORT
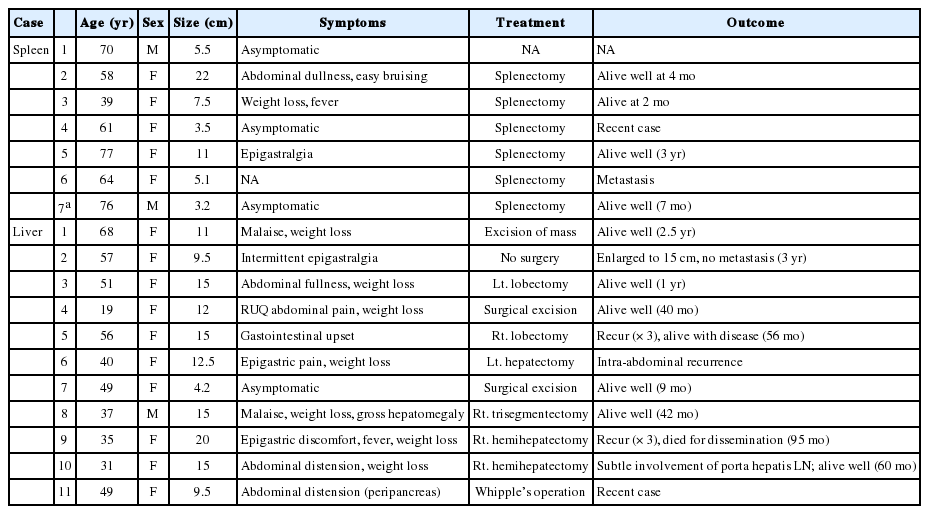
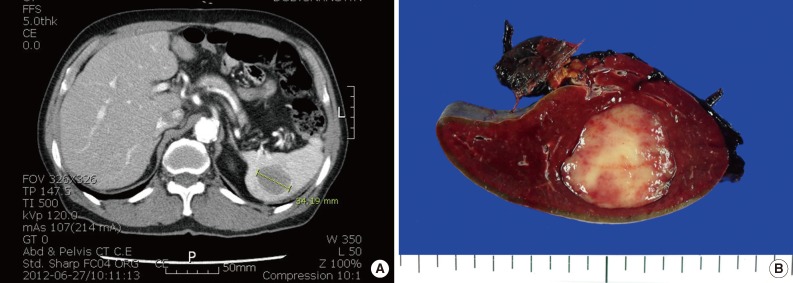
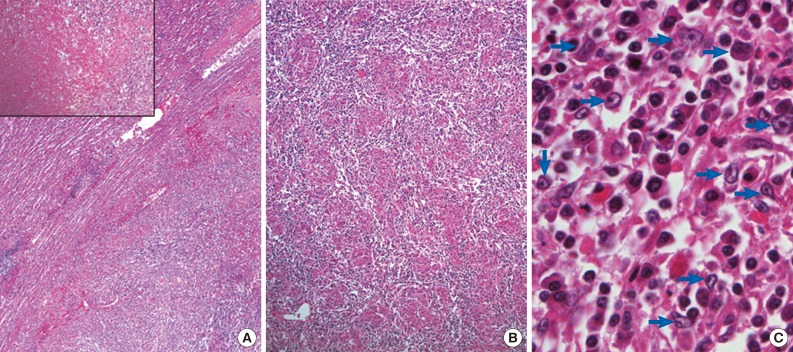
A 76-year-old man underwent abdominal-pelvic computed tomography for follow-up of previous gastric cancer (disease-free state for five years after radical subtotal gastrectomy). A newly developed splenic mass had been increasing in size for the previous six months (1.9 to 3.4 cm) (Fig. 1A). There was no evidence of local recurrence or metastasis, even on positron emission tomography-computed tomography. A splenectomy was performed. A well-defined gray-whitish firm nodule (3.2 cm in greatest dimension) was detected (Fig. 1B). Microscopically, the well-defined lesion was composed of an admixture of inflammatory cells and spindle cells in a background of numerous histiocytic granulomas and central coagulative necrosis (Fig. 2A, B). The oval to spindle cells had pale or eosinophilic cytoplasms with indistinct cell borders. The nuclei were enlarged and twisted or irregularly folded. Small but distinct, centrally located nucleoli were often evident (Fig. 2C). Mitotic figures were not found. The infiltrating reactive inflammatory cells were predominantly composed of lymphocytes, plasma cells, and a small number of eosinophils. The immunohistochemical results are as follows: CD35+ (Fig. 3A), CD21-, smooth muscle actin (SMA)-, and anaplastic lymphoma kinase- in oval to spindle cells, mixed imfiltration of CD3+ and CD20+ lymphocytes, and CD68+ in histiocytes (Fig. 3B). The Ki-67 labeling index was about 30% in spindle cells. EBV in situ hybridization (EBV-ISH) revealed diffuse and strong positivity in oval to spindle cells (Fig. 3C). Special stains for bacteria, acid-fast bacilli and fungi showed no organisms.
Gross finding. (A) Abdominal-pelvic computed tomography (CT) shows a newly developed spelnic mass in a normal-sized spleen (3.4 cm), increasing in size over six months. (B) The mass is a 3.2 cm-sized, well circumscribed, gray-whitish to tan, firm nodule.
Microscopic findings. (A) A well-defined mass is composed of spindle cells admixed with chronic inflammatory cells with a central coagulative necrosis (inset). (B) Many histiocytic granulomas can be identified in the background. (C) The oval to spindle tumor cells (blue arrows) have enlarged twisted/folded nuclei and distinct nucleoli.
The immunohistochemical staining of the tumor cells is positive for CD35 (A), and negative for histiocytes. (B) The histocytic granuloma is composed of CD68-positive cells. (C) Epstein-Barr virus in situ hybridization is detected almost exclusively in spindle tumor cells (inset; high power view), not in histiocytes.
DISCUSSION
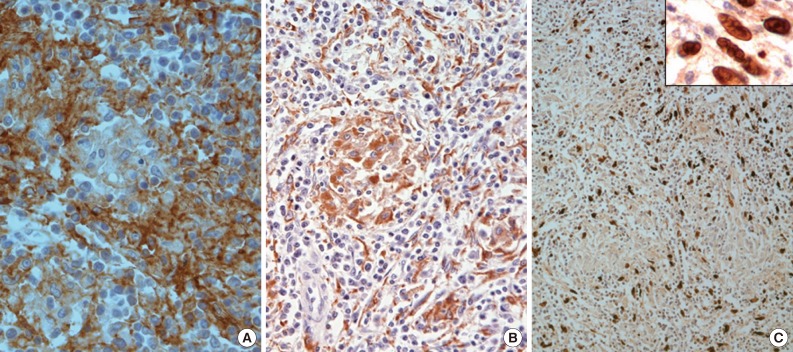
An IPT-like FDCT is extremely rare, and the pathogenesis and clinicopathologic characteristics are not clearly defined. The reviewed papers revealed seven cases in the spleen, ten cases in the liver, and one case in the peripancreas. The range of age was variable, from 19 to 77 years. The tumor size ranged from 3.5 to 22 cm. The clinical outcome was relatively fair, but three casesd disclose several recurrences and one case showed metastasis.2,9 The reported cases are summarized in the Table 1.
The collective immunohistochemical results9 of IPT-like FDCTs are as follows: CD21/CD35-positive in spindle cells (80%), 46.2% for CD23, 16.7% for SMA and 100% for EBV-ISH, which demonstrate that the first lines of investigation for IPT-like FDCT are FDC markers and EBV-ISH. In the present case, the tumor cells were highlighted at EBV-ISH.
The main pathogenesis of IPT-like FDCT has been hypothesized to occur through hepatic and splenic IPT-like tumors arising from a common mesenchymal cell, but using one of three different pathways; mostly myofibroblastic (SMA+), with a minor fraction via FDC lineage (CD21+, CD35+, and CD23+) or histiocyte (CD68+). CD21 expressed in FDC is a well-known EBV receptor, functionally active EBV-transformed FDC cell lines have been successfully established, and clonal EBV infection in some IPT-like FDCTs has been demonstrated. Based on these findings, it has been suggested that EBV might be involved in the pathogenesis of IPT-like FDCTs.9
A histiocytic granuloma is a unique feature of this case, which does not seem to be a well-formed granuloma, but plump histiocytic aggregates with multinucleated giant cells. No infectious organism was detected.
Coagulative necrosis was evident at the central portion of tumor, which may have been related with relatively rapid growth rate in a short time period. This finding has not been described yet.
In summary, we present a case of IPT-like FDCT in the spleen of a patient with a history of gastric carcinoma. This tumor showed distinct histologic features with extensive histocytic granulomas in a mixed inflammatory background.
Notes
This case was presented at 64th fall meeting of Korean Society of Pathologist (E-poster and poster exhibition Abstract #121).
No potential conflict of interest relevant to this article was reported.