Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(4); 2012 > Article
-
Case Report
Primary Endometrial Squamous Cell Carcinoma: A Case Report and Review of Relevant Literature on Korean Women - Sung Jong Lee, Hyun Joo Choi1
-
Korean Journal of Pathology 2012;46(4):395-398.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.4.395
Published online: August 23, 2012
Department of Obstetrics and Gynecology, St. Vincent's Hospital, The Catholic University of Korea School of Medicine, Suwon, Korea.
1Department of Hospital Pathology, St. Vincent's Hospital, The Catholic University of Korea School of Medicine, Suwon, Korea.
- Corresponding Author: Hyun Joo Choi, M.D. Department of Hospital Pathology, St. Vincent's Hospital, The Catholic University of Korea School of Medicine, 93 Jungbu-daero, Paldal-gu, Suwon 442-723, Korea. Tel: +82-31-249-7592, Fax: +82-31-244-6786, chj0103@catholic.ac.kr
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Primary endometrial squamous cell carcinoma (PESCC) is an extremely rare tumor with unclear pathogenesis. A 54-year-old postmenopausal woman presented with a 6-month history of vaginal bleeding. The patient was provisionally diagnosed with uterine submucosal leiomyoma. This was followed by total hysterectomy with a bilateral salpingo-oophorectomy under the laparoscopic guidance. Histopathologically, the tumor was PESCC which was accompanied by a lack of the tumor in the uterine cervix. The tumor showed positive immunoreactivity for p16INK4a. But there was no evidence of human papillomavirus (HPV) on in situ hybridization and HPV DNA chip analysis. We also present a review of the relevant literature on Korean women.
- A 54-year-old woman with gravidity 3 and parity 1, who had been postmenopausal for two years, presented with a 6-month history of vaginal bleeding and general weakness. The patient looked generally anemic and fatigued, and had no past history of taking estrogen replacement therapy. In addition, the patient had a body mass index of 24.5 kg/m2 and a blood cancer antigen 125 level of 24.2 U/mL (normal range, 0 to 35 U/mL). The patient had a normal Papanicolaou smear but no notable gynecological history. Pelvic examination revealed an enlarged uterus without palpable ovaries. Transvaginal ultrasound showed a 7-cm protruding mass in the endometrial cavity with an endometrial thickness of 22.3 mm. In addition, the mass was surrounded by echogenic blood flow and it showed an ill-defined margin with the myometrium.
- The patient underwent total hysterectomy with a bilateral salpingo-oophorectomy under the laparoscopic guidance under a provisional diagnosis of submucosal leiomyoma. The tumor did not involve the serosal surface of the uterus or the abdominal cavity. The cervix, adnexa and vagina appeared normal. Grossly, there was an ill-defined, relatively solid endometrial mass with a spotty necrosis, measuring 7×6×5 cm. In addition, it involved the myometrium at the fundus and body but not its serosal tissue. Following a careful examination, the endometrial mass was divided into 12 sections in total. There were no notable findings in the uterine cervix and both adnexae. The entire uterine cervix was divided into 12 sections in total from the 12 o'clock position.
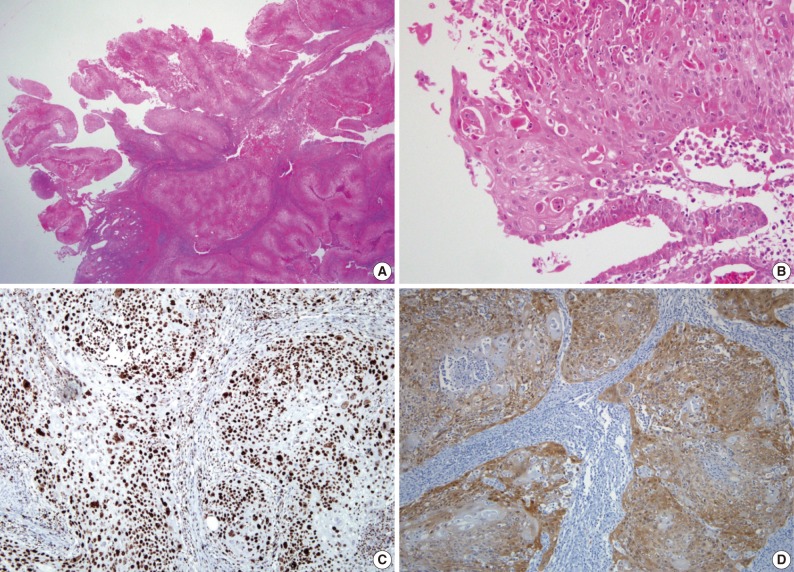
- Microscopically, the tumor showed a clear evidence of squamous differentiation, such as presence of intercellular bridges and keratinization (Fig. 1A, B), thus confirming a well-differentiated, invasive SCC of the endometrium. The tumor involved more than 80% of the myometrial thickness and it showed a vascular invasion to the myometrium. In the adjacent non-neoplastic endometrium, there were glands with both a pseudostratification and a ciliary change and their stroma was infiltrated by inflammatory cells, plasma cells and neutrophils in particular (Fig. 1B). There were no evidences demonstrating the presence of squamous metaplasia of the endometrium, endometrial adenocarcinoma, cervical SCC and a connection between the endometrial tumor and the squamous epithelium of the cervix. Both fallopian tubes and ovaries were normal. Moreover, there was no evidence of SCC at other sites. These findings confirmed the diagnosis of PESCC rather than submucosal leiomyoma. On immunohistochemistry, there was a positive immunoreactivity for cytokeratin 7, p63 (Fig. 1C), and p16INK4a (Fig. 1D), but not for cytokeratin 20 and estrogen receptor (ER) and progesterone receptor (PR). Ki-67 was stained in 80% of the tumor cells. But HPV was not detected on either in situ hybridization (ISH) or HPV DNA chip analysis. The patient underwent radiotherapy for two months. The patient showed a disease-free course during a 13-month follow-up period.
CASE REPORT
- It is generally known that endometrial SCC originates from the uterine cervix. The connection between the endometrium and the cervix should therefore be ruled out in making a diagnosis of PESCC. Squamous differentiation of an endometrioid adenocarcinoma must also be excluded.2
- Several theories regarding the cellular origin of PESCC have been proposed: 1) reserve or stem cells located between the glandular basement membrane and the endometrial columnar cell layer;4 2) squamous metaplasia of the normal endometrium;5 and 3) heterotopic cervical tissue.6 It has been reported that vitamin A deficiency, anti-estrogen treatment, pyometra, chronic infection, uterine prolapse, myoma, intrauterine device, history of pelvic irradiation and curettage are associated with squamous metaplasia of the endometrium.2,5,7,8
- HPV infection plays a key role in the pathogenesis of squamous neoplasms of the uterine cervix,9 whose role in that of PESCC remains controversial. Of note, Kataoka et al.10 demonstrated the presence of HPV type 31 by the polymerase chain reaction (PCR) in one patient with PESCC. But there were no other reports demonstrating a clear association between HPV and PESCC.11-13 Horn et al.11 performed an HPV analysis with general primers and HPV typing in eight patients with PESCC. These authors noted that there was only one positive case for HPV type 16. Giordano et al.12 failed to detect HPV DNA by PCR in one patient with PESCC. In addition, Im et al.13 could not detect HPV by ISH in three patients with PESCC. According to review of literatures about five Korean women with PESCC (Table 1), there were one positive case for HPV 16/18 in the cervix but not the endometrium by ISH and PCR assay14 and another negative case for HPV 16/18 by PCR assay.15 Moreover, we did not find any evidence of HPV in our patient. We therefore suggest that HPV may not be the primary causative factor for PESCC.
- A cyclin-dependent kinase-4 inhibitor involved in the pRb pathway, p16INK4a is a surrogate marker for HPV infection in cervical neoplasms.9 It has been reported that p16INK4a is expressed in some cases of endometrial carcinoma.11,16 To date, however, fewer attempts have been made to evaluate both the HPV status and p16INK4a expression. Ansari-Lari et al.16 reported that p16INK4a expression is moderate to strong and diffuse in endocervical adenocarcinoma and weak and patchy in endometrial adenocarcinoma. These findings suggest that p16INK4a immunohistochemistry may be helpful for distinguishing endocervical adenocarcinoma from endometrial adenocarcinoma. According to Horn et al.,11 50% of the cases showed a positive p16INK4a immunoreactivity but there was only one positive case for HPV. These reports suggest that alterations of the p16INK4a pathway may play a role in the pathogenesis of some cases of PESCC, if any, without an HPV involvement. Similarly, our case showed weak and patchy p16INK4a expression and negative results for HPV by both ISH and DNA chip analysis. Our case therefore indicates that p16INK4a overexpression may be involved in the development of PESCC with no respect to HPV infection.
- The clinical applicability of the ER and PR status as a prognostic indicator of PESCC is still uncertain. Considering that most patients are postmenopausal, however, a loss of estrogen cannot be completely ruled out as an etiologic factor. This is not only because most cases of PESCC occur in postmenopausal women but also because one of the most frequent presenting symptoms is vaginal bleeding. The average duration of symptoms before diagnosis is 11.5 months.8
- Total hysterectomy with a bilateral salpingo-oophorectomy is the first line of choice for menopausal women. The effectiveness of radiotherapy and chemotherapy as adjuvant treatments remains highly controversial.7,8 PESCC has a poor prognosis compared with endometrial adenocarcinoma. That is, it is well documented that the 5-year survival rates in endometrial adenocarcinoma at stages I, II, III, and IV are 89.1%, 78.8%, 57.8%, and 22.8%, respectively.17 However, the 5-year survival rate of PESCC is difficult to assess because of its rarity. With a survival period ranging from 14 to 36 months, it has been reported that the 1-year survival rates in PESCC at stages I, III, and IV are 80%, 20%, and 0%, respectively.7,8
- The mean age of the six Korean patients (Table 1), including our case, was 62 years (range, 54 to 68 years), all of whom were postmenopausal.14,15,18-20 Most of the Korean women with PESCC are multiparous, which is contradictory to the report, by Goodman et al.,8 made from nulliparous women. In addition, vaginal bleeding is one of the typical symptoms that occur in Korean women.
- In summary, there was positive p16INK4a immunoreactivity with no evidence of HPV by ISH and DNA chip analysis in our case. Our case highlights the significant role of p16INK4a overexpression, regardless of the HPV status in the pathogenesis of PESCC. Henceforth, however, further large-scale studies are warranted to gain a deeper insight into its characteristics of PESCC.
DISCUSSION
- 1. Gebhard C. Ueber die vom Oberflächenepithel ausgehenden Carcinomformen des Uteruskörpers sowie über den Hornkrebs des Cavum uteri. Z Geburtsh Gynakol 1892; 24: 1-8.
- 2. Fluhmann CF. The histogenesis of squamous cell metaplasia of the cervix and endometrium. Surg Gynecol Obstet 1953; 97: 45-58. ArticlePubMed
- 3. Paulsen H, Taylor C. International histological classification of tumors. No. 13. Histological typing of female genital tract tumours. 1975; Geneva: World Health Organization.
- 4. Baggish MS, Woodruff JD. The occurrence of squamous epithelium in the endometrium. Obstet Gynecol Surv 1967; 22: 69-115. ArticlePubMed
- 5. Seltzer VL, Klein M, Beckman EM. The occurrence of squamous metaplasia as a precursor of squamous cell carcinoma of the endometrium. Obstet Gynecol 1977; 49(1 Suppl):34-37. PubMed
- 6. Yamamoto Y, Izumi K, Otsuka H, Kishi Y, Mimura T, Okitsu O. Primary squamous cell carcinoma of the endometrium: a case report and a suggestion of new histogenesis. Int J Gynecol Pathol 1995; 14: 75-80. PubMed
- 7. Simon A, Kopolovic J, Beyth Y. Primary squamous cell carcinoma of the endometrium. Gynecol Oncol 1988; 31: 454-461. ArticlePubMed
- 8. Goodman A, Zukerberg LR, Rice LW, Fuller AF, Young RH, Scully RE. Squamous cell carcinoma of the endometrium: a report of eight cases and a review of the literature. Gynecol Oncol 1996; 61: 54-60. ArticlePubMed
- 9. Negri G, Egarter-Vigl E, Kasal A, Romano F, Haitel A, Mian C. p16INK4a is a useful marker for the diagnosis of adenocarcinoma of the cervix uteri and its precursors: an immunohistochemical study with immunocytochemical correlations. Am J Surg Pathol 2003; 27: 187-193. PubMed
- 10. Kataoka A, Nishida T, Sugiyama T, Hori K, Honda S, Yakushiji M. Squamous cell carcinoma of the endometrium with human papillomavirus type 31 and without tumor suppressor gene p53 mutation. Gynecol Oncol 1997; 65: 180-184. ArticlePubMed
- 11. Horn LC, Richter CE, Einenkel J, Tannapfel A, Liebert UG, Leo C. p16, p14, p53, cyclin D1, and steroid hormone receptor expression and human papillomaviruses analysis in primary squamous cell carcinoma of the endometrium. Ann Diagn Pathol 2006; 10: 193-196. ArticlePubMed
- 12. Giordano G, D'Adda T, Merisio C, Gnetti L. Primary squamous cell carcinoma of the endometrium: a case report with immunohistochemical and molecular study. Gynecol Oncol 2005; 96: 876-879. ArticlePubMed
- 13. Im DD, Shah KV, Rosenshein NB. Report of three new cases of squamous carcinoma of the endometrium with emphasis in the HPV status. Gynecol Oncol 1995; 56: 464-469. ArticlePubMed
- 14. Jung DW, Han SW, Kim NS, Hong SW, Yang SW, Hong M. Primary squamous cell carcinoma of the endometrium. Korean J Obstet Gynecol 1997; 40: 2092-2096.
- 15. Chung MJ, Lee DG. Primary squamous cell carcinoma of the endometrium covering submucosal leiomyoma. Korean J Pathol 1999; 33: 65-67.
- 16. Ansari-Lari MA, Staebler A, Zaino RJ, Shah KV, Ronnett BM. Distinction of endocervical and endometrial adenocarcinomas: immunohistochemical p16 expression correlated with human papillomavirus (HPV) DNA detection. Am J Surg Pathol 2004; 28: 160-167. PubMed
- 17. Creasman WT, Odicino F, Maisonneuve P, et al. Carcinoma of the corpus uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. Int J Gynaecol Obstet 2006; 95(Suppl 1):S105-S143.
- 18. Seo JY, Gu SJ, Park JH, Park TH, Kim TS, Kim IS. A case of primary endometrial squamous cell carcinoma. Korean J Obstet Gynecol 2001; 44: 1735-1738.
- 19. Kim JU, Lee YS, Moon SO, et al. A case of primary endometrial squamous cell carcinoma. Korean J Obstet Gynecol 2003; 46: 834-837.
- 20. Tong SY, Lee SK, Lee JH, Kim SB. Primary squamous cell carcinoma confined to the endometrium of submucosal myoma. Korean J Obstet Gynecol 2003; 46: 1024-1028.
REFERENCES
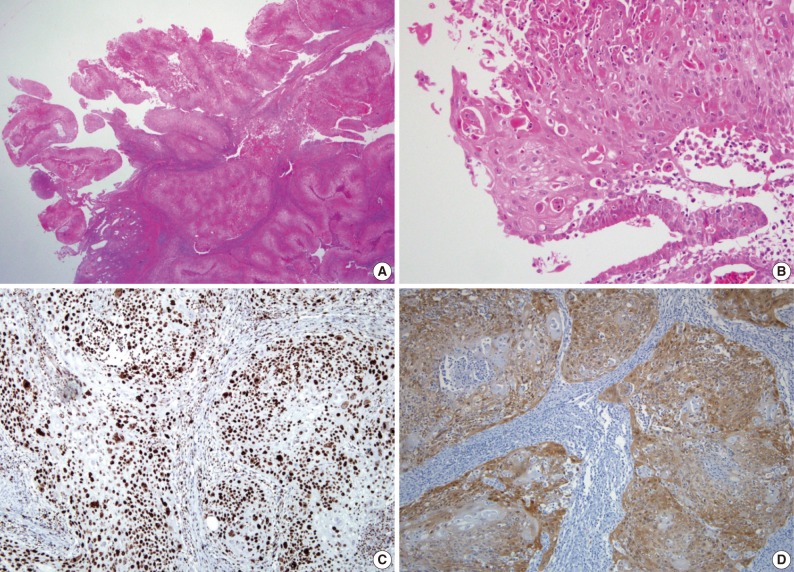
PESCC, primary endometrial squamous cell carcinoma; HPV, human papillomavirus; PLNM, pelvic lymph node metastasis; CIS, carcinoma in situ of the cervix; HSIL, high-grade squamous intraepithelial lesion; ISH, in situ hybridization; PCR, polymerase chain reaction; TH, total hysterectomy; BSO, bilateral salpingo-oophorectomy; CT, chemotherapy; RT, radiation therapy; AWD, alive with the disease; NA, unknown; ASCUS, atypical squamous cells of undetermined significance; RH, radical hysterectomy; SCC, squamous cell carcinoma.
Figure & Data
References
Citations

- Primary endometrial squamous cell carcinoma (PESCC): Review of the literature and case report
Kuang-Han Liu, Chia-Chin Tsai, Krystal Baysan Lin, Pei-Shen Huang
Taiwanese Journal of Obstetrics and Gynecology.2025; 64(1): 159. CrossRef - Primary squamous cell carcinoma of the uterine wall associated with adenomyosis: A rare case report and literature review
Yang Li, Lanlan Xuan, Qiucheng Wang
International Journal of Gynecology & Obstetrics.2025;[Epub] CrossRef - p16 Block Type Overexpression, p53 Wild Type Reactivity, and Cervical Involvement do not Always Exclude the Diagnosis of Primary Endometrial Squamous Cell Carcinoma (PESCC)
Daniela Fanni, Clara Gerosa, Michele Peiretti, Valerio Mais, Elena Massa, Stefano Angioni, Gavino Faa
International Journal of Gynecological Pathology.2024; 43(2): 200. CrossRef - Pathogenetic characteristics of endometrioid adenocarcinoma of uterus at present stage
T. I. Moiseenko, S. V. Shatalova, E. M. Nepomnyashchaya, V. A. Bandovkina, M. L. Adamyan
Medical alphabet.2024; (36): 35. CrossRef - Case report: Clinicopathological characteristic of two cases of primary endometrial squamous cell carcinoma and review of the literature
Hui-Bin Zhang, Li-Hua Lin, Qiu-Ping Lin, Yuan-Qing Lin, Dan Luo, Shu-Xia Xu
Frontiers in Oncology.2024;[Epub] CrossRef - Treatment of primary squamous cell carcinoma of the endometrium and review of previous literature: A case report
Liyun Song, Qi Wu, Suning Bai, Ren Xu, Xiaona Wang, Yanyan Yang
Medicine.2023; 102(17): e33667. CrossRef -
Prevalence of
human papilloma virus
and
Chlamydia trachomatis
in endometrial and cervical carcinoma: a comparative study in North Indian women
Heena Gautam, Sumita Mehta, Nidhi Nayar, Neha Kumar, Syed Akhtar Husain, Mausumi Bharadwaj
Systems Biology in Reproductive Medicine.2023; 69(6): 399. CrossRef - PAX8 Positivity, Abnormal p53 Expression, and p16 Negativity in a Primary Endometrial Squamous Cell Carcinoma: A Case Report and Review of the Literature
Daniela Fanni, Michele Peiretti, Valerio Mais, Elena Massa, Clara Gerosa, Francesca Ledda, Maria Luisa Fais, Gavino Faa, Stefano Angioni
International Journal of Gynecological Pathology.2022; 41(4): 431. CrossRef - Molecular Analysis of HPV-independent Primary Endometrial Squamous Cell Carcinoma Reveals TP53 and CDKN2A Comutations
Mark R. Hopkins, Doreen N. Palsgrove, Brigitte M. Ronnett, Russell Vang, Jeffrey Lin, Tricia A. Murdock
American Journal of Surgical Pathology.2022; 46(12): 1611. CrossRef - Primary squamous cell carcinoma of the endometrium—Case report with cytological characteristics in direct and indirect endometrial samples
Sanda Rajhvajn, Ana Barišić, Lada Škopljanac‐Mačina, Danijela Jurič, Vesna Mahovlić
Cytopathology.2021; 32(6): 823. CrossRef - Primary squamous cell carcinoma of the endometrium associated with human papilloma virus in a young woman: a case report
Tchin Darré, Abdoul-Samadou Aboubakari, Lantam Sonhaye, Baguilane Douaguibe, Akila Bassowa, Gado Napo-Koura
Journal of Medical Case Reports.2019;[Epub] CrossRef - Primary squamous cell carcinoma of the endometrium in a woman of perimenopausal age
Chao Zhang, Hongyan Zhang, Linqing Yang, Yunfei Wang, Xiaoyu Li, Jinfeng Guo, Jing Xu
Medicine.2018; 97(48): e13418. CrossRef - S100P is Overexpressed in Squamous Cell and Adenosquamous Carcinoma Subtypes of Endometrial Cancer and Promotes Cancer Cell Proliferation and Invasion
Hongfei Jiang, Hang Hu, Fan Lin, Yoon Pin Lim, Yunfen Hua, Xiaomei Tong, Songying Zhang
Cancer Investigation.2016; 34(10): 477. CrossRef - Überraschung in der Abradatdiagnostik
U. Kellner, A. Kellner, U. Cirkel
Der Pathologe.2015; 36(3): 317. CrossRef

Fig. 1
PESCC, primary endometrial squamous cell carcinoma; HPV, human papillomavirus; PLNM, pelvic lymph node metastasis; CIS, carcinoma

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article