Human Papillomavirus Prevalence and Cell Cycle Related Protein Expression in Tonsillar Squamous Cell Carcinomas of Korean Patients with Clinicopathologic Analysis
Article information
Abstract
Background
Human papillomavirus (HPV)-related tonsillar squamous cell carcinoma (TSCC) has recently been characterized as a distinct subset with a favorable prognosis. The prevalence and clinicopathologic significance of HPV-related TSCC in Koreans are not well known.
Methods
HPV in situ hybridization (ISH) accompanied by p53, p16, pRb, and cyclin D1 immunohistochemical staining were performed on 89 resection cases of TSCC from 2000 through 2010.
Results
HPV was detected by ISH in 59 of 89 cases (66.3%). HPV-positive TSCCs were more common in younger ages (p=0.005), and tumor sizes were smaller in the HPV-positive compared to the HPV-negative group (p=0.040). Positive HPV staining was significantly correlated with p16 expression (p<0.001), pRb inactivation (p=0.003), and cyclin D1 down-regulation (p<0.001) but not with p53 expression (p=0.334). Seventeen cases that showed p16-immunopositivity with HPV-negativity by ISH were retested by HPV typing; HPV DNA was not detected in all cases. There was no significant difference between HPV-positive and HPV-negative patients either in the disease-specific survival (DSS, p=0.857) or overall survival (p=0.910). Furthermore, pRb-inactivated cases showed better DSS (p=0.023), and p53-positive cases showed worse DSS (p=0.001).
Conclusions
Although high HPV prevalence was noted, it was not correlated with histopathologic findings or survival benefit. In addition to p53 expression, pRb inactivation along with p16 overexpression and down-regulation of cyclin D1 are thought to be important pathogenetic steps for developing TSCCs.
Head and neck squamous cell carcinoma (HNSCC) is a clinically challenging disease group with more than 551,000 new cases and over 306,000 deaths worldwide in 2008.1 It is well known that the most important risk factors for HNSCC are tobacco use and alcohol consumption. In addition to these classic risk factors, human papillomavirus (HPV) infection has recently been identified as an independent risk factor for HNSCC, especially of oropharyngeal cancers.2 Interestingly, the incidences of oropharyngeal cancers have been increasing in the US and Korea over the past decade, while those of laryngeal cancers have decreased.3,4 This increasing incidence pattern may be related to an HPV epidemic; however, its relationship with HNSCC in Korean patients has not been clarified.
The reported prevalence of HPV in oropharyngeal or tonsillar SCC over the past two decades varies broadly, ranging from 0% to 100%, depending on the location, patient ethnicity, specimen type, and detection method.2,5-10 The clinical significance of this subset has not been completely determined, though HPV-positive HNSCC patients had a tendency to be younger with no history of smoking or alcohol consumption and show a favorable prognosis.11 Also, morphologic characteristics of HPV-positive tumors have been described as non-keratinizing, poorly differentiated, having basaloid morphology with cystic cervical lymph node metastasis, or tonsillar crypt origin.7,8,12,13
The oncogenic HPV disrupts the cell cycle through two viral oncoproteins, E6 and E7, which functionally inactivate p53 and pRb tumor suppressor proteins, respectively. The disruption yields down-regulation of p53, pRb, and cyclin D1 and up-regulation of cyclin-dependent kinase inhibitors p16INK4A, p21CIF1/WAF1, as well as p14ARF. The aims of this study are to identify the prevalence of HPV in tonsillar squamous cell carcinoma (TSCC) from Korea, a low but increasing incidence region, to observe the clinicopathologic features of HPV-associated TSCC and to determine the prognostic values of HPV and related proteins.
MATERIALS AND METHODS
Patients and tumor materials
Formalin-fixed, paraffin-embedded tissue blocks were obtained from 89 patients diagnosed with TSCC who were treated with surgery and neoadjuvant and/or postoperative adjuvant chemoradiotherapy during the period from January 2000 to December 2010 at Asan Medical Center, Seoul, Korea. Clinical information including age, gender, histories of smoking and alcohol consumption, tumor-node-metastasis (TNM) stage, and survival were abstracted from the electronic medical records. Tumors were staged according to the 7th edition of the TNM classification scheme from the American Joint Committee on Cancer 2010. Smoking history was measured in pack-years and classified into three categories: non-smoker, former smoker that quit smoking more than ten years ago, or current smoker. Alcohol consumption was defined as having no history of alcohol use, having three or fewer drinks per day, or having more than three drinks per day.
All hematoxylin and eosin-stained sections were reviewed for reconfirmation of the diagnosis. Tumor differentiation was further sub-classified into three categories according to the World Health Organization (WHO) classification: well differentiated, moderately differentiated, and poorly differentiated squamous cell carcinoma. Tumor origin was divided into crypt or surface according to the location and growth direction of tumors. Tumors were also examined to determine whether keratinization was present. Duplicated 2 mm tissue cores were arrayed to decrease sampling errors and minimize tissue loss during processing. Tissue microarray sections were evaluated by HPV in situ hybridization (ISH), p16, pRb, cyclin D1, and p53 immunohistochemistry.
HPV ISH
An INFORM HPV III Family 16 Probe (B) was used in conjunction with ISH iView Blue Plus detection kit (Ventana Medical System Inc., Tucson, AZ, USA). The INFORM HPV III Family 16 Probe (B) detects the following high risk HPV genotypes: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, and 66. Using light microscopy, any blue nuclear dots in the tumor cells were regarded as positive staining. All cases were classified in a binary scheme as either positive or negative.
Immunohistochemistry
Immunoperoxidase staining was performed on 4-micrometer tissue microarray sections using a Ventana autostainer and ultraView DAB detection kit (Ventana Medical System Inc.) according to the manufacturer's instructions. The following antibodies were used: monoclonal p16INK4 (1:10, Pharmingen, Franklin Lakes, NJ, USA), monoclonal p53 (1:3,000, DAKO-M7001, DAKO, Glostrup, Denmark), monoclonal pRb (1:40, DAKO-M7131), and monoclonal cyclin D1 (1:100, Neomarkers, Fremont, CA, USA). p16INK4 expression was regarded as positive if strongly and diffusely stained in nuclei and/or cytoplasm in ≥70% of the tumor cells. p53, pRb, and cyclin D1 staining were scored as positive if strong and diffuse nuclear staining was present in ≥20% of the tumor cells.
DNA extraction
HPV-negative, p16-positive cases were retested by HPV DNA chip. DNA was extracted from formalin-fixed paraffin-embedded tissue using a LaboPass Tissue Mini DNA Purification Kit (Cosmo Genetech, Seoul, Korea). Paraffin-embedded tumor tissues were cut into 20 µm-thick sections, using disposable microtome blades, and three consequent sections were collected using microcentrifuge tubes. Then, two extractions were mixed with 1.2 mL of xylene, and excess xylene was removed by two 1.2 mL 100% ethanol washes. Dried tissue samples were incubated with lysis buffer and proteinase K at 56℃ for 30 minutes. Subsequently, the mixture was applied to the spin column and centrifuged into a collection tube according to the manufacturer's protocol. The purified DNA was used directly for polymerase chain reaction (PCR).
DNA amplification and HPV genotyping
A commercially available HPV DNA chip (Goodgene, Seoul, Korea) was used. The HPV DNA chip contained 40 type-specific probes: 21 types of high-risk type HPV (16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 67, 68, 69, 70, 73, and 82) and 19 types of low-risk type HPV (6, 11, 30, 32, 34, 40, 41, 42, 43, 44, 54, 55, 61, 62, 72, 81, 83, 84, and 90). Briefly, DNA amplification was performed in a 2720 Thermal Cycler (Applied Biosystems, Foster City, CA, USA) by PCR with primer sets, which target L1 and L2 regions of HPV DNA. As a control gene, the human β-globin gene was also amplified. The PCR products from all samples were detected by electrophoresis using 2% agarose gels, and the HPV DNA product size was 185 base pairs. Hybridized HPV DNA was visualized using a DNA chip scanner (GeneScan, Goodgene). To avoid contamination that may yield a false positive result, all PCR-related work was performed in specialized zones within a PCR laboratory.
Statistical analysis
Two-tailed Fisher's exact test and/or χ2 test were used to analyze the correlation between the clinicopathologic variables and HPV status. For continuous variables (e.g., tumor size), Student's t-test was chosen to evaluate the difference between HPV-negative and -positive groups. Survival analysis was performed based on Kaplan-Meier method and compared by log-rank test. All potential prognostic factors with a p-value<0.05 from the univariate analysis were incorporated into the multivariate analysis. The univariate and multivariate analyses were performed using the Cox proportional hazard regression model. All statistical analyses were conducted using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA). A p-value<0.05 was considered to be significant.
RESULTS
The patients were comprised of 81 (91%) men and eight (9%) women with a mean age of 55 years, ranging from 25 to 78. HPV was detected in 59 (66.3%) cases by ISH. The mean age of patients was significantly younger in the HPV-positive group (53.7±8.76) relative to the HPV-negative group (59.0±10.93, p=0.020). HPV positivity was not associated with gender (p=1.000), smoking history (p=0.490), or alcohol consumption (p=0.907). HPV-positive tumors were smaller in size (2.34±1.00 cm) than HPV-negative tumors (2.96±1.42 cm, p=0.040). However, anatomic stage, T stage, N stage, and M stage were not associated with HPV status (Table 1).
Comparison of immunohistochemistry with HPV status is demonstrated in Table 2 and Fig. 1. In total, 83.1% (74/89) of TSCCs were p16-positive, 5.6% (5/89) pRb-positive, 23.6% (21/89) cyclin D1-positive, and 27.0% (24/89) p53-positive. Strong positive correlation between p16 expression and HPV status (p<0.001) and an inverse correlation between expressions of pRb and cyclin D1 and HPV positivity (p=0.003 and p<0.001, respectively) were noted. HPV positivity was noted in 77% (57/74) and 13.3% (2/15) of p16-positive and -negative tumors, respectively. None of the pRb-positive tumors were HPV-positive (0/5), whereas 59 (70%) of 84 pRb-negative tumors were HPV-positive. While 28.6% (6/21) of cyclin D1-overexpressing tumors were HPV-positive, 77.9% (53/68) of cyclin D1-negative tumors showed HPV-positivity. There was no significant correlation between HPV status and p53 expression (p=0.334).
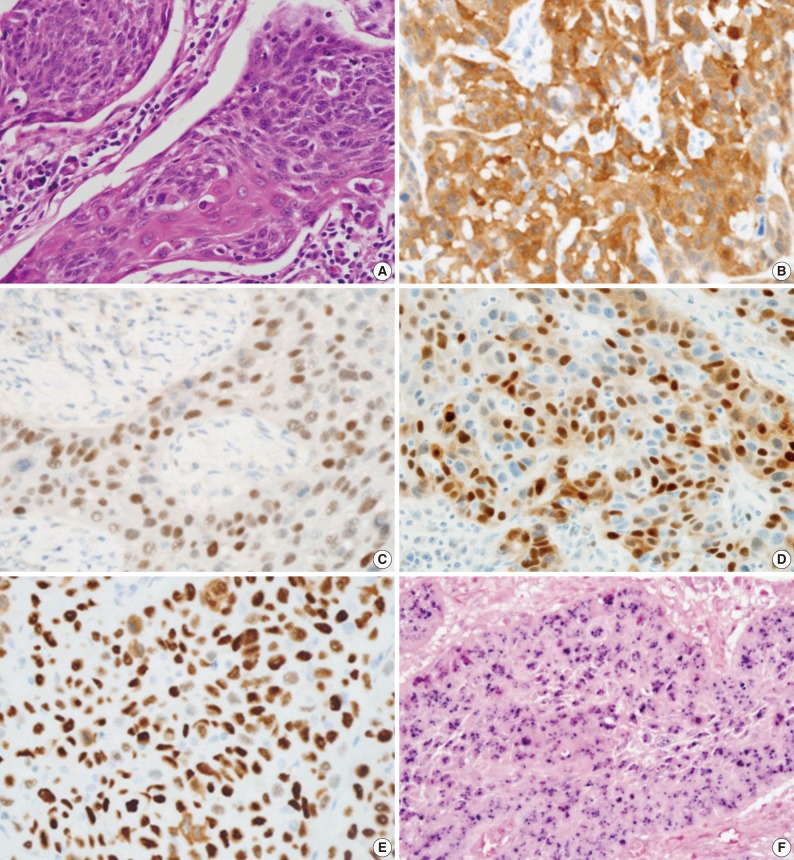
Representative photographs of tonsillar squamous cell carcinoma stained with (A) hematoxylin-eosin, and antibodies against (B) p16, (C) pRb, (D) cyclin D1, (E) p53, and (F) human papillomavirus in situ hybridization.
HPV genotyping using DNA chip was performed on the 17 cases that showed positive p16-staining but negative HPV staining by ISH. No HPV DNA was detected by genotyping in any of the 17 cases.
Upon histopathologic analysis, positive HPV results were higher in the crypt origin TSCCs (46/64, 72%) compared to surface origin TSCCs (13/25, 52%), but this difference was not statistically significant (p=0.075). In addition, there were no significant correlations between tumor differentiation, keratinization, cystic cervical lymph node metastasis, and HPV status (Table 3).
Follow-up periods ranged from 7 to 135 months with a mean follow-up of 55 months. The recurrence rate was 15.7% (14/89), with 15.2% (9/59) in the HPV-positive group and 16.6% (5/30) in the HPV-negative group (p=0.430). Our findings revealed no significant survival benefit by HPV status not only in overall survival (OS, p=0.910), but also in disease-specific survival (DSS, p=0.857) (Fig. 2). pRb positivity was significantly related to a worse OS (p=0.023) but was not related to DSS (p=0.681) (Fig. 2). The patients who showed high p53 expression had remarkably worse DSS (p=0.001) without affecting OS (p=0.997) (Fig. 3). Other cell cycle-related proteins, p16 and cyclin D1, did not show significant correlation with OS (p16, p=0.866; cyclin D1, p=0.204) or DSS (p16, p=0.468; cyclin D1, p=0.939). We performed survival analysis with combinations of HPV ISH status and the expression status of cell cyclerelated proteins. Each group was divided to four subgroups (i.e., HPV-positive/p16-positive; HPV-positive/p16-negative; HPV-negative/p16-positive; HPV-negative/p16-negative). Any HPV status with p16, pRb, or cyclin D1 expression status did not influence OS and DSS. However, the HPV-negative/p53-positive subgroup showed worse DSS than the other HPV-positive/p53-positive, HPV-positive/p53-negative, and HPV-negative/p53-negative subgroups (p=0.000) (Fig. 3). In univariate and multivariate Cox proportional analyses, T stage (T1-T2 vs T3-T4; hazard ratio, 5.444; 95% confidence interval [CI], 1.641 to 18.062; p=0.006) and pRb expression status (positive vs negative; hazard ratio, 0.109; 95% CI, 0.010 to 1.153; p=0.066) were identified as independent factors for OS in TSCC patients. M stage (M0 vs M1; hazard ratio, 8.215; 95% CI, 2.641 to 25.553; p=0.0003) and p53 expression status (positive vs negative; hazard ratio, 0.185; 95% CI, 0.063 to 0.547; p=0.002) were revealed as independent predictors for DSS.
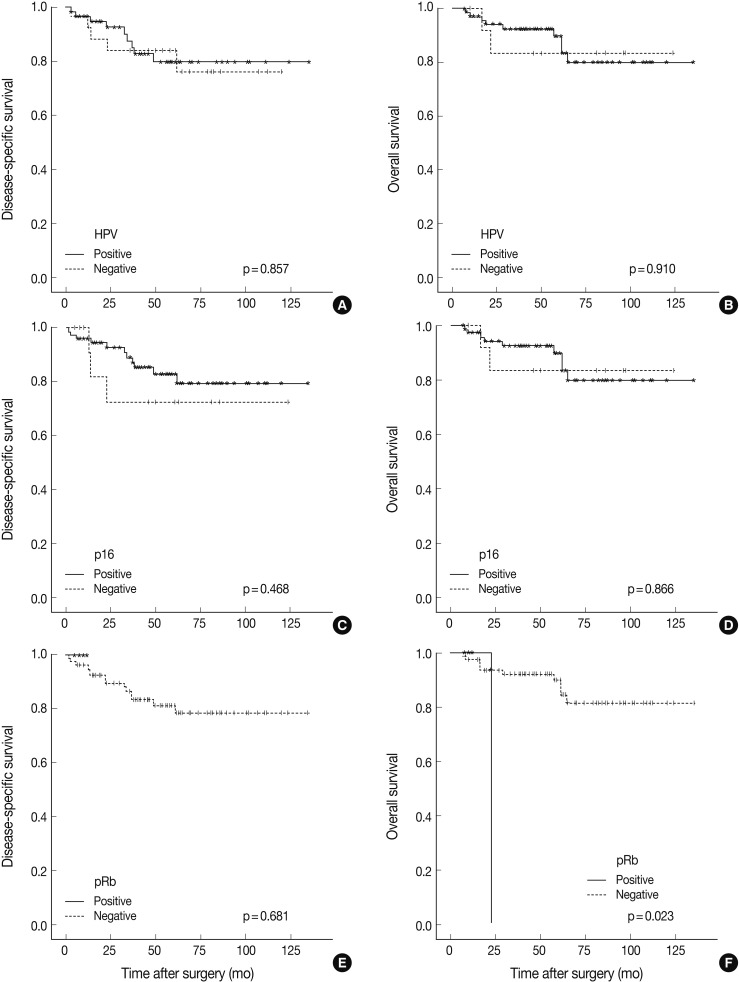
Kaplan-Meier survival curves by log-rank test. Disease-specific survival for (A) human papillomavirus (HPV), (C) p16, and (E) pRb. Overall survival for (B) HPV, (D) p16, and (F) pRb.
DISCUSSION
In prior studies, HPV infection rates in head and neck squamous cell carcinomas varied considerably, ranging from 0% to 100%.5,6 In our study, HPV was detected in 59/89 (66.3%) of TSCC patients by in ISH. The differences in HPV prevalence among the studies might be explained by the HPV detection methodology, sample size, and changes in lifestyle with time, such as tobacco use, alcohol consumption, and sexual behavior. Although high risk sexual habits such as oral sex may not be common in Korea, the considerably high prevalence of HPV could mean that other infection routes than sexual transmission are important for Koreans.
For HPV detection, ISH and PCR have been most widely used, and both methods have merits and limitations. ISH can visualize the virus in nuclei of tumor cells, but it is less sensitive than PCR depending on the copy number of viral genome, and it cannot demonstrate oncogenic transcription. On the other hand, PCR is a more sensitive method but may detect the virus present in non-tumor cells that are not clinically relevant or virus from the laboratory environment or other specimens, leading to false-positive results.14 HPV genotyping, another method of HPV detection, has the advantage of simultaneous detection of multiple HPV subtypes with high sensitivity, but its cost is high. Considering these problems, the difficulty lies in using ISH, PCR, or HPV genotyping as screening tests for HPV detection. Therefore, p16 immunoreactivity has been proposed as a surrogate marker for HPV-positive tumors of the anogenital tract, as well as the upper aerodigestive tract.15
p16 is a tumor suppressor gene that prevents progression of the S-phase of cell cycle, through blocking cyclin D/CDK2-mediated phosphorylation of pRb, thereby keeping the pRb checkpoint in place. In HPV-positive tumors, p16 overexpression is observed due to loss of negative feedback by inactivation of pRb by HPV oncoprotein E7.16 In this study, HPV-positive tumors showed high p16 overexpression (98%, 58/59) and low pRb immunoreactivity (0%, 0/59), and these results were in agreement with previous reports.17,18 However, 17 cases of HPV-negative tumors also showed p16 overexpression. These p16-positive/HPV-negative tumors were retested by HPV genotyping using DNA chip, and none of them were shown to harbor any of the 21 types of high-risk or 19 types of low-risk HPV. This result confirmed the accuracy of HPV ISH applied in our study. On the contrary, Lewis et al.19 found 42% of p16-positive/HPV-negative cases as positive for HPV on repeated PCR. We share a view with Perrone et al.20 that the false positive rate of PCR cannot be ignored. The mechanisms of p16-overexpression in HPV-negative tumors have not been ascertained. One can conjecture that p16 expression might be innate, and the tumor could develop independently regardless of HPV infection. HPV might be shed to tumors with genetic progression, resulting in pRb gene deletion or suppressed pRb gene expression independent of active viral protein expression.19 Also, other pRb pathway disturbances, regardless of HPV status such as mutational inactivation of RB protein, can be considered.21 Methodologically, there may be yet unidentified HPV genotypes that current HPV-specific tests cannot detect and do not contain the consensus DNA sequences detectable by ISH, PCR, or genotyping.19 Robinson et al.22 found 5% of p16-positive/HPV ISH-negative results in six studies examining 496 oropharyngeal squamous cell carcinomas, while Song et al.9 reported a greater number of p16-positive/HPV ISH-negative cases at 27.6% (13/47) in Koreans. The high proportion of p16-positive/HPV ISH-negative cases in our results (19.1%, 17/89) together with the result of Song et al.9 suggest that this considerably high incidence of p16-positive/HPV ISH-negative cases may be a distinguishing feature of TSCC in Koreans. Furthermore, in light of these results, there are limitations in using p16 as a surrogate marker for judging HPV infection status.
In HPV-infected tumor cells with p16 expression, its downstream regulators such as pRb or cyclin D1, may exhibit diverse expression profiles. Several studies have reported the rate of cyclin D1 overexpression in head and neck cancers as 17-80%.23,24 Overexpression of cyclin D1 might result from gene amplification, gene rearrangement, or post-translational modification. In oral cavity cancers, prognostic significance of cyclin D1 or pRb and the relationship between expression profiles of these proteins and HPV status have been diverse in previous studies.18,25 Our results showed an inverse correlation between expression of cyclin D1 and pRb with HPV ISH status (cyclin D1, p<0.001; pRb, p=0.003). While cyclin D1 overexpression had no effects on overall or DSS outcome, pRb overexpression was significantly correlated with worse OS (p=0.023), and pRb expression was identified as an independent predictor for OS by univariate and multivariate analyses.
In HPV-related tumors, wild-type p53 undergoes ubiquitination and degradation by HPV oncoprotein E6, resulting in less immunopositive protein.7,26 Thus, focal positive or negative p53 immunoreactivity has been regarded as a molecular signature for HPV-induced tumors. However, E6 degradation of p53 protein is not functionally equivalent to p53 mutation. Although HPV-infected cells express E6 oncoprotein, endogenous wild-type p53 can activate some target genes.27 In this study, p53 immunopositive rates were not significantly different between HPV-positive and -negative groups (24% vs 30%). However, p53-positive TSCC showed worse DSS (p=0.001). Although we did not perform p53 mutation analysis, 14 HPV-positive/p53-immunoreactive cases in this study might have harbored non-disruptive p53 mutations, according to Westra et al.,28 and may be related to smoking habits. Our results showed that p53-immunopositivity was related to a worse DSS (p=0.001), and p53 was an independent prognostic factor for DSS by univariate and multivariate analyses. Furthermore, upon combination analysis of HPV status and p53 immunoreactivity status, the HPV-negative/p53-positive subgroup showed the worst DSS. From these results, p53 status seems to be a single important factor for predicting DSS.
According to our results, no survival benefits were observed in HPV-positive TSCC patients in comparison with HPV-negative patients. This phenomenon might be attributed to higher smoking or drinking rates in Korea than in developed countries. According to the records of the Ministry of the Health and Welfare of Korea for 2008, the smoking rates were 40.9% in males and 4.1% in females, with a mean of 22.3%. In contrast, the U.S. Centers for Disease Control announced the smoking rates as 23% in males and 18% in female, and a mean of 20.6%. In light of these differences, it can be presumed that the higher smoking rates in males account for a majority of TSCC in Korea and thereby have a greater effect on survival than does HPV status, resulting in no survival benefits as analyzed by HPV infection. Hafkamp et al.10 reported marked differences in survival rate between smokers and non-smokers with HPV 16-associated tonsillar carcinomas. Interestingly, past results of Western studies parallel ours with respect to relationships of HPV infection and survival outcomes.29,30 There is a possibility that, with smoking rates reducing gradually in Western countries, the subset of HPV-related tumors has become outstanding. Clinical implication of HPV-positive oropharyngeal cancer may yet vary depending on sociocultural circumstances.
Routine HPV assessment is a rising issue in the standard pathologic evaluation of HNSCCs to assess cancer risk, predict patient outcomes, determine the site of tumor origin for metastatic tumors, and guide therapeutic strategies. Although high HPV prevalence was noted and epidemic HPV infection is suspected in Korea, we failed to segregate the HPV-positive TSCC cases as a clinically or pathologically distinct subset. The prognostic value of HPV and related proteins in HNSCC remains to be studied more elaborately.
In conclusion, high HPV prevalence in TSCCs (66.3%) is noted in Koreans. In addition to p53 expression, pRb inactivation along with p16 overexpression and down-regulation of cyclin D1 are thought to be important pathogenetic steps for developing TSCCs. In the present study, HPV status was not correlated with histopathologic features or survival benefits.
Notes
No potential conflict of interest relevant to this article was reported.



