Search
- Page Path
- HOME > Search
Original Article
- Upward trend in follicular lymphoma among the Korean population: 10-year experience at a large tertiary institution
- Meejeong Kim, Hee Sang Hwang, Hyungwoo Cho, Dok Hyun Yoon, Cheolwon Suh, Chan Sik Park, Heounjeong Go, Jooryung Huh
- J Pathol Transl Med. 2021;55(5):330-337. Published online September 2, 2021
- DOI: https://doi.org/10.4132/jptm.2021.07.25
- 7,061 View
- 125 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Follicular lymphoma (FL) is the second most common non-Hodgkin lymphoma (NHL) in Western countries. However, it is relatively rare in Asia. This study examined epidemiologic characteristics of FL in South Korea, with an emphasis on recent trends of increase in cases.
Methods
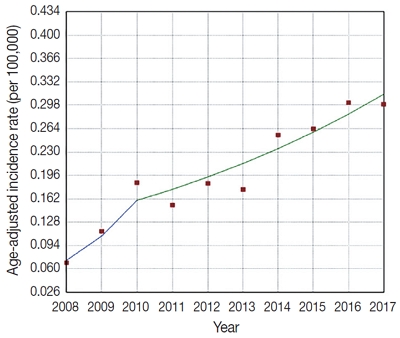
We retrospectively examined 239 cases of newly diagnosed FL at a large tertiary institution in Korea (Asan Medical Center, Seoul, Republic of Korea) between 2008 and 2017. Age-adjusted incidence rates and clinicopathological variables were analyzed, and joinpoint regression analysis was used to identify the changes.
Results
The age-adjusted incidence of FL significantly increased during the study period (p = .034), and the ratio of (relative incidence) patients with FL to patients with NHL increased from 4.28% to 9.35% in the same period. Over the 10-year study assessment duration, the proportion of patients with stage III/IV FL (p = .035) and expression of BCL2 (p = .022) or BCL6 (p = .039) significantly increased. From 2013–2017, the proportion of patients with highrisk Follicular Lymphoma International Prognostic Index (FLIPI) score increased (21.5% to 28.7%), whereas that of low-risk FLIPI decreased (55.4% to 38.6%), although those results were not statistically significant (p = .066).
Conclusions
We found an increasing incidence of FL, with a disproportionate increase in the incidence of high-stage disease and recent changes in the clinicopathologic features of the Korean patient population. -
Citations
Citations to this article as recorded by- Incidence Trend of Follicular Lymphoma in Taiwan Compared to Japan and Korea, 2001–2019
Liang-Chun Chiu, Chih-Wen Lin, Hung-Ju Li, Jian-Han Chen, Fu-Cheng Chuang, Sheng-Fung Lin, Yu Chang, Yu-Chieh Su
Journal of Clinical Medicine.2023; 12(4): 1417. CrossRef - A Case Report on the Complete Response of a Patient with Recurrent Follicular Lymphoma Treated with Integrative Medicine
Kyung-dug Park, Jisoo Kim, Yoona Oh, Beom-Jin Jeong, Yu-jin Jung, Sunhwi Bang
The Journal of Internal Korean Medicine.2023; 44(3): 585. CrossRef - Recent Updates on Diagnosis and Treatment of Follicular Lymphoma
Ga-Young Song, Deok-Hwan Yang
The Korean Journal of Medicine.2023; 98(5): 231. CrossRef - Classical Hodgkin lymphoma following follicular lymphoma: a case report
Bomi Kim
Journal of Yeungnam Medical Science.2023; 40(Suppl): S113. CrossRef - Incidence, clinicopathological features and genetics of in‐situ follicular neoplasia: a comprehensive screening study in a Japanese cohort
Naoki Oishi, Takahiro Segawa, Kunio Miyake, Kunio Mochizuki, Tetsuo Kondo
Histopathology.2022; 80(5): 820. CrossRef
- Incidence Trend of Follicular Lymphoma in Taiwan Compared to Japan and Korea, 2001–2019
Brief Case Report
- A Case of Type II Enteropathy-Associated T-Cell Lymphoma with Epstein-Barr Virus Positivity
- Min Jeong Song, Chan Sik Park, Hee Sang Hwang, Cheol Won Suh, Dok Hyun Yoon, Jooryung Huh
- Korean J Pathol. 2014;48(6):426-429. Published online December 31, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.6.426
- 10,409 View
- 52 Download
- 5 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Various Endoscopic Features in Monomorphic Epitheliotropic Intestinal T-Cell Lymphoma
Yasuhiro Aoki, Tomohisa Sujino, Kaoru Takabayashi, Makoto Mutakuchi, Katsura Emoto, Naoki Hosoe, Haruhiko Ogata, Takanori Kanai
Case Reports in Gastroenterology.2021; 15(1): 312. CrossRef - A viral map of gastrointestinal cancers
Natália R. Costa, Rui M. Gil da Costa, Rui Medeiros
Life Sciences.2018; 199: 188. CrossRef - Type II Enteropathy-Associated T-cell Lymphoma: A Rare Report from Iran
Neda Nozari
Middle East Journal of Digestive Diseases.2017; 9(1): 55. CrossRef - Unusual Cause of Dysphagia
Shahram Agah, Ramak Ghavam, Ahmad Darvishi Zeidabadi, Arash Sarveazad
Middle East Journal of Digestive Diseases.2017; 9(1): 58. CrossRef - Multiple lesions of gastrointestinal tract invasion by monomorphic epitheliotropic intestinal T-cell lymphoma, accompanied by duodenal and intestinal enteropathy-like lesions and microscopic lymphocytic proctocolitis: a case series
Hideki Ishibashi, Satoshi Nimura, Yoshiyuki Kayashima, Yasushi Takamatsu, Kunihiko Aoyagi, Naohiko Harada, Masanori Kadowaki, Takihiko Kamio, Shotaro Sakisaka, Morishige Takeshita
Diagnostic Pathology.2016;[Epub] CrossRef
- Various Endoscopic Features in Monomorphic Epitheliotropic Intestinal T-Cell Lymphoma
Case Report
- Fine Needle Aspiration Cytology of Osteoclast-like Giant Cell Tumor of the Liver: A Case Report .
- Chan Sik Park, Ji Eun Kim, Mee Soo Chang
- J Pathol Transl Med. 1999;10(1):79-84.
- 1,998 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Osteoclast-like giant cell tumor of the liver is an extremely rare malignancy with poor prognosis. To our knowledge, 5 cases have been reported in English literatures, but there was no report about fine needle aspiration cytologic(FNAC) features. We experienced a case of osteoclast-like giant cell tumor of the liver obtained by computed tomography(CT)-guided FNAC and needle biopsy. The cytologic findings mimicked giant cell tumor of the bone. A large hepatic mass of the left lobe with abdominal wall invasion was found by CT in a 46-year-old female complaining of epigastric pain. The FNAC showed moderately cellular smears consisting of osteoclast-like giant cells and mononuclear cells, which were individually scattered or intermingled in clusters. The osteoclast-like giant cells had abundant cytoplasms and multiple small round nuclei with fine chromatin and distinct nucleoli. The mononuclear cells had moderate amount of cytoplasm and relatively bland-looking oval nuclei with single small nucleoli. All of the cytologic features recapitulated the histologic findings of bland-looking osteoclast-like multinucleated giant cells evenly dispersed throughout the background of mononuclear cell. The immunohistochemical study showed positive reaction for CD68 and vimentin, but negative for cytokeratin in both osteoclast-like giant cells and mononuclear cells.
Original Articles
- The Increased Expression and Diagnostic Usefulness of CD56 Antigen in Paraffin Embedded Plasma Cell Neoplasm.
- Seok Hyung Kim, Chan Sik Park, Eun Young Choi, Hyun Wook Kang, Seong Hoe Park, Doo Hyun Chung
- Korean J Pathol. 2001;35(3):201-205.
- 2,431 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The natural killer cell antigen CD56 (NCAM) is a member of the immunoglobulin superfamily and is expressed on neurons, astrocytes, and Schwann cells. Recently, it has been reported that CD56 expression is detected on plasma cells of multiple myeloma by flow cytometry.
METHOD
In this study, to test the diagnostic usefulness of the anti-CD56 antibody for plasma cell neoplasm on paraffin-embedded materials, we performed immunohistochemical staining of samples from 19 patients with plasma cell neoplasms. These cases included 14 cases of multiple myeloma, 3 cases of solitary plasmacytoma of the bone, and two cases of extramedullary plasmacytoma.
RESULTS
The neoplastic plasma cells from 68 % of the patients with plasma cell neoplasms expressed CD56 highly. CD56 was expressed in all three cases of solitary plasmacytoma of the bone and one of two extramedullary plasmacytoma, and nine out of 14 multiple myeloma cases. In contrast, reactive plasma cells from the 18 patients with miscellaneous lesions were completely negative for CD56.
CONCLUSIONS
CD56 is aberrantly expressed on the neoplastic plasma cells, and it may be used as a useful marker for the diagnosis of plasma cell neoplasms in paraffin-embedded tissues.
- Expression Pattern of the Cortical Immature Thymocyte Specific Antigen JL1 in Thymomas; a New Adjunctive Diagnostic Marker.
- Young Soo Park, Youngji Kim, Yun Hee Lee, Joo Ryung Huh, Chan Sik Park
- Korean J Pathol. 2008;42(5):251-259.
- 2,310 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
JL1 is a novel antigen that has been reported to be expressed exclusively in immature CD4 CD8 double positive T-cells in the thymic cortex. Thymomas are often infiltrated with lymphocytes that are mostly immature T-cells. METHODS: We evaluated 67 cases of surgically resected thymomas and reviewed their histological, surgical, and clinical findings. Representative sections were immunostained using anti-JL1 monoclonal antibody and the immunostaining score was evaluated in each case. RESULTS: JL1 was strongly positive in immature T cells infiltrated in various subtypes of thymomas. The mean value of the immunostaining score was 0 for type A, 0.24 for the A areas of type AB, 2.71 for the B areas of type AB, 3 for type B1, 1.87 for type B2, 0.67 for type B3, and 0.13 for type C. The immunostaining score correlated with the histological subtypes according to the WHO classification, and stages according to the modified Masaoka system. CONCLUSION: JL1 was specifically detected in immature thymocytes in thymomas. Therefore, JL1 immunostaining can be useful for subtyping thymomas. JL1 can also serve as an adjunctive marker to diagnose thymomas in small biopsy specimens.
- Diagnostic Usefulness of Monoclonal Antibody for T Lymphoblastic Lymphoma/Acute Lymphoblastic Leukemia-Specific JL1 Antigen in Paraffin Embedded Tissue.
- Chan Sik Park, Seong Hoe Park
- Korean J Pathol. 1999;33(11):1033-1038.
- 2,030 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - JL1 is a novel human thymocyte differentiation antigen, which is exclusively expressed by double positive (CD4+ CD8+) cortical thymocytes. We previously reported that the JL1 antigen was selectively expressed on the surface of acute lymphoblastic leukemia cells. T-Lymphoblastic lymphoma/acute lymphoblastic leukemia (T-LBL/ALL), the 6th prevalent lymphoma in Korea, is composed of immature neoplastic lymphoid cells and shows a rapid response to appropriate treatment. Early and precise diagnosis of LBL/ALL is crucial. Light microscopic distinction of LBL/ALL from other non-Hodgkin's lymphomas can sometimes be difficult and is aided by immunophenotypic studies. This study is designed to investigate the diagnostic utility of anti-JL1 monoclonal antibody (YG5) for LBL/ALL in formalin fixed, paraffin embedded tissue. We collected 25 cases of LBL/ALL (18 T-cell, 5 B-cell and 2 undetermined lineage) from 1993 through 1998. We confirmed the diagnosis using morphologic and immunophenotypic data. Strong JL1 expression along cell membrane was observed in 16 out of 18 T-LBL/ALL cases (89%). In 28 cases of other types of lymphomas of including 7 cases of non-T LBL/ALL and 14 cases of small round cell tumors, no JL1 expression was identified. These results show that the immunostaining for JL1 using YG5 on paraffin embedded sections can be useful for the specific diagnosis of T-LBL/ALL in routine diagnostic service.
- Pathologic Analysis of 2159 Cases of Appendix.
- Chan Sik Park, Mee Soo Chang, In Ae Park, Yong Il Kim, Gheeyoung Choe
- Korean J Pathol. 2000;34(1):39-49.
- 2,786 View
- 49 Download
-
 Abstract
Abstract
 PDF
PDF - We reviewed 2159 consecutive cases of surgically resected appendices. The appendectomy specimen consisted of 91 cases of acute focal appendicitis (5.4%), 926 cases of acute suppurative appendicitis (55.1%), 228 cases of acute gangrenous appendicitis (13.6%), 63 cases of periappendicitis (3.8%), 13 cases of pure fibrous obliteration of the lumen (FOL; 0.8%), 18 cases of other diseases (7 mucoceles, 2 mucinous cystic neoplasms, 4 carcinoids, 2 metastatic carcinomas, 2 tuberculous appendicitides, and 1 eosinophilic appendicitis; 1%), and 342 cases with no diagnostic abnormality (20.3%). Patients having acute appendicitis ranged from 3 to 84 years of age, and patients in their 10's and 20's occupied over half of 2159 cases. Diagnostic accuracy of the acute appendicitis was 79.7%. Incidence of the acute appendicitis was suspected to be 7.2/100,000/year. Twenty eight cases of acute appendicitis were associated with diverticula. In the former acute primary diverticulitis led to acute appendicitis in 14 of 28 cases. Among 478 incidental appendectomy cases, there were 3 acute focal appendicitides, 1 acute suppurative appendicitis, 1 eosinophilic appendicitis, 32 periappendicitides, 1 mucocele, 40 pure FOLs, 1 deciduosis, 1 endometriosis, and 1 diverticulosis without inflammation. There were 69 cases of FOL (32 complete forms and 37 incomplete forms), among which 13 cases were associated with acute appendicitis. FOL was more frequent in female patients as well as patients over 40 years of age. Incomplete FOL was considered to progress to complete form with age. The incidence of appendiceal diverticula was higher, whereas the incidences of carcinoid tumor and FOL were lower compared with that in the western report. In 14 of 28 cases the appendiceal diverticulum was the site in which acute appendicitis began.

 E-submission
E-submission

 First
First Prev
Prev



