Peritoneal and Nodal Gliomatosis with Endometriosis, Accompanied with Ovarian Immature Teratoma: A Case Study and Literature Review
Article information
Abstract
Gliomatosis peritonei (GP) indicates the peritoneal implantation of mature neuroglial tissue and is usually accompanied by ovarian mature or immature teratoma. Here, we report a case of ovarian immature teratoma associated with gliomatosis involving the peritoneum, lymph nodes and Douglas' pouch, where gliomatosis coexisted with endometriosis. As far as we know, only seven cases of GP have been reported as coexisting with endometriosis. Eight cases with mature glial tissue in the lymph nodes, i.e., nodal gliomatosis, have been published either in association with GP or in its absence. Metaplasia of pluripotent coelomic stem cells has been suggested to be responsible for the pathogenesis of endometriosis and GP rather than implantation metastases of ovarian teratomatous tumor with varying maturation. This theory is also applied to GP independently of ovarian teratomatous tumors. To the best of our knowledge, nodal gliomatosis coexisting with GP and also involving endometriosis has not yet been reported.
Gliomatosis peritonei (GP) was first described in 1905 as a condition of mature glial nodular implants on the peritoneum and omentum associated with ovarian teratoma.1 To date, approximately 100 cases have been described in the literature. Eight cases with glial tissue in the pelvic and paraaortic lymph nodes, i.e., nodal gliomatosis, have been reported either in association with GP or in its absence.1-8 GP may coexist with endometriosis.9-15 Both nodal and peritoneal gliomatosis are benign conditions that require no adjuvant therapy. However, because they mimic peritoneal dissemination of malignancies, awareness of these conditions is important.
Here, we discuss unresolved pathogenesis of this rare coexisting endometriosis and gliomatosis involving the peritoneum and lymph nodes along with a brief review.
CASE REPORT
A 34-year-old female (G2P2A0L2) visited our hospital with an eight-month history of a palpable abdominal mass. She had a history of two cesarean sections. Normal beta-human chorionic gonadotropin with increased alpha-fetoprotein (22.7 ng/mL), cancer antigen (CA) 125 (61.7 U/mL), and CA19-9 (553.7 U/mL) were observed. Contrast-enhanced computed tomography showed a large solid and cystic mass in the left lower abdomen and pelvis. A huge left ovarian tumor filling the peritoneal cavity was found during laparotomy, and yellow-colored ascites (200 mL) was expelled. The external surface of the tumor was pinkish-tan, transparent, smooth, and intact. No pelvic adhesions were observed. Multiple firm, gray-white nodules measuring 0.1 to 0.3 cm were observed on the omentum, uterine serosa and posterior cul-de-sac peritoneum. One surface hemorrhagic nodule that measured 0.3 cm was found on the right ovary. Left salpingo-oophorectomy, right wedge resection, partial omentectomy, and biopsy of the uterine serosal nodules were performed. Under the impression of ovarian malignant tumor, intraoperative frozen biopsies were taken from the omental nodules, left ovary and salpinx. For staging, pelvic lymph node sampling, partial omentectomy and posterior cul-de-sac peritoneal resection were performed.
Grossly, the excised left ovarian mass measured 21.0 cm in diameter and weighed 2,350 g. A predominantly solid mass with multicystic changes, which were filled with clear watery fluid, was observed on the cut surface (Fig. 1A). Thirty sections were taken from the ovarian tumor, and various mature tissues of tridermal lineage were demonstrated (Fig. 1B); the mass was comprised predominantly of mature glial tissue (90%) with focal immature neuroepithelial cells forming rosette-like structures with few mitosis (Fig. 1C). Some mature neurons were also observed within the glial tissue. Choroid plexuses were also found. These immature neuroectodermal foci, including primitive mesenchyma, led to the diagnosis of an immature teratoma, grade 1, according to the classification of Robboy and Scully.3 There were no other germ cell tumor components, including a yolk sac tumor. The peritoneum, cul-de-sac and uterine serosa, as well as the opposite ovarian surface, showed involvement of glial peritonei (grade 0). Nodules of the right ovary, peritoneum and omentum were composed of glial tissue (grade 0) (Fig. 1D). Out of 32 dissected lymph nodes, one left hypogastric lymph node showed one mature glial implant, i.e., nodal gliomatosis (grade 0) (Fig. 1D, inset). Endometrial glands with stromata were found within the peritoneal nodules (Fig. 1E). Some scattered psammoma bodies were observed in peritoneal and nodal gliomatosis, as well as brain tissue in the ovarian immature teratoma. Immunohistochemically, glial fibrillary acidic protein (prediluted, polyclonal, Dako, Glostrup, Denmark) (Fig. 1F, left) immunostaining confirmed the glial nature of the tissue. The endometrial stroma of endometriosis was stained with CD10 (56C6, prediluted, Dako) (Fig. 1F, right).
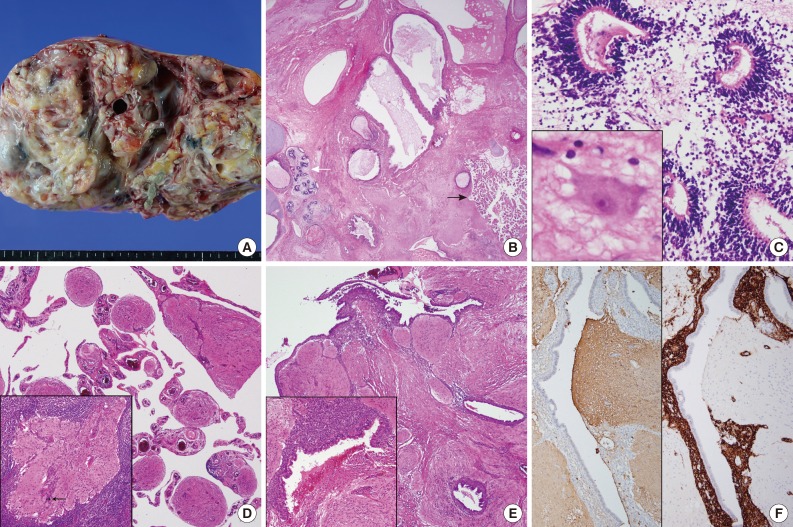
(A) The cut surface of the resected ovary is multilocular cystic and has a solid appearance. (B) The majority of the tumor is composed of mature glial tissue and some intestinal and respiratory epithelia beneath the skin as well as mature hyaline cartilage. Note the choroid plexuses (black arrow) and a few primitive neuroectodermal components (white arrow). (C) Primitive neural tissues are seen in the glial tissue. Inset indicates mature neurons. (D) Mature glial tissue is seen in the omental nodules. Inset indicates a focus of glial tissue in the lymph node. Note psammoma bodies (arrow). (E) Endometriotic glands with stroma, as well as hemosiderin-laden macrophages, are located adjacent to peritoneal glial implants. (F) Mature glial tissue is highlighted with glial fibrillary acidic protein immunostain (left), while the endometrial stroma is stained with CD10 immunostain (right).
Three cycles of chemotherapy of bleomycin, etoposide and cisplatin (BEP) were performed. After the surgery, alpha-fetoprotein, CA125, and CA19-9 levels reached the normal range. During the nine-month post-operative follow-up period, the patient had an uneventful course.
DISCUSSION
GP is a rarely encountered complication of ovarian teratomas and is characterized by peritoneal implants of glial tissue usually of a low World Health Organization grade, although cases of malignant evolution or high grades have also been described.16 About 100 cases have been retrieved in the literature. To our best knowledge, nine cases of nodal gliomatosis (including the present case) were demonstrated in the pelvic or paraaortic lymph nodes;1-8 eight cases were associated with both GP and ovarian teratomatous tumors, while the remaining case was without GP.6 Another interesting phenomenon is the rare combination of GP and endometriosis, as was seen in the present case. To date, seven cases of endometriosis combined with GP have been published in the world literature.9-15 A summary of peritoneal gliomatosis coexisting with nodal gliomatosis or endometriosis is shown in Tables 1 and 2.
The pathogenesis of GP is not yet completely understood. Lymphangeneous glial implants or direct spillage of the glial foci of an ovarian teratoma have been suggested by the previous articles.2-7 Another viewpoint proposed that GP is a metastasis of glial tissue to a focus of pre-existing endometriosis because these endometrial foci are more vascular and therefore are more receptive. However, this concept contradicts the fact that endometriosis is rare in the pediatric population, and it is unlikely because despite extensive sampling, there were only mixed endometrial and glial cells but no pure endometriosis. The pathogenesis of endometriosis and GP may be shared. Originally, the presence of GP indicated that these lesions were shared by implantation metastases of an ovarian teratomatous tumor with varying maturation.7,10-12 Metaplasia of pluripotent coelomic or Mullerian stem cells has also been suggested, but the most scientifically supported and widely accepted mechanism of endometriosis is retrograde effluent flow through the lumen of the fallopian tubes into the pelvic-peritoneal cavities during menstruation.9 Metaplasia may be induced by unknown stimuli in other uncommon peritoneal lesions, such as melanosis peritonei, etc.17 Dworak et al.11 suggested that GP temporally predisposes a patient to the development of endometriosis. A recent assay for loss of heterozygosity revealed that normal tissues and GP showed a heterozygous pattern in the microsatellite loci, whereas the associated ovarian teratomas had a homozygous pattern.18 These findings suggest that GP with or without nodal involvement is genetically unrelated to the associated teratoma but may be stimulated by these teratomas. Other rare locations such as intrathoracic gliomatosis, isolated GP independent to ovarian teratoma or one occurring after ventriculoperitoneal shunt operations also support this theory. The peritoneal mesothelium that modulates the cytoskeleton and shape is explained as subserosal multipotential subserosal cells that can replicate and differentiate diversely under unspecified stimuli.19 Mesothelial hyperplasia is commonly found when it is stimulated by pleural and peritoneal effusion.19 This mesothelial hyperplasia may be rarely seen in lymph nodes, and in these cases it would be mimicking metastatic tumors.18 Gliomatosis affecting the lymph node can be explained by this unusual location of mesothelial hyperplasia, although the present case showed no peritoneal mesothelial hyperplasia. A frequent association between GP and effusion was found; about 35 cases of GP were accompanied by ascites, and 3 cases involved pleural effusion.1,4,6,8 The frequent association with ascites or pleural effusion and co-existing nodal or GP, as shown in Table 1, may provide supporting evidence of this unusual location of gliomatosis.1,19 However, although the common association of GP with ovarian teratoma is indisputable, the reason why subperitoneal cells develop into glial islands in the presence of these ovarian tumors remains to be investigated. Another explanation of the occasionally present ascites or pleural effusion is that the pressure on the lymphatics in the tumor of the peritoneum as well as the ovary causes the fluid to escape through the superficial lymphatic vessels of the tumor or induces increased vascular permeability.19
Clinically, intraoperatively encountered widespread, grayish tan-colored, firm, tiny nodules can be mistaken as peritoneal carcinomatosis or disseminated tuberculosis, especially in cases showing calcification or psammoma bodies like the present patient.10,11 Despite the rarity of ovarian immature teratomas with GP data and limitations, the prognosis of GP has long been regarded as good compared to that of immature teratoma without GP.14 However, the application of cisplatin-based chemotherapy regimens has dramatically improved the prognosis of immature teratomas of high grades and stages.16 Recent studies suggested that the poor prognosis in immature teratoma is correlated with incomplete resection, tumor rupture, younger age, higher stage and grade, and GP, but not with cyst spillage, enucleation, nodal gliomatosis, or microfoci of yolk sac tumor, i.e., Heifetz lesions.16
To the best of our knowledge, peritoneal and nodal gliomatosis as well as combined endometriosis are rare phenomena that have not yet been described in the English literature.
Notes
No potential conflict of interest relevant to this article was reported.

