Evaluation of Pathologic Complete Response in Breast Cancer Patients Treated with Neoadjuvant Chemotherapy: Experience in a Single Institution over a 10-Year Period
Article information
Abstract
Background
Pathologic complete response (pCR) after neoadjuvant chemotherapy (NAC) has been associated with favorable clinical outcome in breast cancer patients. However, the possibility that the prognostic significance of pCR differs among various definitions has not been established.
Methods
We retrospectively evaluated the pathologic response after NAC in 353 breast cancer patients and compared the prognoses after applying the following different definitions of pCR: ypT0/is, ypT0, ypT0/is ypN0, and ypT0 ypN0.
Results
pCR was significantly associated with improved distant disease-free survival (DDFS) regardless of the definition (ypT0/is, p = .002; ypT0, p = .008; ypT0/is ypN0, p < .001; ypT0 ypN0, p = .003). Presence of tumor deposits of any size in the lymph nodes (LNs; ypN ≥ 0(i+)) was associated with worse DDFS (ypT0 ypN0 vs ypT0 ypN ≥ 0(i+), p = .036 and ypT0/is ypN0 vs ypT0/is ypN ≥ 0(i+), p = .015), and presence of isolated tumor cells was associated with decreased overall survival (OS; ypT0/is ypN0 vs ypT0/is ypN0(i+), p = .013). Residual ductal carcinoma in situ regardless of LN status showed no significant difference in DDFS or OS (DDFS: ypT0 vs ypTis, p = .373 and ypT0 ypN0 vs ypTis ypN0, p = .462; OS: ypT0 vs ypTis, p = .441 and ypT0 ypN0 vs ypTis ypN0, p = .758). In subsequent analysis using ypT0/is ypN0, pCR was associated with improved DDFS and OS in triple-negative tumors (p < .001 and p = .003, respectively).
Conclusions
Based on our study results, the prognosis and rate of pCR differ according to the definition of pCR and ypT0/is ypN0 might be considered a more preferable definition of pCR.
Neoadjuvant chemotherapy (NAC) is used as a standard therapy for inflammatory and inoperable locally advanced breast cancers [1]. NAC may shrink the extent of the tumor and provide prognostic information to test treatment response [2]. Pathologic complete response (pCR) after NAC is associated with improved prognosis in breast cancer and therefore is used as a surrogate of clinical outcome [3]; however, the definitions of pCR have not been standardized, rendering interpretation of NAC data challenging [3-5].
Differences among definitions of pCR are based on the inclusion of lymph node (LN) status and ductal carcinoma in situ (DCIS). The NSABP B-18 trials showed that patients with ypT0/is had a better 5-year disease-free survival than patients with residual invasive disease in the breast [6,7], and several subsequent trials employed ypT0/is as the primary endpoint [8-11]. However, several studies showed that residual tumors in LNs implied worse prognosis regardless of residual tumors in the breast [3,12-15]. Isolated tumor cells (ITCs) in LNs after NAC are designated as non-pCR by the American Joint Committe on Cancer TNM [16]; however, sufficient evidence is lacking to support this recommendation. Including residual DCIS in pCR is another controversial issue regarding the definition of pCR [3,17]. The pooled analysis of 12 neoadjuvant randomized trials by the Collaborative Trials in Neoadjuvant Breast Cancer (CTNeoBC) showed that event-free survival and overall survival (OS) of patients with no tumor cells in the breast (ypT0 ypN0) were comparable to those of patients with residual DCIS (ypT0/is ypN0) [12]. Conversly, in the trials by the German Breast Group and Arbeits gemeinschaft Gynäkologische Onkologie-Breast Group (GBG and AGO-B), patients with ypTis ypN0 had a worse event-free survival than patients with ypT0 ypN0 [3]. However, the analysis conducted at MD Anderson Cancer Center showed no difference in survival between patients with ypT0 ypTN0 and ypTis ypTN0 [17].
Therefore, the previously proposed definitions of pCR can be divided into two main categories, assessment of pathologic response after NAC in the breast only or in both the breast and LNs. For example, the NSABP-B18 defined pCR as absence of residual invasive tumor cells in the breast (ypT0/is), and CTNeoBC and residual cancer burden proposed by the study conducted at MD Anderson Cancer Center defined pCR as no residual invasive tumor cells not only in the breast but also in the LNs (ypT0/is ypN0). In contrast, the Japanese Breast Cancer Society (JBCS) defined pCR as complete disappearance of tumor cells including DCIS in the breast (ypT0), and the GBG and AGO-B defined it as no residual tumor cells in the breast as well as in the LNs (ypT0 ypN0) [3,6,7,18,19].
Molecular intrinsic subtypes of breast cancer have important prognostic value [20]. Due to the infeasibility of this classification in routine practice, the simplified classification based on immunohistochemical (IHC) results of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) can be used to categorize substitutes, classifying ER/PR+HER2– as luminal A, ER/PR+HER2+as luminal B, ER/PR–HER2+as HER2-positive and ER/PR–HER2– as triple-negative (TN) tumors [21]. These IHC classifications also have prognostic value similar to those of molecular intrinsic subtypes [22]. Thus, assessment of pCR according to subtype might provide additional prognostic information.
Different definitions of pCR can result in different prognosis. Defining the criteria of pCR that better predict clinical outcome would be important. Therefore, in this study, the prognostic significance of different definitions of pCR were compared and the prognostic significance of LN status, ITCs in the LN, residual DCIS and subtypes were further investigated.
MATERIALS AND METHODS
Study population
We retrospectively retrieved data from 353 individual patients from electronic medical records of Samsung Medical Center in Seoul, Korea, from January 2004 to December 2013. Patients treated with anthracycline and taxane-based NAC and who subsequently underwent surgery with curative intent for primary breast cancer were included. Patients who had histologically confirmed distant metastasis at the time of diagnosis and who were diagnosed with inflammatory carcinoma were excluded. This study was approved by the Institutional Review Board of Samsung Medical Center, and the requirement for informed consent was waived.
Baseline studies including clinical examination, mammography, ultrasound, and magnetic resonance imaging were performed to assess the extent of primary tumor in the breast and LNs. All patients were diagnosed with breast cancer based on core needle biopsies, and LN metastasis was confirmed using core needle biopsy or fine-needle aspiration. All patients were treated with four or six cycles of anthracycline and taxane-based regimen at 3-week intervals, including adriamycin with docetaxel, adriamycin with cyclophosphamide plus docetaxel (AC-T), or AC-T plus trastuzumab. Patients with hormonal receptor–positive tumors received adjuvant endocrine therapy for at least 5 years after surgery. Patients with HER2-overexpressing and/or amplified tumors received neoadjuvant trastuzumab plus chemotherapy followed by adjuvant trastuzumab. Local and regional recurrence was confirmed either histologically or cytologically.
Histologic review
Core biopsies before NAC and surgical specimens obtained after NAC were reviewed. The largest size of tumors, histologic type, histologic grade, lymphovascular invasion (LVI), proportion of DCIS, number of positive LNs, size of the largest metastasis, and treatment response in breast and LN were evaluated. Tumor size and extent in breast and LNs were assessed according to the recommendation proposed by Provenzano et al. [23]. Histologic type was defined in accordance with the World Health Organization classification [24], and histologic grade was classified using the modified Scarff-Bloom-Richardson grading system [25].
To compare the prognostic impact of the pCR components defined previously, all patients were subdivided into the following subgroups according to TNM [16]: (1) no residual invasive tumor cells in the breast, ypT0/is, (2) no residual invasive tumor cells in the breast or LNs, ypT0/is ypN0, (3) no residual invasive tumor cells or DCIS in the breast, ypT0, and (4) no residual invasive tumor cells or DCIS in the breast and LNs, ypT0 ypN0.
ER, PR, and HER2 were assessed on both core biopsies and surgical specimens. ER and PR were considered positive only when greater than or equal to 1% of tumor cells showed nuclear staining. HER2 was positive if tumor cells showed 3+by IHC or 2+by IHC with amplification using silver in situ hybridization [26]. To assess the prognostic impact of pCR on intrinsic subtypes of breast cancer, all patients were classified into four subtypes according to the IHC results as follows: ER/PR+HER2- with histologic grade 1 or 2 tumors as luminal A-like; ER/PR+HER2– with histologic grade 3 tumors or ER/PR/HER2+ tumors as luminal B–like; ER/PR–HER2+tumors as HER2-positive; and ER/PR/HER2– tumors as TN [3,27].
Statistical analysis
Distant disease-free survival (DDFS) and OS were defined as the time between the date of initial diagnosis to the date of distant recurrence or the date of death from any cause, respectively. The significance of differences in baseline variables was analyzed using two-sided χ2, Fisher exact or Mann-Whitney U test as appropriate. DDFS and OS were plotted using the Kaplan-Meier product-limit method, and the log-lank p-value was calculated. To assess the prognostic impact of the pCR component, hazard ratios (HRs), 95% confidence intervals and p-value were calculated using Cox proportional hazards model. All tests were two sided, and a p-value less than .05 was considered statistically significant. Statistical analyses were performed using the SPSS statistical software ver. 20.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Patient characteristics
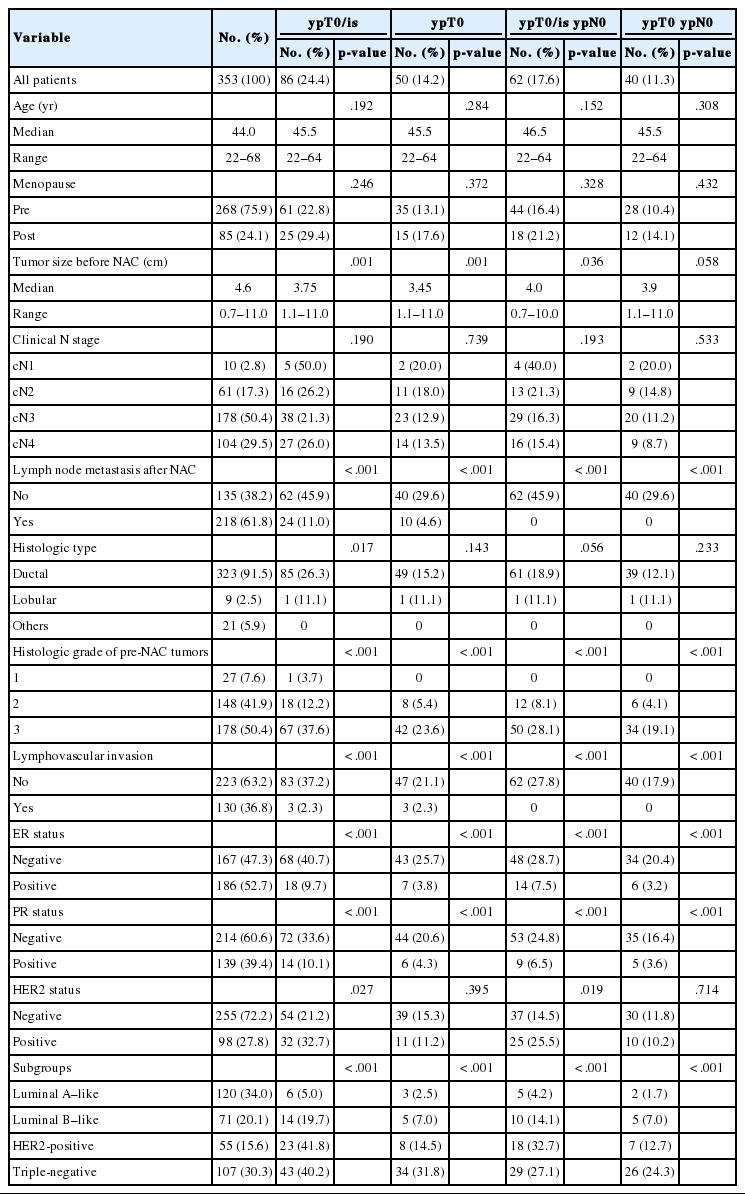
Median age at diagnosis was 44.0 years (range, 22 to 68 years). Median size of tumor was 4.6 cm (range, 0.7 to 11.0 cm) before NAC and 1.5 cm (range, 0.0 to 13.0 cm) after NAC. Most patients (282/353, 79.9%) had cN2 or N3 nodal status before NAC, and median number of positive LNs after NAC was 1 (range, 0 to 39). Baseline clinicopathologic characteristics and corresponding pCR rates according to definition of pCR are summarized in Table 1. In brief, histologic grade, LVI, presence of metastatic LN, and hormonal receptor status showed significant correlation with pCR rate according to definition. Patients with high histologic grade tumors, no LVI, no metastatic LN, and negative hormonal receptor status tended to have higher pCR rates. HER2-positive and TN tumors showed significantly higher pCR rates than luminal A-like and luminal B-like tumors regardless of the pCR definition. The median follow-up time of 353 patients was 36.5 months (range, 0.4 to 129.0 months). During this period, 101 patients (28.6%) had a relapse and 41 (11.6%) died. The 5-year DDFS was 68.0%, and OS was 84.8%.
Correlation between pCR and survival according to definition
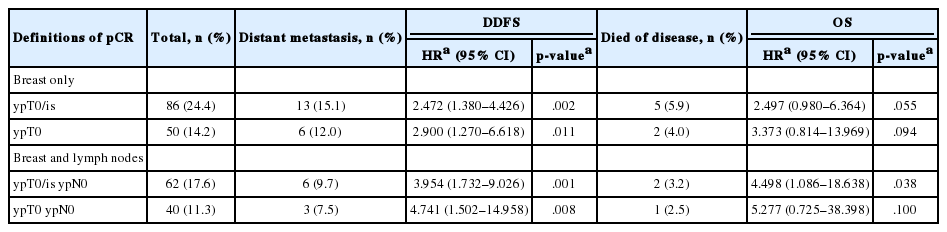
According to the four definitions of pCR, 86 (24.4%) patients were diagnosed as ypT0/is, 50 (14.2%) as ypT0, 62 (17.6%) as ypT0/is ypN0, and 40 (11.3%) as ypT0 ypN0. Patients who achieved pCR showed significantly better DDFS than patients who did not (Fig. 1A, C, E, G). Similarly, patients who achieved pCR also tended to have better OS than patients who did not, but this difference was not statistically significant when ypT0 and ypT0 ypN0 were used as the pCR definitions (Fig. 1B, D, F, H). HRs for DDFS and OS increased sequentially as follows: ypT0/is, ypT0, ypT0/is ypN0, and ypT0 ypN0 (Table 2).
Survival analysis according to definition of pCR. DDFS and OS according to ypT0/is definition of pCR (A, B), ypT0 (C, D), ypT0/is ypN0 (E, F), and ypT0 ypN0 (G, H). pCR, pathologic complete response; DDFS, distant disease-free survival; OS, overall survival.
Prognostic significance of LN status
In the ypT0 subgroup (n=50), 10 patients (20.0%) had tumor deposits in the LNs (ypN≥0(i+)) and experienced worse DDFS than patients with no metastatic LNs (5-year DDFS: ypT0 ypN0, 92.1%; ypT0 ypN≥0(i+), 68.6%; p=.036). In the ypT0/is subgroup (n=86), 24 patients (27.9%) had residual tumor deposits in the LNs (ypN≥0(i+)) and experienced worse DDFS than patients with no metastatic LNs (5-year DDFS: ypT0/is ypN0, 89.0%; ypT0/is ypN≥0(i+), 70.2%; p =.015). The 5-year OS for patients with ypT0 ypN≥0(i+) and ypT0/is ypN≥0(i+) (88.9% and 86.5%, respectively) appeared worse than for patients with ypT0 ypN0 and ypT0/is ypN0 (97.4% and 93.2%, respectively), but the difference was not statistically significant (p=.236 and p=.095, respectively).
Prognostic significance of ITCs in the LNs
Among patients with ypT0 ypN≥0(i+) (n=10), 3 had ITCs in the LNs, and none relapsed or died. Among patients with ypT0/is ypN≥ 0(i+) (n=24), five had ITCs in the LNs, and showed worse OS compared to patients with ypT0/is ypN0 (5-year OS: ypT0/is ypN0(i+), 75.0% vs ypT0/is ypN0, 93.2%; p=.013). For DDFS, patients with ITCs in LNs tended to experience worse DDFS than patients with no tumor cells in the LNs (5-year DDFS: ypT0/is ypN0(i+), 80.0% vs ypT0/is ypN0, 89.0%; p=.336).
Prognostic significance of residual DCIS
Patients with residual DCIS in the breast tended to experience worse DDFS and OS compared with patients with no residual tumor cells in the breast (5-year DDFS: ypT0, 87.6% and ypTis, 78.3%; 5-year OS: ypT0, 95.8% and ypTis, 85.5%), but the difference was not statistically significant (p=.373 and p=.441, respectively). Considering LN status, patients with ypT0 ypN0 had 5-year DDFS of 92.1% and OS of 97.4%, which appeared better than those of patients with ypTis ypN0 (5-year DDFS, 83.3% and 5-year OS, 87.5%). However, these were not statistically significant (p=.462 and p=.758, respectively).
Among patients who achieved pCR when ypT0/is was used as the definition of pCR, the proportion of patients with residual DCIS was significantly different among IHC subtypes (p=.001); highest with HER2-positive tumors (15/23, 65.2%) followed by luminal B-like (9/14, 64.3%), luminal A-like (3/6, 50%), and lowest with TN tumors (9/43, 20.9%).
Prognostic significance of pCR in IHC subtypes
To analyze the prognosis between patients with or without pCR according to IHC subtype, we defined pCR as ypT0/is ypN0 according to our study results. In TN tumors, pCR was significantly associated with improved survival in terms of both DDFS and OS. However, in luminal A-like, luminal B-like, and HER2-positive tumors, pCR showed no prognostic impact on survival (Fig. 2). In patients without pCR, HER2-positive and TN tumors showed poorer prognosis than in luminal A-like and luminal B-like tumors (Fig. 2).
(A-H) Prognosis between patients with or without pCR according to intrinsic subtype. pCR, pathologic complete response; Luminal A-like, ER/PR+HER2– tumors with histologic grade 1 or 2; Luminal B-like, ER/PR+HER2– tumors with histologic grade 3 or ER/PR+HER2+ tumors; HER2-positive, ER/PR–HER2+ tumors; Triple-negative, ER/PR/HER2– tumors; ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor 2.
DISCUSSION
To the best of our knowledge, this study is the first analysis of the prognostic significance of different pCR definitions on long-term outcome in breast cancer patients treated homogeneously with anthracycline and taxane-based NAC regimens as well as neoadjuvant trastzumab plus chemotherapy at a single institute in Korea. We compared the following four definitions of pCR; ypT0/is, ypT0, ypT0/is ypN0, and ypT0 ypN0, and the corresponding pCR rates were 24.4%, 14.2%, 17.6%, and 11.3%, respectively (Table 1). These rates were similar to previous studies. In a study by JBCS (n=353), pCR rates of ypT0/is, ypT0, ypT0/is ypN0, and ypT0 ypN0 were 20.4%, 9.9%, 18.4%, and 8.2%, respectively [28]. In a meta-analysis by CTNeoBC (n=13,125), pCR rates of ypT0/is, ypT0/is ypN0, and ypT0 ypN0 were 22%, 18%, and 13%, respectively [12]. In the study by GBG and AGO-B (n=6,377), pCR rates of ypT0/is, ypT0/is ypN0, and ypT0 ypN0 were 22.8%, 19.8%, and 15.0%, respectively [3].
In the present study, patients with pCR, regardless of definition, had significantly better DDFS than patients without pCR. Regarding OS, however, patients with pCR when ypT0/is and ypT0/is ypN0 were used as pCR definitions showed significantly better survival than patients without pCR (Fig. 1). Regarding LN status, even if tumor cells were not present in the breast including DCIS, patients with residual tumor cells of any size in the LNs experienced worse DDFS than patients with no metastatic LNs. Presence of ITCs in the LNs after NAC is regarded as non-pCR by the American Joint Committee on Cancer for TNM staging [16]; however, data supporting this recommendation is insufficient. Our study showed that patients with ITCs in the LNs might have poorer OS than patients with no tumor cells in the LNs. However, further studies with larger populations are warranted.
Theoretically, ypT0 ypN0 represents the strictest definition of pCR, meaning complete eradication of all tumor cells in both the breast and LNs. Thus, we compared the prognosis between ypT0 and ypTis as well as between ypT0 ypN0 and ypT0/is ypN0 and found that presence of DCIS did not result in any difference. Thus, based on the results from this study, we considered ypT0/is ypN0 the more preferable definition of pCR. These results were consistent with previous studies by JBCS, CTNeoBC, and MD Anderson [12,17,28]. But not with those of GBG and AGO-B, which suggested ypT0 ypN0 as the best definition of pCR [3]. This discrepancy might be caused by the smaller number of patients and events in ypTis (n=36) and ypTis ypN0 (n=22), resulting in a much lower statistical significance to show prognostic differences in this study.
Among the IHC subtypes, HER2-positive and TN tumors achieved high pCR rates. pCR was significantly correlated with DDFS and OS only in TN tumors (Fig. 2). However, in patients without pCR, HER2-positive and TN tumors showed poorer prognosis than in luminal A-like and luminal B-like tumors. These results are in agreement with the previously reported studies by Liedtke et al. [29] and Houssami et al. [30].
The potential limitations of this study are as follows. First, due to the small number of patients and events, comparison between patients with pCR and without pCR using Cox proportional hazards model was not feasible. Second, because Ki-67 was not available for all patients, subtypes based on only ER, PR, and HER2 status and histologic grade might not be the same as molecular intrinsic subtypes.
In conclusion, the prognosis and rate of pCR varied according to definition of pCR. In our study, pCR defined as ypT0/is ypN0 was considered the most preferable. pCR could be used as a surrogate of favorable clinical outcome in TN tumors but not in luminal A-like, luminal B-like, or HER2-positive tumors.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.