Postmortem lung and heart examination of COVID-19 patients in a case series from Jordan
Article information
Abstract
Background
Coronavirus disease 2019 (COVID-19) has emerged as a pandemic for more than 2 years. Autopsy examination is an invaluable tool to understand the pathogenesis of emerging infections and their consequent mortalities. The aim of the current study was to present the lung and heart pathological findings of COVID-19–positive autopsies performed in Jordan.
Methods
The study involved medicolegal cases, where the cause of death was unclear and autopsy examination was mandated by law. We included the clinical and pathologic findings of routine gross and microscopic examination of cases that were positive for COVID-19 at time of death. Testing for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was confirmed through molecular detection by real-time polymerase chain reaction, serologic testing for IgM and electron microscope examination of lung samples.
Results
Seventeen autopsies were included, with male predominance (76.5%), Jordanians (70.6%), and 50 years as the mean age at time of death. Nine out of 16 cases (56.3%) had co-morbidities, with one case lacking such data. Histologic examination of lung tissue revealed diffuse alveolar damage in 13/17 cases (76.5%), and pulmonary microthrombi in 8/17 cases (47.1%). Microscopic cardiac findings were scarcely detected. Two patients died as a direct result of acute cardiac disease with limited pulmonary findings.
Conclusions
The detection of SARS-CoV-2 in postmortem examination can be an incidental or contributory finding which highlights the value of autopsy examination to determine the exact cause of death in controversial cases.
Since the declaration of coronavirus disease 2019 (COVID-19) as a pandemic, several parameters have been used to measure its public health impact [1]. These statistical measures include the rate of detected cases, rate of critical cases, and importantly the rate of death as a result of the disease [2]. The case fatality ratio (CFR) can be used to evaluate the severity among the detected cases; nevertheless, this parameter is prone to inherent bias in light of the following factors: (1) the guidelines for COVID-19 testing vary in different countries, with subsequent underestimation of true number of cases; (2) the postmortem detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) does not necessarily indicate its causal role in death which may cause an overestimation of the CFR; and (3) the time lags in handling and reporting of recovery and mortality from the disease which can lead to an under- or overestimation of the CFR [3-5].
Autopsy examination is the definitive method to establish the cause of death, particularly in the context of a novel infectious disease such as COVID-19 [6,7]. It can be chiefly beneficial to identify the causal relationship between death and infectious diseases in pandemic setting [8]. In addition, autopsy examination can provide important clues to understand the mechanisms of SARS-CoV-2–induced organ damage and its underlying mechanisms [9]. Forensic examination is a central step in a multidisciplinary approach to determine the cause of death in medicolegal cases positive for COVID-19 [10,11]. Thus, autopsy examination is invaluable in resolving disputes in medicolegal cases with legal liability of health professionals in the context of COVID-19–related deaths, especially in the hospitals and nursing homes [12,13]. The utility of autopsy examination has also been emphasized in cases of breakthrough infection post–COVID-19 vaccination [10]. In the absence of suitable precautionary measures, autopsy examination can be done using the minimally invasive approach, which can provide important clues to data on deaths attributed to COVID-19 [14].
More than 2 years have passed amid COVID-19 pandemic, and much has been known regarding its epidemiology, pathophysiology, and clinical manifestations [15]. Specifically, it is well-known now that there is a wide variability in clinical presentation of the disease with a majority of cases being asymptomatic or mild-to-moderate in clinically apparent infections [16]. Nevertheless, a substantial number of COVID-19 cases evolve into severe or critical disease with respiratory failure, septic shock, and/or multiple-organ failure and death from the disease [17,18].
Despite the rapid availability of extensive and comprehensive research on COVID-19, several aspects of the disease have not been fully elucidated yet, one of which is labeling the deaths with positive SARS-CoV-2 testing results as COVID-19–related mortalities despite the absence of typical findings of the disease [11,19,20]. Thus, autopsy examination can be the sole method to reach a definitive conclusion about the genuine cause of death in such a scenario [21].
In COVID-19, the causative agent is SARS-CoV-2, which utilizes angiotensin-converting enzyme 2 receptors to enter the target cells [22]. Although COVID-19 is primarily a respiratory disease, extrapulmonary manifestations including cardiovascular effects are commonplace especially in severe and critical cases [23]. Hypercoagulability state in association with COVID-19 has been observed frequently and could be linked to dual effect of direct virus damage and activation of various host inflammatory mediators [24]. Subsequently, the hypercoagulability can give rise to acute coronary syndrome (ACS) as a cardiac manifestation of the disease [25].
For the diagnosis of COVID-19, molecular detection by nucleic acid amplification testing including real-time polymerase chain reaction (qPCR) can be considered the gold standard laboratory diagnostic method [26]. Another diagnostic approach, which can be helpful in COVID-19 cases with late presentation include serologic testing for IgM antibodies [27]. The use of electron microscopy (EM) is considered a reliable tool to delineate the ultra-structural details of viruses, including SARS-CoV-2; however, its use in clinical practice has been limited by cost issues besides the need for technical expertise and tedious procedure compared to molecular detection techniques [28].
Histopathologic findings in autopsies from COVID-19–positive cases include the detection of diffuse alveolar damage (DAD) in a vast majority of cases [28,29], with frequent detection of microthrombi. The spectrum of findings ranges from alveolar hyaline membranes formation, interstitial edema, necrosis of type 1 pneumocytes and endothelial cells in the exudative phase to hyperplasia of type II pneumocytes, and interstitial myofibroblasts with lymphocytic infiltration in the organizing phase and eventually collagenous fibrosis and end-stage lung changes in the fibrotic phase [29]. Despite the view that COVID-19 pneumonia is a heterogeneous disease, from a histopathologic point of view, there is previous evidence that acute and organizing DAD can be considered the primary cause of mortality due to SARS-CoV-2 infection [29,30].
In spite of the growing number of case series describing the autopsy findings in COVID-19–positive deaths, there is a general lack of reports describing the pathophysiology and histopathologic examination of autopsies in the Middle East region to the best of our knowledge [6,7,31]. Thus, such an investigation can be considered necessary to supplement the previous literature with more insights that can be helpful to better define the histopathologic changes that occur in the context of COVID-19 and to establish the cause of death in cases with atypical presentation. Therefore, the current study aimed to evaluate the histopathologic findings in autopsies in a case series from individuals who were positive for COVID-19 at time of death in Jordan.
MATERIALS AND METHODS
Study design
The current study was based on conducting a serial postmortem examination in COVID-19–positive patients at time of death among medicolegal cases in which autopsies are mandatory by Jordanian law to determine the cause of death. Testing for SARS-CoV-2 for all cases of death was mandatory by law before burial in Jordan. Autopsies were conducted at Jordan University Hospital (JUH) and Zarqa Hospital. Forensic gross assessment was done for specimens from the lungs, heart, among other organs. Postmortem specimens were tested for SARS-CoV-2 by qPCR, serologic testing, or both. The final confirmation of SARS-CoV-2 detection in autopsies was done through examining lung specimens under EM, which was conducted at the Department of Pathology, Microbiology and Forensic Medicine at the School of Medicine, University of Jordan.
Testing for COVID-19
The postmortem detection of SARS-CoV-2 was based on three approaches as follows: (1) qPCR of nasopharyngeal swabs, with RNA purification using the automated Zybio Nucleic Acid Isolation System EXM3000 (Zybio, Chongqing, China), with reverse-transcriptase qPCR being done using SARS-CoV-2 Nucleic Acid Detection Kit (Zybio) targeting three genomic regions (Envelope, ORF1ab, and Nucleocapsid) with interpretation according to manufacturer’s instructions; (2) serologic testing to detect IgM/IgG; (3) EM examination of autopsies with lung tissue.
Initially, all cases were identified through either a positive qPCR testing result or serologic testing, while EM examination was conducted among all cases.
Autopsy examination
Autopsies carried out on COVID-19–positive dead bodies were done by authority of the District Attorney since all cases were labeled as medicolegal cases. Such cases are considered medicolegal due to the sudden and unexpected death with no clear causes, with consent to conduct autopsy examination being waived in such cases. Most included autopsies were limited to the chest and abdomen, but some cases were examined fully according to the circumstances of their death. Personal protective equipment was used among all staff members. The procedures involved the minimum needed number of staff. Full external inspection of the body as it was received was conducted initially, followed by midline chest and abdomen incision with extraction of the lungs and heart with full inspection and documentation by “inspection report and photographing of all positive findings.” Tissue sampling was limited to the lungs and heart.
Histopathologic examination
Tissue specimens were fixed in 10% formalin for 72 hours, dehydrated by ethanol, and cleared twice by xylene, then embedded in paraffin, and sectioned as 5 μm sections. The prepared sections were dried and stained by hematoxylin and eosin full final histopathologic examination, which was conducted by the first authors and the senior author (M.A. and M.A.A.-A.), who are consultant histopathologists at JUH.
The differentiation between “death from COVID-19” vs. “death with SARS-CoV-2 infection” was based on the presence of DAD in the former group in contrast to its total absence in the later group.
EM examination
The procedure of EM was adopted from a previous publication by Shatarat et al. [32]. Briefly, the extracted tissues from autopsies were fixed for one hour in buffered 1%–2% osmium tetroxide followed by gradual dehydration in ethanol/propylene oxide and embedding in epoxy resin media mixture. The U7 ultra-cut was used to obtain sections with a range of 70–90 nm, followed by mounting on 200 mesh copper grids, and contrasted with uranyl acetate and lead citrate [32]. The FEI Morgagni Transmission Electron Microscope was used for image acquisition and analysis.
Criteria for identification of “death from COVID-19” vs. “death with SARS-CoV-2 infection”
As previously stated, we used histopathologic findings as the sole criterion to define death from COVID-19 if DAD was found while its absence, was used to denote death with SARS-CoV-2 infection.
Statistical analysis
Based on the small sample size, two-sided Fisher exact test was used to investigate categorical variables, while assessment of the association between age as a continuous variable with dichotomous categorical variables was done using the Mann-Whitney U test. Statistical analysis was done using IBM SPSS Statistics for Windows ver. 22.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Characteristics of the included cases
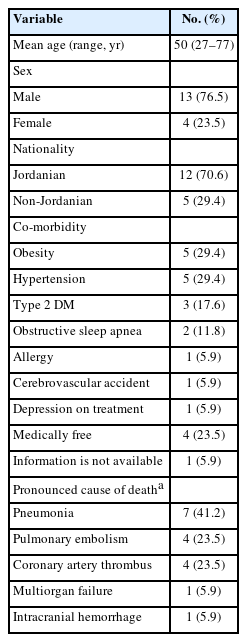
The study cohort comprised 17 individuals who were positive for COVID-19 at postmortem SARS-CoV-2 assessment by qPCR testing of nasopharyngeal swabs (n = 4), serologic testing for SARS-CoV-2 IgM (n=3) or confirmed by both methods (n=10). Two individuals were diagnosed with COVID-19 by qPCR several days prior to death (5 days and 12 days antemortem), whereas the remaining cases had positive test results within 24 hours from being declared dead. The majority of cases were males (76.5%), Jordanians (70.6%), and the average age at time of death was 50 years (Table 1).
The majority of cases were declared dead at home (n = 11, 64.7%). Eight cases were diagnosed during the first COVID-19 wave in Jordan, while the remaining nine cases were diagnosed during the second wave of COVID-19 in the country.
The most frequent co-morbidities in the study cohort were hypertension and obesity (n = 5 for both). Previous emergency department visits were recorded for eight cases (four of which were for respiratory symptoms including shortness of breath and cough).
Four cases died with SARS-CoV-2 infection compared to 13 dying from COVID-19
Evidence of the presence of SARS-CoV-2 with the absence of DAD was found in four cases (23.5%). Based on that, the case series was divided into two groups “death with SARS-CoV-2 infection” vs. “death from COVID-19.” In the former group, two cases were presumptively diagnosed with pneumonia at death, one with ACS and the last case was diagnosed with subdural and subarachnoid hemorrhage. For the “death from COVID-19” group, six were diagnosed with pneumonia, four were diagnosed with pulmonary embolism, and three were diagnosed with acute coronary syndrome. The mean age of individuals within the “death with SARS-CoV-2 infection” was younger than the mean age of those within the “death from COVID-19” group (39 years vs. 54 years, p=.078, Mann-Whitney U test).
Absence of co-morbidities was recorded among all cases in the “death with SARS-CoV-2 infection” (0/4) in contrast to (9/11, 81.8%) having at least one co-morbid condition in the “death from COVID-19” group with missing data in two cases (p=.011, Fisher exact test).
Autopsy findings from lung tissues
Gross examination of the lungs in the study cohort revealed the common occurrence of congestion and edema followed by hepatization of lungs (Table 2).
On histopathologic examination, DAD was detected in 13/17 cases (76.5%), which was sub-classified into exudative DAD (n = 5), proliferative DAD (n= 7), and a single case of evolving fibrosing DAD. All cases with exudative DAD showed hyaline membrane formation, denudation and/or necrosis of type 1 pneumocytes (Fig. 1).
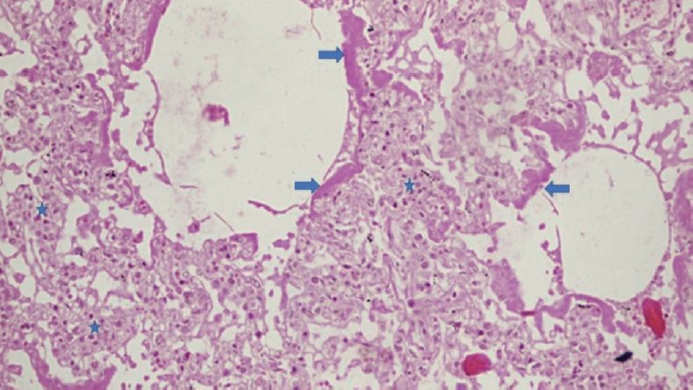
The histopathologic changes of a case with exudative phase of diffuse alveolar damage with hyaline membrane formation (arrows) and lymphocytic infiltrate (star).
Variable degrees of hyaline membrane organization and type II pneumocytes hyperplasia were noted in the seven proliferative DAD cases (Fig. 2).
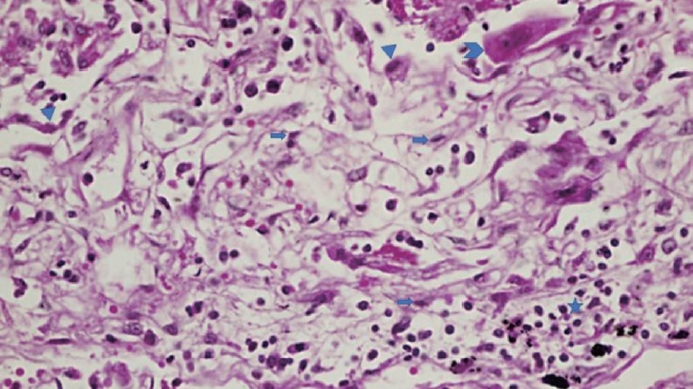
The histopathologic changes of a case with evolving fibrotic changes with type II pneumocytes hyperplasia (arrowhead), squamous metaplasia (chevron), expansion of septum with interstitial fibroblastic and myofibroblast proliferation (arrows), edema, and lymphocytic infiltrate (star).
A majority of cases displayed evidence of interstitial and intraalveolar edema (64.7%), lymphocytic infiltration of the alveoli (64.7%), and pulmonary capillaries congestion (100%). Microthrombi were found in eight cases (47%), of which two cases showed no DAD, two cases displayed exudative DAD, and four cases showed proliferative DAD. Emphysematous changes were noted in eight cases (Table 2, Fig. 3).
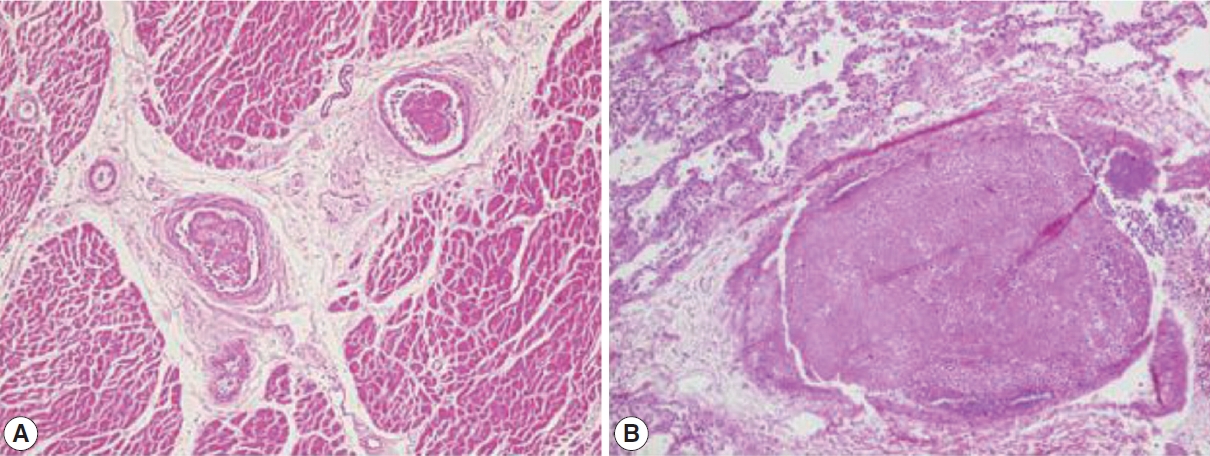
Intravascular microthrombi. (A) Heart tissue showing two intravascular microthrombi. (B) Lung with large thrombus occupying a medium sized vessel.
In the absence of co-morbidities, no specific histologic changes were noticed in alveoli (n=4), compared to the presence of lymphocytic infiltration in 8/9 of the cases with co-morbidities (p= .011, Fisher exact test). All cases in the “died with COVID-19” group lacked alveolar changes by definition (n=4), compared to 11/13 with lymphocytic infiltration in the “died from COVID-19” group (p=.006, Fisher exact test).
Autopsy findings from heart tissues
Gross examination of the heart in this case series revealed the relatively high prevalence of atherosclerotic changes in coronary arteries (n = 8, 47.1%). Histopathologic changes were scarcely detected. Fibrosis in intima and thickening of media were detected in a single case, while myocardial cell necrosis was found in another single case (Table 2).
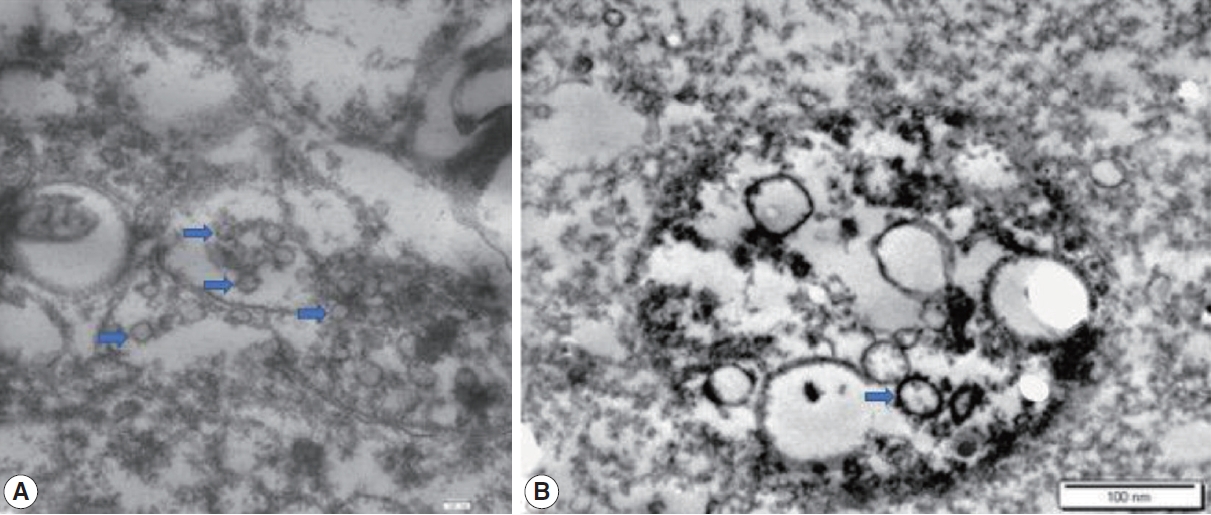
EM findings
All cases were examined using EM, and spherical structures with surface spikes were found in all cases (n=17, 100%) (Fig. 4).
DISCUSSION
This study represents the first description of autopsy findings from individuals positive for COVID-19 in Jordan, and Arab countries to the best of our knowledge. Previously, a majority of autopsy case series in the context of COVID-19 were mostly conducted in the United States, Europe, and China [21]. Such a study appears of prime importance in the Middle East region for a number of reasons. First, challenges were posed to forensic pathologists considering the controversies around the Islamic burial rituals and handling of corpses if autopsies revealed the presence of SARS-CoV-2 [33,34]. This is particularly relevant considering the evidence suggesting the presence of replicative SARS-CoV-2 a few days postmortem as shown in the study by Grassi et al. [35] that involved 29 autopsies examined in Italy. Our findings confirmed the presence of the virus in all cases included in this study. The diagnosis of COVID-19 in this case series was established by postmortem molecular or serologic testing for SARS-CoV-2 even in the absence of typical clinical presentation of COVID-19 at time of death. Second, this study is important in Jordan considering the previous evidence of high prevalence of embracing conspiratorial beliefs towards emerging virus infections that could entail irrational COVID denialism [36]. The findings of this study add an explicit proof of the presence of the virus among autopsies that tested positive for the virus through direct EM visualization. The confirmation of coronavirus presence by EM examination added further proof of virus presence in all included cases despite the variability in laboratory testing approach initially used in this case series (qPCR vs. serologic testing).
Macroscopic and microscopic findings in the majority of cases (13/17, 76.5%) in this study were consistent with previous literature suggesting the crucial role of DAD as the hallmark of acute respiratory distress syndrome complicating COVID-19 infections [37-39]. The predominance of proliferative DAD in this case series indicates the late presentation of a substantial number of cases with subsequent ominous outcome. The wide prevalence of DAD as the predominant feature in lung parenchyma among COVID-19–positive autopsies was reported previously in various reports from the United States [40,41], Germany [30,42], Spain [43], Italy [44], and China [45]. An early case series from Switzerland that involved 21 autopsies examined following COVID-19–related mortalities revealed that the major cause of death was respiratory insufficiency due to exudative DAD and massive capillary congestion [46]. In addition, the Swiss case series reported the detection of microthrombi despite the intake of anticoagulation prior to death [46].
The role of coagulopathy in the pathophysiology of COVID-19 was manifested by the frequent detection of microthrombi in lungs (8/17, 47.1%) in the study cohort. Likewise, and indicative of the central role of thrombotic microangiopathy in critical cases of COVID-19, a study from Iran reported the presence of thrombotic microangiopathy in 60% of 31 lung biopsies from patients who passed away due to COVID-19 [47]. Additional reports on autopsy findings amid COVID-19 pandemic found a high incidence of thromboembolic events suggesting its role in the fatal outcome of COVID-19 [39,48]. A recent comprehensive review for autoptic investigations from of 749 COVID-19 mortalities in 14 studies revealed the presence of pulmonary embolism-related findings in 30% of cases, with venous thromboembolic events as the cause of death 25% of the cases [49]. An early Austrian study involving 11 autopsies showed that thrombosis in small pulmonary arteries was a fundamental finding resulting in mortality due to COVID-19 [50].
The frequency of co-morbidities was high in this case series among mortalities that were linked directly to SARS-CoV-2 infection in contrast to its total absence among those who died with the disease. Conditions like hypertension, obesity, and type 2 diabetes mellitus were previously linked to excess mortality among SARS-CoV-2 infected patients [51]. In line with this observation, co-morbidities in this cohort were linked to death from COVID-19 rather than death with the virus.
A novel finding of this study was the observation that four out of 17 individuals died without significant histopathologic pulmonary changes. This observation was made despite the presence of SARS-CoV-2 as evidenced by qPCR, serology, and EM findings. One important parameter in the assessment of infectious disease is the CFR, which is defined as “the proportion of individuals diagnosed with a disease who die from that disease” [3]. The aspects of bias in the efforts to estimate COVID-19 CFR appear to cause an underestimation through time lags in reporting of death, and overestimation through underreporting of asymptomatic and mild cases [5]. Another important cause of bias, which was noticed in this study, is the overestimation of fatalities due to COVID-19. This can happen as a result of reporting any death with a positive SARS-CoV-2 testing result as a COVID-19 case, even in the absence of sufficient evidence that the individual died as a result of virus infection, which might be present as an incidental finding [52]. Such a scenario can frequently occur in the course of COVID-19 epidemic waves with a high proportion of asymptomatic cases/mild disease [16]. Hence, subclinical cases are rarely tested and consequently are missed.
In this study, even with a small sample size, the proportion of death with SARS-CoV-2 infection appears relatively high 4/17 (23.5%). In line with this finding, a study from Italy reported on the causes of death among nine cases that tested positive for COVID-19 at time of death, with five cases dying as a result of carbon monoxide poisoning in a nursing home (death with SARS-CoV-2 infection) [11]. In an earlier study from Germany, Edler et al. [42] found a similar observation; however, at a much smaller scale with only 5% out of 80 autopsies that were labeled as “non-COVID-19 deaths.”
It is important to note that the incidental finding of SARS-CoV-2 in autopsies can be higher in outbreak situation. The current study took place during the first and second waves of COVID-19 in Jordan, with more than several thousand of newly diagnosed cases at waves’ peaks [53]. Several differential diagnoses should be considered in outbreak setting with community spread of SARS-CoV-2, including other viral infections, previously undiagnosed heart disease, and drug toxicity among other conditions [54]. Despite the absence of DAD in four cases, the role of SARS-CoV-2 in mortality cannot be ruled out, particularly in the cases with ACS and this issue could be viewed as a caveat in our stratification approach. This is evidenced by the previous studies linking COVID-19 with direct cardiac damage and indirect involvement through the thrombotic complications [55]. However, we are inclined to believe that the cases in the “death with SARS-CoV-2 infection” group did not pass away due to SARS-CoV-2 complications since the subjects in this group lacked co-morbidities and were younger compared to those with histopathologic evidence of death due to the infection.
Finally, the findings in this case series should be interpreted in light of several limitations that included: (1) the small sample size, which was mostly related to restriction of autopsy examination to medicolegal cases; (2) potential selection bias since all deaths were considered as medicolegal cases; (3) missing of full clinical history data in a few cases, including the history of COVID-19 vaccine uptake among the four cases included following the start of vaccination campaign in Jordan, besides the lack of data on microbiologic testing to rule out bacterial superinfections; (4) the approach used to stratify the cases into “died of COVID-19” vs. “died with SARS-CoV-2 infection” depended on the detection of DAD solely. Thus, future studies should benefit from a refined approach of classification including consideration of detailed medical records from the included cases, as well as the full utility of postmortem radiology, besides toxicologic investigations [20]; and finally (5) virtual autopsy (virtopsy) was not conducted in this study and should be considered in the future studies considering its promising role for postmortem investigation in the context of resolving disputed cases of COVID-19 deaths.
To conclude, in this case series, we described the histopathologic findings of COVID-19–related mortalities and explored the distinction between death due to COVID-19 as opposed to dying with SARS-CoV-2 infection. This disparity might be supported by the younger age and absence of co-morbidities in the “died with COVID-19” group; however, this observation is pending further evidence from studies with larger samples. Besides DAD as the primary histopathologic finding among the “death from COVID-19” group, microthrombi were frequently detected. This microthrombi can be indicative of a hypercoagulability state. Such a state appears to play a prominent role in the pathophysiology of severe and critical cases of COVID-19, which can be implicated in the mortality from the disease.
Notes
Ethics Statement
This study was approved by the Institutional Review Board of Jordan University Hospital (JUH–IRB, decision No. 78/2021, reference No. 10/2021/5885, issued on 14 March 2021). The written informed consent from the next of kin was waived based on the medico-legal status of the cases.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author contributions
Conceptualization: MA, MAAA. Data curation: MA, IT, MS, ABH, IMAA, BAO, SAM, HAR, ASA, MZ, MAAA. Formal analysis: MA, MS. Funding acquisition: MA. Investigation: MA, IT, MS, ABH, IMAA, BAO, SAM, HAR, ASA, MZ, MAAA. Methodology: MA, IT, MS, ABH, IMAA, BAO, SAM, HAR, ASA, MZ, MAAA. Project administration: MA. Resources: MA, IT, MS, ABH, IMAA, BAO, SAM, HAR, ASA, MZ, MAAA. Supervision: MA, MAAA. Validation: MA, MS. Visualization: MA, MS. Writing— original draft preparation: MA, MS. Writing—review & editing: MA, IT, MS, ABH, IMAA, BAO, SAM, HAR, ASA, MZ, MAAA. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
This research was funded by Deanship of Scientific Research at the University of Jordan, grant number: 498/2021/19; (24/2020–2021), granted on 21 April 2021.