Multiple hepatocyte nuclear factor 1A (HNF1A)-inactivated hepatocellular adenomas arising in a background of congenital hepatic fibrosis
Article information
Hepatocellular adenomas (HCAs) are benign hepatocellular neoplasms with distinct molecular subtypes [1,2]. Hepatocyte nuclear factor 1A (HNF1A)–inactivated hepatocellular adenoma (H-HCA) occupies about 35% of all HCAs [1,2]. H-HCA demonstrates somatic (90%) or germline (10%) inactivating mutations of HNF1A gene, which encodes a transcription factor involved in several metabolic pathways of hepatocytes, and inactivation of HNF1A promotes lipogenesis [3]. Clinically, H-HCAs occur predominantly in females, are frequently associated with oral contraceptives, and a subset of H-HCA with germline HNF1A mutations is associated with maturity-onset diabetes type 3 (MODY3). Morphologically, H-HCAs frequently show steatosis and loss of liver fatty acid-binding protein (LFABP) expression in the tumor cells [1,2].
Here, we report a rare case of a young male patient with multiple H-HCAs in a background of congenital hepatic fibrosis (CHF).
CASE REPORT
A 25-year-old man was admitted to the hospital for liver transplantation for multiple hepatic masses that were incidentally discovered by imaging. He had previously been diagnosed with CHF on liver biopsy 14 years ago, and had received transjugular intrahepatic portosystemic shunt for portal hypertension at that time. He had no history of metabolic syndrome, alcohol intake or prior intake of androgens and his body mass index was 25.2 kg/m2. There was no evidence of other abnormalities associated with CHF, and there was no remarkable family history. Preoperative liver function tests were as follows: aspartate aminotransferase 35 U/L, alanine aminotransferase 29 U/L, gamma-glutamyl transferase 19 U/L, alkaline phosphatase 79 U/L, total bilirubin 4.2 mg/dL, and direct bilirubin 1.3 mg/dL. Serological tests for hepatitis B and C virus were negative. On computed tomography, there were multiple fat-containing nodules in both hepatic lobes.
The liver weighed 1,242 g, and sections revealed nine discrete tan-to-yellow nodules in both lobes, measuring 9.5 × 6.5 × 7.5 cm in the largest one. The background liver was firm with a reticular appearance (Fig. 1). On microscopic examination, the background liver showed the typical histological features of CHF: broad fibrous bands rimmed by small bile ductular structures with ductal plate malformation patterns (Fig. 1). The pathological findings of the nine nodules are summarized in Table 1 and Figs. 2 and 3. Six nodules were diagnosed as H-HCAs and the three smaller nodules as large regenerative nodule (LRN) or focal nodular hyperplasia (FNH)-like nodules, based on the histo-pathological and immunohistochemical characteristics. Notably, although LFABP loss was seen in all six H-HCAs, nodules #1, #2, and #9 showed only patchy mild steatosis, and nodules #1 and #2 also demonstrated focal peliosis and mild ductular reaction. The remaining 4 H-HCAs demonstrated diffuse steatosis. On follow-up, the patient is currently well without evidence of recurrence.
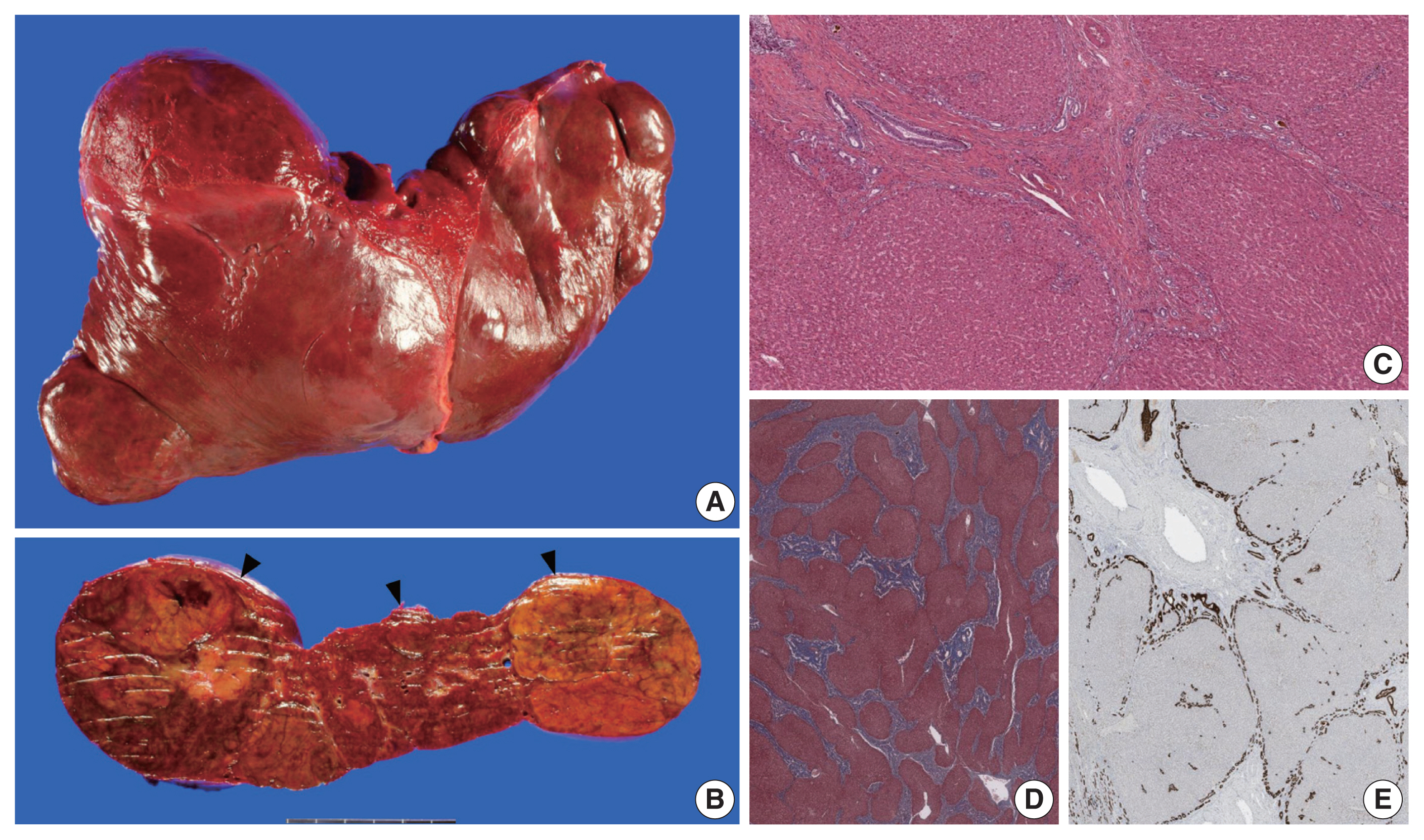
(A–C) Gross findings. (A) The explanted liver is distorted in shape due to the multiple bulging masses. (B) A representative section reveals three lobulated nodules (arrowheads). The nodules are lobulated, well-demarcated but non-encapsulated, with focal hemorrhage and peliosis. (C) On microscopy, the background liver shows broad fibrous bands lined by ductular structures with ductal plate malformation pattern and inspissated bile. (D) Masson’s trichrome stain reveals the jigsaw-puzzle pattern biliary fibrosis. (E) Cytokeratin 7 immunostain high-lights the ductular structures at the interface between the fibrous bands and the hepatic lobules.
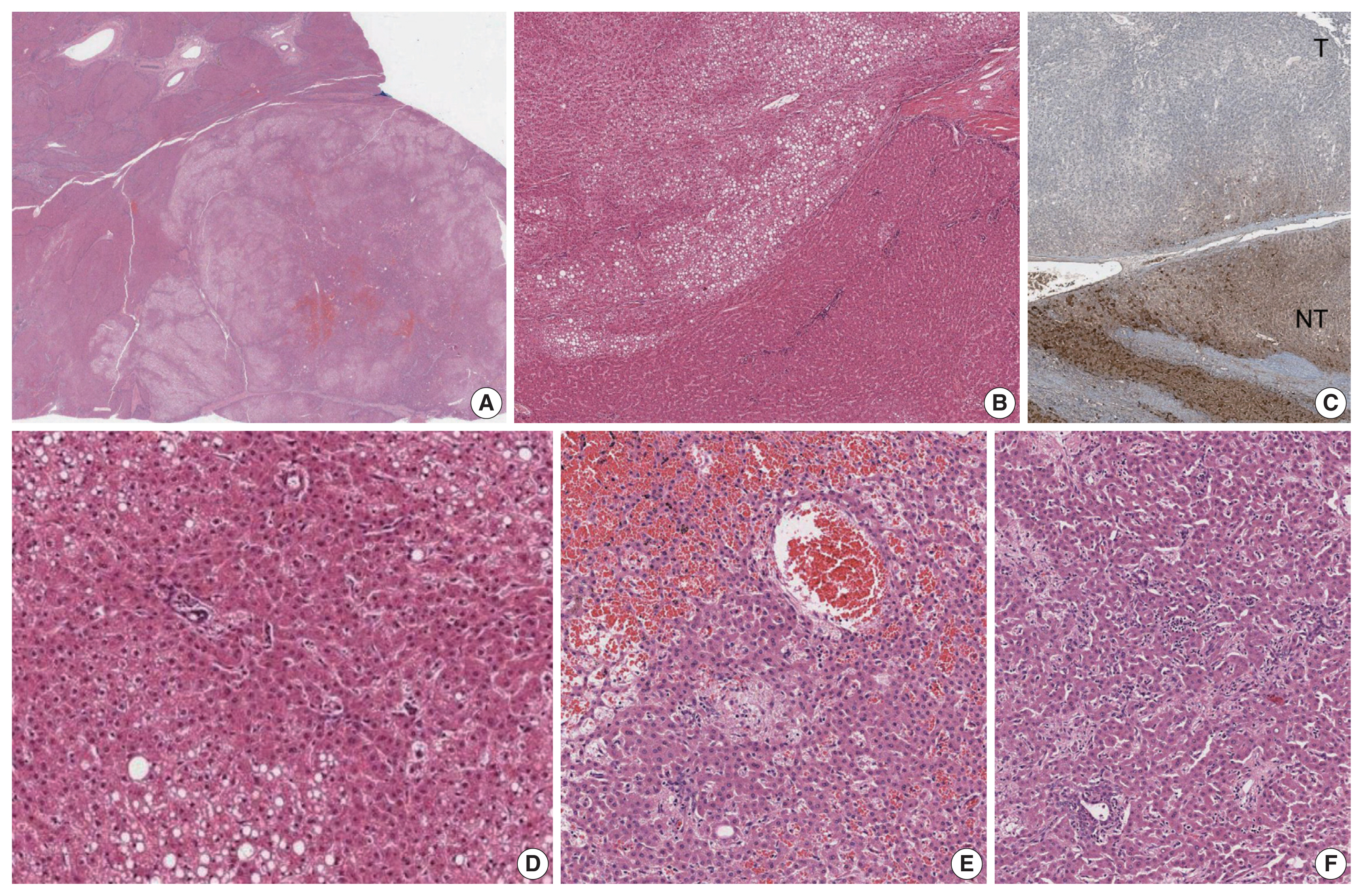
The histopathological and immunohistochemical features of this case. (A) Scanning power view demonstrates a well-demarcated and non-encapsulated solid mass (lower right). (B) The peripheral portion of the tumor shows patchy macrovesicular steatosis. (C) Loss of liver fatty acid-binding protein expression is seen in the tumor (T, tumor; NT, non-tumor). (D) Higher power magnification of the hepatocellular adenoma, demonstrating the patchy macrovesicular steatosis and unpaired arteries. (E) No significant cytoarchitectural atypia is present. The central portion of nodule #1 demonstrates focal sinusoidal dilatation with congestion and peliosis. (F) A few pseudoportal tracts are seen in nodule #1, containing clusters of bile ductules.

Smaller focal nodular hyperplasia-like nodules were seen (A–C) with small fibrous scars containing thick-walled blood vessels and patchy non-map-like glutamine synthetase expression. Fibrous septa were also seen in a large regenerative nodule but the central scar-like fibrous tissue was less prominent (D).
DISCUSSION
To our knowledge, this is the second reported case of H-HCA arising in a background of CHF. Hepatocellular nodules, including FNH and FNH-like nodules, HCAs and even hepatocellular carcinomas (HCCs), have been demonstrated to occur in the setting of hepatic vascular abnormalities, such as Budd-Chiari syndrome and congenital extrahepatic portosystemic shunts [4–8]. While CHF belongs to a group of fibropolycystic diseases of the liver that affects the biliary system, portal hypertension dominates the clinical presentation of this disease, as the number of portal vein branches is often reduced [9]. Treatment of CHF with portosystemic shunt surgery may also add to the abnormal heterogeneous vascularity in the parenchyme [10]. As a result, the uneven hepatic perfusion may give rise to the formation of hepatocellular nodules. However, although this vascular concept explains the pathogenesis of reactive hyperplastic hepatocellular nodules such as FNH and LRN/FNH-like nodules, the relationship between this vascular abnormality and the occurrence of neoplastic hepatocellular nodules is still not well understood. Indeed, the neoplastic nature of smaller hepatocellular nodules resembling HCAs (previously referred to as “adenoma-like” nodules or adenomatous hyperplasia) arising in vascular disorders have been questioned, due to the morphological overlap with LRNs and FNH-like nodules and their frequent co-existence within the same liver [4]. However, as the molecular classification of HCAs has been better characterized over the past decade, immunohistochemical stains have facilitated the diagnosis of HCAs [7]. Interestingly, Sempoux et al. [7] described three cases of H-HCAs arising in backgrounds of hepatic vascular disorders which were either associated with HCCs or contained atypical foci. This is a notable finding as it implies that H-HCAs associated with vascular disorders may be at increased risk of malignant transformation, in contrast to those arising in “conventional” settings (e.g., females, oral contraceptives, MODY3, etc) [2]. Another interesting finding is that H-HCAs in the context of hepatic vascular disorders often demonstrated a lack of intratumoral steatosis, which differs from the characteristic histology (diffuse steatosis) of typical H-HCAs [7]. Indeed, in our case, three H-HCAs demonstrated only focal mild steatosis, and the diagnosis was rendered based on the loss of LFABP expression.
Although further validation would be required, the identification of nodular lesions on imaging in the liver of patients with CHF or hepatic vascular disorders may warrant histological examination to rule out the possibility of HCCs or HCAs. In addition, H-HCAs arising in the context of hepatic vascular disorders may not be associated with the typical clinicopathological features, such as steatosis and low risk of malignant transformation.
Notes
Ethics Statement
This case study was approved by the Institutional Review Board of Seoul National University Hospital (#H-1809-141-975) and informed consent was waived.
Author Contributions
Conceptualization: YL (Yangkyu Lee), HK. Funding acquisition: HK. Investigation: YL (Yangkyu Lee), HK. Supervision: HK. Writing—original draft: YL (Yangkyu Lee). Writing—review & editing: YL (Yangkyu Lee), HP, KL, YL (Youngeun Lee), KL, HK. Approval of final manuscript: all authors.
Conflicts of Interest
H.K., a contributing editor of the Journal of Pathology and Translational Medicine, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding Statement
No funding to declare.

