Imprint Cytology of Soft Tissue Myoepithelioma: A Case Study
Article information
Abstract
Soft tissue myoepithelioma is a rare neoplasm composed of myoepithelial cells. Here, we describe the cytologic features of soft tissue myoepithelioma arising on the right forearm in an 18-year-old man. The excised tumor (3.0×1.8×1.5 cm) was well-demarcated, yellow-gray, soft, and myxoid. The cytologic smears showed round to spindle, epithelioid, and plasmacytoid cells in the myxoid background. The nuclei were uniform, round to ovoid, with finely distributed chromatin and eosinophilic or pale cytoplasm. The tumor cells demonstrated immunoreactivity for cytokeratin (AE1/AE3), epithelial membrane antigen, S100 protein, and glial fibrillary acidic protein. Electron microscopy showed intermediate filaments, desmosomes, and basal lamina.
Soft tissue myoepithelioma is a rare neoplasm of soft tissue. It is composed of cells with myoepithelial differentiation. While myoepithelioma is a well-defined entity in the salivary gland, soft tissue myoepithelioma has recently been recognized. It is usually found in adults and occurs in a wide range of locations, including distal and proximal extremities, trunk, head, and neck.1 Histologically, the tumors are composed of myoepithelial cells showing epithelioid, plasmacytoid, clear cell, and spindle cell morphology in myxoid or fibrous stroma.2,3 To our knowledge, no cytologic findings of soft tissue myoepithelioma have been reported in the literature. We describe the imprint cytologic features of soft tissue myoepithelioma arising in the right forearm of an 18-year-old-man.
CASE REPORT
An 18-year-old man presented with a soft tissue mass of five months' duration in the right forearm. There was no trauma history. Physical examination revealed a round, tender mass. On magnetic resonance scan of the right forearm, T1-weighted imaging revealed a circumscribed mass with intermediate signal intensity. T2-weighted imaging revealed high signal intensity within the mass (Fig. 1A, B). Gadolinium-enhanced fat-suppressed T1-weighted imaging of the mass showed inhomogeneous enhancement. There was no bony involvement. The initial clinical impression was schwannoma. The mass was excised and imprint cytology of the mass was performed.
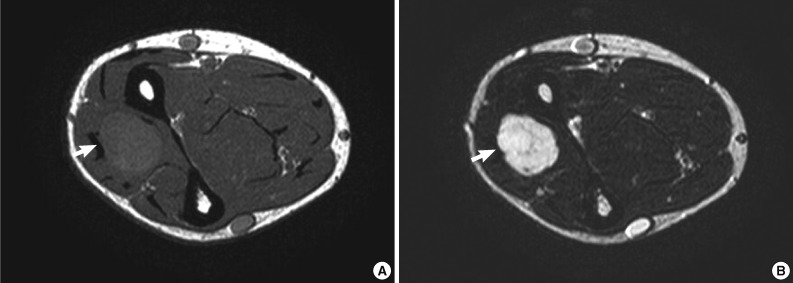
Magnetic resonance images of the right forearm. (A) An intermediate signal mass is present in the right forearm on axial T1-weighted image (arrow). (B) The mass shows a high signal intensity on axial T2-weighted image (arrow).
The obtained slides were stained with hematoxylin and eosin and Papanicolaou methods. On microscopic examination, the smears were moderately cellular. The smear revealed clusters, sheets, and isolated cells in the background of myxoid materials (Fig. 2A-E). Tissue fragments were occasionally scattered. The cells were round to spindle and epithelioid-shaped. The nuclei were uniformly round to ovoid, with finely distributed chromatin and a small nucleolus. The nuclear membrane was smooth. The cytoplasmic borders were well-defined or indistinct. The tumor cells had abundant eosinophilic or pale cytoplasm. Some cells had eccentrically-located nuclei and lesser amount of basophilic cytoplasm, resulting in a plasmacytoid appearance. Long, tapering cytoplasmic processes were also seen. Cytoplasmic vacuolation was noted in some tumor cells. Cells with naked nuclei were also present. Fibrillary materials were occasionally seen in the background. No nuclear pleomorphism was present. Neither mitosis nor necrosis was found. On immunohistochemical staining for cytologic slides, the tumor cells were occasionally positive for cytokeratin (AE1/AE3) and S100 protein.
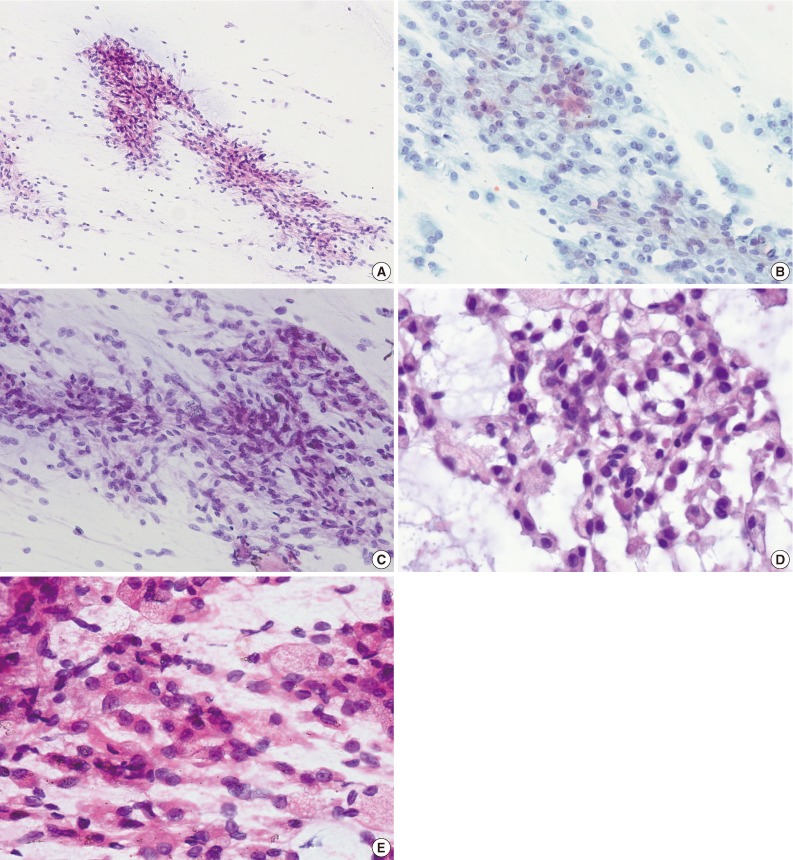
Cytologic findings. (A) The smears are moderately cellular. The tumor cells are present in clusters, sheets and isolated cells in myxoid background. (B) The tumor cells have uniformly round and oval nuclei with finely distributed chromatin and a small nucleolus (Papanicolaou stain). (C) Spindle cells are arranged in clusters. (D) The cells have eccentrically displaced nuclei with basophilic or vacuolated cytoplasm. (E) Epithelioid cells with abundant eosinophilic cytoplasm are present.
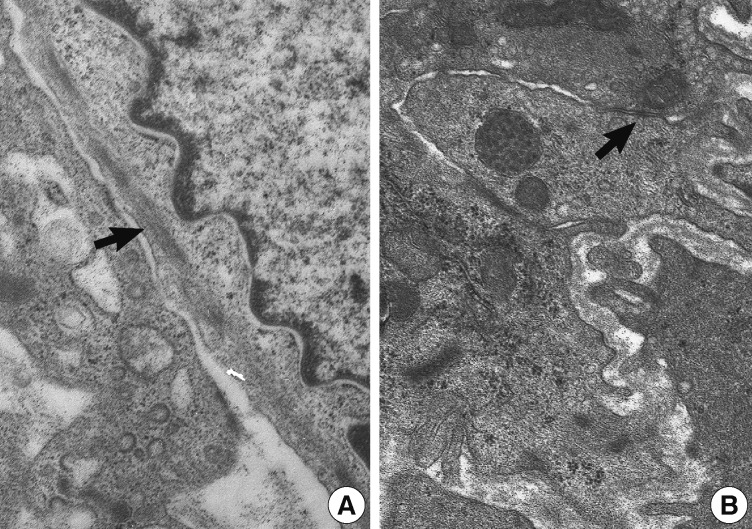
The excised tumor measured 3.0×1.8×1.5 cm. The tumor was well-demarcated, yellow solid, soft, and myxoid (Fig. 3). Histologically, the tumor showed multilobulated growth with myxoid and fibrous stroma. The tumor consisted of epithelioid, spindle and plasmacytoid cells (Fig. 4A, B). The tumor cells were present in solid sheets or reticular pattern without ductal component or necrosis. The tumor cells showed immunostaining for cytokeratin (AE1/AE3), epithelial membrane antigen (EMA), S100 protein, and glial fibrillary acidic protein (GFAP) (Fig. 4C, D). Electron microscopic examination showed intermediate filaments, desmosomes, and basal lamina (Fig. 5). The histologic features were consistent with soft tissue myoepithelioma. Neither recurrence nor metastasis was noted four year follow-up.
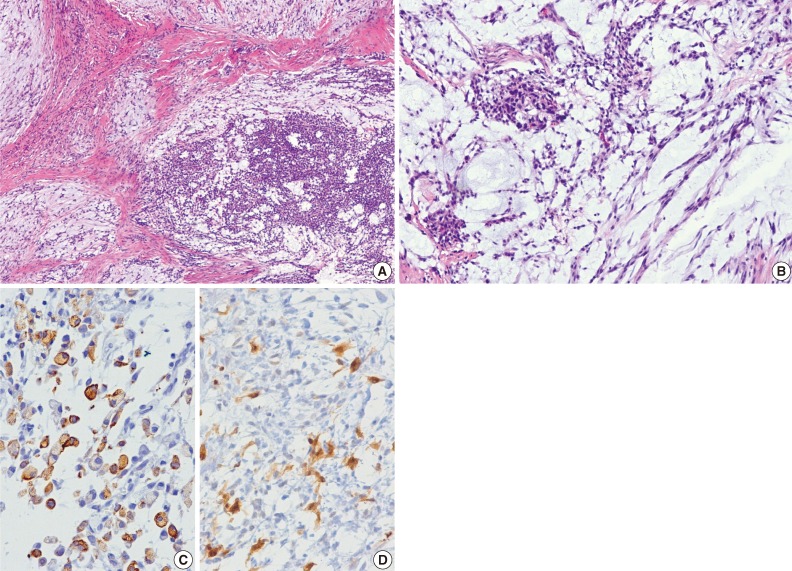
Histologic findings. (A) At low power, the tumor shows lobular architecture in myxoid and fibrous stroma. (B) The tumor cells are arranged in reticular pattern and solid nests. (C, D) The tumor cells show positivity for cytokeratin (AE1/AE3) (C) and S100 protein (D).
DISCUSSION
Soft tissue myoepithelioma is a rare tumor composed of neoplastic cells with features of myoepithelial differentiation. The tumor presents as a painless or painful mass in the dermis, subcutis, or deep soft tissue.3,4 While most myoepitheliomas are of salivary gland origin, they have been reported in the soft tissue, retroperitoneum,3 lung,5 and testis.6 The histogenesis of myoepithelial tumors arising in soft tissue is unknown. It likely reflects a different pattern of gene expression during oncogenesis rather than origin of a specific cell lineage.7 Hallor et al.8 reported that a minimally deleted region of 3.55 Mb at chromosome band 19p13 was identified in soft tissue myoepitheliomas. In the present case, the tumor consisted of epithelioid, spindle, and plasmacytoid cells forming solid sheets or reticular pattern in myxoid and fibrous stroma. The tumor cells revealed positive reaction for cytokeratin (AE1/AE3), EMA, S100 protein, and GFAP. The cytomorphologic and immunohistochemical features of the present case are similar to those of myoepitheliomas arising in the salivary gland.9-12
Soft tissue myoepitheliomas, mixed tumors, and parachordomas are on the spectrum of tumor showing myoepithelial differentiation.1 Characteristically, mixed tumor has more pronounced ductal differentiation, while parachordoma shows prominent cytoplasmic vacuolation. In the present case, the tumor had no ductal component and no cytoplasmic vacuolation. Ultrastructurally, myoepitheliomas show intermediate filaments, desmosomes, and basal lamina.13 Intermediate filaments, desmosomes, and basal lamina were present in this case.
Soft tissue myoepitheliomas may be mistaken as other type of soft tissue tumors due to their cytomorphologically heterogeneous features. The differential diagnosis of soft tissue myoepithelioma includes mixed tumor, parachrodoma, schwannoma, smooth muscle tumor, ossifying fibromyxoid tumor (OFMT), myxoid liposarcoma, extraskeletal myxoid chondrosarcoma (EMC), and metastatic carcinoma. Mixed tumor of soft tissue is uncommon. It shows epithelial and myoepithelial cells in chondromyxoid background. In addition, acinar or duct-like arrangement usually present. Parachordoma shows spindle to epithelioid cells, with clear, vacuolated cytoplasm. Immunohistochemically, parachordomas are positive for cytokeratin and S100 protein.14 Schwannoma has wavy, point-ended nuclei in collagenous or myxoid background and nuclear palisading.15 Smooth muscle tumor has cigar-shaped, blunt-ended nuclei and eosinophilic fibrillary cytoplasm.16 Conversely, the cells of soft tissue myoepithlioma have more tapered nuclei. Immunoreactivity for smooth muscle actin, desmin, and h-caldesmon supports a diagnosis of smooth muscle tumor. OFMT shows round and ovoid cells in myxoid matrix.17 OFMT is immunoreactive for S100 protein in approximately 70% of cases but negative for cytokeratin and GFAP. Myxoid liposarcoma shows lipoblasts and delicate, arborizing, thin-walled blood vessels in myxoid background.18 EMC is characterized by spindle, stellate, or round cells in a myxoid or chondromyxoid matrix and shows variable immunoreactivity for S100 protein, neuron-specific enolase, and synaptophysin.19,20 Generally, metastatic carcinomas show epithelial tumor cells with hyperchromatic nuclei, prominent nucleoli, and a high nuclear to cytoplasmic ratio. It can be excluded by the absence of immunoreactivity for S100 protein and myogenic markers. Immunohistochemical expression for epithelial markers (cytokeratin and/or EMA), S100 protein or GFAP is useful for confirmation of myoepithelial differentiation.3,7
Although most cases of myoepithelial neoplasms of soft tissue are benign, approximate 20% have a risk for local recurrence.3 The histopathologic criteria for malignancy in soft tissue myoepithelial neoplasms are moderate to severe cytologic atypia, increase of nuclear to cytoplasmic ratio, nuclear pleomorphism, and readily identifiable nucleoli.2,3 No cytologic features of malignancy were present in this case of myoepithelioma. The treatment is complete surgical excision with a clear margin.
In conclusion, recognition of the cytomorphologic features of soft tissue myoepithelioma is necessary for the correct cytological diagnosis. Soft tissue myoepithelioma should be included in the differential diagnosis of soft tissue epithelioid and spindle cell neoplasms.
Notes
No potential conflict of interest relevant to this article was reported.