Primary Endometrial Squamous Cell Carcinoma: A Case Report and Review of Relevant Literature on Korean Women
Article information
Abstract
Primary endometrial squamous cell carcinoma (PESCC) is an extremely rare tumor with unclear pathogenesis. A 54-year-old postmenopausal woman presented with a 6-month history of vaginal bleeding. The patient was provisionally diagnosed with uterine submucosal leiomyoma. This was followed by total hysterectomy with a bilateral salpingo-oophorectomy under the laparoscopic guidance. Histopathologically, the tumor was PESCC which was accompanied by a lack of the tumor in the uterine cervix. The tumor showed positive immunoreactivity for p16INK4a. But there was no evidence of human papillomavirus (HPV) on in situ hybridization and HPV DNA chip analysis. We also present a review of the relevant literature on Korean women.
Primary endometrial squamous cell carcinoma (PESCC) is an extremely rare tumor, and its pathogenesis remains unclear. It was first reported by Gebhard in 1892.1 Its diagnostic criteria were established in 1928 by Fluhmann,2 and are as follows: 1) no coexistence of endometrial adenocarcinoma; 2) no connection between the endometrial tumor and the squamous epithelium of the cervix; and 3) no primary cervical squamous cell carcinoma (SCC). In 1975, the World Health Organization (WHO) added two other criteria: presence of intercellular bridges and keratinization.3 Here, we present a case of PESCC satisfying the WHO criteria with positive p16INK4a immunoreactivity and having no evidence of human papillomavirus (HPV).
CASE REPORT
A 54-year-old woman with gravidity 3 and parity 1, who had been postmenopausal for two years, presented with a 6-month history of vaginal bleeding and general weakness. The patient looked generally anemic and fatigued, and had no past history of taking estrogen replacement therapy. In addition, the patient had a body mass index of 24.5 kg/m2 and a blood cancer antigen 125 level of 24.2 U/mL (normal range, 0 to 35 U/mL). The patient had a normal Papanicolaou smear but no notable gynecological history. Pelvic examination revealed an enlarged uterus without palpable ovaries. Transvaginal ultrasound showed a 7-cm protruding mass in the endometrial cavity with an endometrial thickness of 22.3 mm. In addition, the mass was surrounded by echogenic blood flow and it showed an ill-defined margin with the myometrium.
The patient underwent total hysterectomy with a bilateral salpingo-oophorectomy under the laparoscopic guidance under a provisional diagnosis of submucosal leiomyoma. The tumor did not involve the serosal surface of the uterus or the abdominal cavity. The cervix, adnexa and vagina appeared normal. Grossly, there was an ill-defined, relatively solid endometrial mass with a spotty necrosis, measuring 7×6×5 cm. In addition, it involved the myometrium at the fundus and body but not its serosal tissue. Following a careful examination, the endometrial mass was divided into 12 sections in total. There were no notable findings in the uterine cervix and both adnexae. The entire uterine cervix was divided into 12 sections in total from the 12 o'clock position.
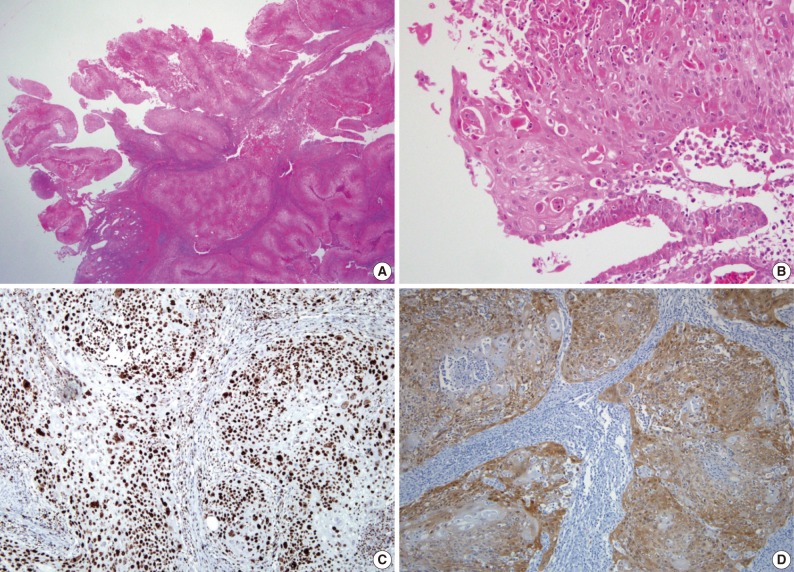
Microscopically, the tumor showed a clear evidence of squamous differentiation, such as presence of intercellular bridges and keratinization (Fig. 1A, B), thus confirming a well-differentiated, invasive SCC of the endometrium. The tumor involved more than 80% of the myometrial thickness and it showed a vascular invasion to the myometrium. In the adjacent non-neoplastic endometrium, there were glands with both a pseudostratification and a ciliary change and their stroma was infiltrated by inflammatory cells, plasma cells and neutrophils in particular (Fig. 1B). There were no evidences demonstrating the presence of squamous metaplasia of the endometrium, endometrial adenocarcinoma, cervical SCC and a connection between the endometrial tumor and the squamous epithelium of the cervix. Both fallopian tubes and ovaries were normal. Moreover, there was no evidence of SCC at other sites. These findings confirmed the diagnosis of PESCC rather than submucosal leiomyoma. On immunohistochemistry, there was a positive immunoreactivity for cytokeratin 7, p63 (Fig. 1C), and p16INK4a (Fig. 1D), but not for cytokeratin 20 and estrogen receptor (ER) and progesterone receptor (PR). Ki-67 was stained in 80% of the tumor cells. But HPV was not detected on either in situ hybridization (ISH) or HPV DNA chip analysis. The patient underwent radiotherapy for two months. The patient showed a disease-free course during a 13-month follow-up period.
DISCUSSION
It is generally known that endometrial SCC originates from the uterine cervix. The connection between the endometrium and the cervix should therefore be ruled out in making a diagnosis of PESCC. Squamous differentiation of an endometrioid adenocarcinoma must also be excluded.2
Several theories regarding the cellular origin of PESCC have been proposed: 1) reserve or stem cells located between the glandular basement membrane and the endometrial columnar cell layer;4 2) squamous metaplasia of the normal endometrium;5 and 3) heterotopic cervical tissue.6 It has been reported that vitamin A deficiency, anti-estrogen treatment, pyometra, chronic infection, uterine prolapse, myoma, intrauterine device, history of pelvic irradiation and curettage are associated with squamous metaplasia of the endometrium.2,5,7,8
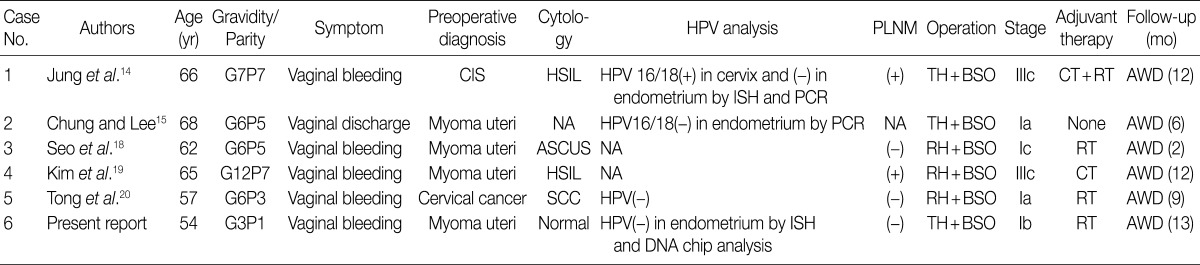
HPV infection plays a key role in the pathogenesis of squamous neoplasms of the uterine cervix,9 whose role in that of PESCC remains controversial. Of note, Kataoka et al.10 demonstrated the presence of HPV type 31 by the polymerase chain reaction (PCR) in one patient with PESCC. But there were no other reports demonstrating a clear association between HPV and PESCC.11-13 Horn et al.11 performed an HPV analysis with general primers and HPV typing in eight patients with PESCC. These authors noted that there was only one positive case for HPV type 16. Giordano et al.12 failed to detect HPV DNA by PCR in one patient with PESCC. In addition, Im et al.13 could not detect HPV by ISH in three patients with PESCC. According to review of literatures about five Korean women with PESCC (Table 1), there were one positive case for HPV 16/18 in the cervix but not the endometrium by ISH and PCR assay14 and another negative case for HPV 16/18 by PCR assay.15 Moreover, we did not find any evidence of HPV in our patient. We therefore suggest that HPV may not be the primary causative factor for PESCC.
A cyclin-dependent kinase-4 inhibitor involved in the pRb pathway, p16INK4a is a surrogate marker for HPV infection in cervical neoplasms.9 It has been reported that p16INK4a is expressed in some cases of endometrial carcinoma.11,16 To date, however, fewer attempts have been made to evaluate both the HPV status and p16INK4a expression. Ansari-Lari et al.16 reported that p16INK4a expression is moderate to strong and diffuse in endocervical adenocarcinoma and weak and patchy in endometrial adenocarcinoma. These findings suggest that p16INK4a immunohistochemistry may be helpful for distinguishing endocervical adenocarcinoma from endometrial adenocarcinoma. According to Horn et al.,11 50% of the cases showed a positive p16INK4a immunoreactivity but there was only one positive case for HPV. These reports suggest that alterations of the p16INK4a pathway may play a role in the pathogenesis of some cases of PESCC, if any, without an HPV involvement. Similarly, our case showed weak and patchy p16INK4a expression and negative results for HPV by both ISH and DNA chip analysis. Our case therefore indicates that p16INK4a overexpression may be involved in the development of PESCC with no respect to HPV infection.
The clinical applicability of the ER and PR status as a prognostic indicator of PESCC is still uncertain. Considering that most patients are postmenopausal, however, a loss of estrogen cannot be completely ruled out as an etiologic factor. This is not only because most cases of PESCC occur in postmenopausal women but also because one of the most frequent presenting symptoms is vaginal bleeding. The average duration of symptoms before diagnosis is 11.5 months.8
Total hysterectomy with a bilateral salpingo-oophorectomy is the first line of choice for menopausal women. The effectiveness of radiotherapy and chemotherapy as adjuvant treatments remains highly controversial.7,8 PESCC has a poor prognosis compared with endometrial adenocarcinoma. That is, it is well documented that the 5-year survival rates in endometrial adenocarcinoma at stages I, II, III, and IV are 89.1%, 78.8%, 57.8%, and 22.8%, respectively.17 However, the 5-year survival rate of PESCC is difficult to assess because of its rarity. With a survival period ranging from 14 to 36 months, it has been reported that the 1-year survival rates in PESCC at stages I, III, and IV are 80%, 20%, and 0%, respectively.7,8
The mean age of the six Korean patients (Table 1), including our case, was 62 years (range, 54 to 68 years), all of whom were postmenopausal.14,15,18-20 Most of the Korean women with PESCC are multiparous, which is contradictory to the report, by Goodman et al.,8 made from nulliparous women. In addition, vaginal bleeding is one of the typical symptoms that occur in Korean women.
In summary, there was positive p16INK4a immunoreactivity with no evidence of HPV by ISH and DNA chip analysis in our case. Our case highlights the significant role of p16INK4a overexpression, regardless of the HPV status in the pathogenesis of PESCC. Henceforth, however, further large-scale studies are warranted to gain a deeper insight into its characteristics of PESCC.
Notes
No potential conflict of interest relevant to this article was reported.