Search
- Page Path
- HOME > Search
Original Article
- Categorizing high-grade serous ovarian carcinoma into clinically relevant subgroups using deep learning–based histomic clusters
- Byungsoo Ahn, Eunhyang Park
- J Pathol Transl Med. 2025;59(2):91-104. Published online February 18, 2025
- DOI: https://doi.org/10.4132/jptm.2024.10.23
- 5,029 View
- 248 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
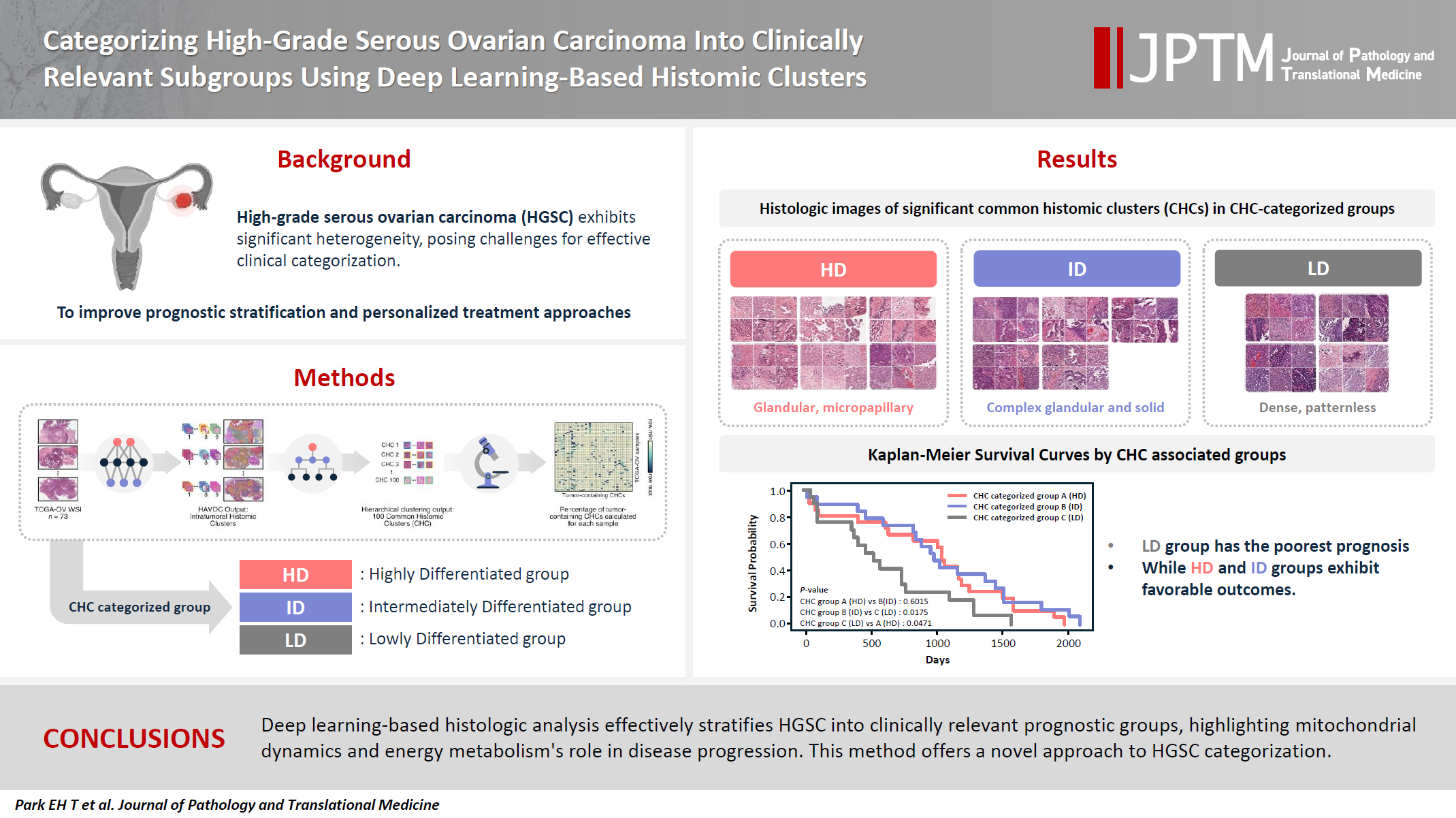
Supplementary Material - Background
High-grade serous ovarian carcinoma (HGSC) exhibits significant heterogeneity, posing challenges for effective clinical categorization. Understanding the histomorphological diversity within HGSC could lead to improved prognostic stratification and personalized treatment approaches. Methods: We applied the Histomic Atlases of Variation Of Cancers model to whole slide images from The Cancer Genome Atlas dataset for ovarian cancer. Histologically distinct tumor clones were grouped into common histomic clusters. Principal component analysis and K-means clustering classified HGSC samples into three groups: highly differentiated (HD), intermediately differentiated (ID), and lowly differentiated (LD). Results: HD tumors showed diverse patterns, lower densities, and stronger eosin staining. ID tumors had intermediate densities and balanced staining, while LD tumors were dense, patternless, and strongly hematoxylin-stained. RNA sequencing revealed distinct patterns in mitochondrial oxidative phosphorylation and energy metabolism, with upregulation in the HD, downregulation in the LD, and the ID positioned in between. Survival analysis showed significantly lower overall survival for the LD compared to the HD and ID, underscoring the critical role of mitochondrial dynamics and energy metabolism in HGSC progression. Conclusions: Deep learning-based histologic analysis effectively stratifies HGSC into clinically relevant prognostic groups, highlighting the role of mitochondrial dynamics and energy metabolism in disease progression. This method offers a novel approach to HGSC categorization. -
Citations
Citations to this article as recorded by- Learning Disabilities in the 21st Century: Integrating Neuroscience, Education, and Technology for Better Outcomes
Syed Mohammed Basheeruddin Asdaq, Ahmad H. Alhowail, Syed Imam Rabbani, Naira Nayeem, Syed Mohammed Emaduddin Asdaq, Faiqa Nausheen
SAGE Open.2025;[Epub] CrossRef
- Learning Disabilities in the 21st Century: Integrating Neuroscience, Education, and Technology for Better Outcomes
Brief Case Report
- Osteosarcomatous Differentiation in Rebiopsy Specimens of Pulmonary Adenocarcinoma with EGFR-TKI Resistance
- Hyein Ahn, Hyun Jung Kwon, Eunhyang Park, Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2018;52(2):130-132. Published online April 4, 2017
- DOI: https://doi.org/10.4132/jptm.2016.11.17
- 7,054 View
- 135 Download
- 1 Web of Science
- 1 Crossref
Original Articles
- Aquaporin 1 Is an Independent Marker of Poor Prognosis in Lung Adenocarcinoma
- Sumi Yun, Ping-Li Sun, Yan Jin, Hyojin Kim, Eunhyang Park, Soo Young Park, Kyuho Lee, Kyoungyul Lee, Jin-Haeng Chung
- J Pathol Transl Med. 2016;50(4):251-257. Published online June 7, 2016
- DOI: https://doi.org/10.4132/jptm.2016.03.30
- 11,680 View
- 123 Download
- 25 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Aquaporin 1 (AQP1) overexpression has been shown to be associated with uncontrolled cell replication, invasion, migration, and tumor metastasis. We aimed to evaluate AQP1 expression in lung adenocarcinomas and to examine its association with clinicopathological features and prognostic significance. We also investigated the association between AQP1 overexpression and epithelial-mesenchymal transition (EMT) markers.
Methods
We examined AQP1 expression in 505 cases of surgically resected lung adenocarcinomas acquired at the Seoul National University Bundang Hospital from 2003 to 2012. Expression of AQP1 and EMT-related markers, including Ecadherin and vimentin, were analyzed by immunohistochemistry and tissue microarray.
Results
AQP1 overexpression was associated with several aggressive pathological parameters, including venous invasion, lymphatic invasion, and tumor recurrence. AQP1 overexpression tended to be associated with higher histological grade, advanced pathological stage, and anaplastic lymphoma kinase (ALK) translocation; however, these differences were not statistically significant. In addition, AQP1 overexpression positively correlated with loss of E-cadherin expression and acquired expression of vimentin. Lung adenocarcinoma patients with AQP1 overexpression showed shorter progression- free survival (PFS, 46.1 months vs. 56.2 months) compared to patients without AQP1 overexpression. Multivariate analysis confirmed that AQP1 overexpression was significantly associated with shorter PFS (hazard ratio, 1.429; 95% confidence interval, 1.033 to 1.977; p=.031).
Conclusions
AQP1 overexpression was thereby concluded to be an independent factor of poor prognosis associated with shorter PFS in lung adenocarcinoma. These results suggested that AQP1 overexpression might be considered as a prognostic biomarker of lung adenocarcinoma. -
Citations
Citations to this article as recorded by- The Expanding Role of Aquaporin-1, Aquaporin-3 and Aquaporin-5 as Transceptors: Involvement in Cancer Development and Potential Druggability
Catarina Pimpão, Inês V. da Silva, Graça Soveral
International Journal of Molecular Sciences.2025; 26(3): 1330. CrossRef - The comprehensive potential of AQP1 as a tumor biomarker: evidence from kidney neoplasm cohorts, cell experiments and pan-cancer analysis
Yifan Liu, Donghao Lyu, Yuntao Yao, Jinming Cui, Jiangui Liu, Zikuan Bai, Zihui Zhao, Yuanan Li, Bingnan Lu, Keqin Dong, Xiuwu Pan
Human Genomics.2025;[Epub] CrossRef - The Association of Aquaporins with MAPK Signaling Pathway Unveils Potential Prognostic Biomarkers for Pancreatic Cancer: A Transcriptomics Approach
Inês V. da Silva, Paula A. Lopes, Elisabete Fonseca, Emanuel Vigia, Jorge Paulino, Graça Soveral
Biomolecules.2025; 15(4): 488. CrossRef - Obesity Impacts Post‐Myocardial Infarction Neovascularization by Downregulating AQP1 Expression via the TRPC5‐NFATc3 Signaling Pathway
Mengru Gao, Jing Han, Yifei Zhu, Xin Wen, Lei Feng, Tingting Zhou
Comprehensive Physiology.2025;[Epub] CrossRef - Aquaporin‐1, aquaporin‐3 and aquaporin‐5 differentially modulate cell biophysical and biomechanical properties, impacting cell stiffness and cell–cell adhesion
Catarina Pimpão, Filomena A. Carvalho, Inês Vieira da Silva, Andreia Barateiro, Nuno C. Santos, Graça Soveral
The FEBS Journal.2025;[Epub] CrossRef - Prognostic Assessment of Aquaporins in Pancreatic Adenocarcinoma: An In Silico Analysis
Vignesh Krishnasamy, Lalhmingliana, Nachimuthu Senthil Kumar
Current Biotechnology.2025; 14(2): 130. CrossRef - Clinical application of cold atmospheric-pressure plasma: mechanisms and irradiation conditions
Eun Ji Jeong, Hyun Min Park, Dong Jae Lee, Jun Lee, Jun Yeong Cho, Kyung Deok Seo, Seokjun Je, Min Hyung Jung, Woo Yeon Hwang, Kyung Sook Kim
Journal of Physics D: Applied Physics.2024; 57(37): 373001. CrossRef - Aquaporins in Cancer Biology
Chul So Moon, David Moon, Sung Koo Kang
Frontiers in Oncology.2022;[Epub] CrossRef - A Comprehensive Prognostic Analysis of Tumor-Related Blood Group Antigens in Pan-Cancers Suggests That SEMA7A as a Novel Biomarker in Kidney Renal Clear Cell Carcinoma
Yange Wang, Chenyang Li, Xinlei Qi, Yafei Yao, Lu Zhang, Guosen Zhang, Longxiang Xie, Qiang Wang, Wan Zhu, Xiangqian Guo
International Journal of Molecular Sciences.2022; 23(15): 8799. CrossRef - Differential modulation of lung aquaporins among other pathophysiological markers in acute (Cl2 gas) and chronic (carbon nanoparticles, cigarette smoke) respiratory toxicity mouse models
Sukanta S. Bhattacharya, Brijesh Yadav, Ekta Yadav, Ariel Hus, Niket Yadav, Perminder Kaur, Lauren Rosen, Roman Jandarov, Jagjit S. Yadav
Frontiers in Physiology.2022;[Epub] CrossRef - Aquaporin water channels as regulators of cell-cell adhesion proteins
Sarannya Edamana, Frédéric H. Login, Soichiro Yamada, Tae-Hwan Kwon, Lene N. Nejsum
American Journal of Physiology-Cell Physiology.2021; 320(5): C771. CrossRef - Targeting Aquaporins in Novel Therapies for Male and Female Breast and Reproductive Cancers
Sidra Khan, Carmela Ricciardelli, Andrea J. Yool
Cells.2021; 10(2): 215. CrossRef - Targeting ion channels for the treatment of lung cancer
Liqin Zhang, Shuya Bing, Mo Dong, Xiaoqiu Lu, Yuancheng Xiong
Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.2021; 1876(2): 188629. CrossRef - Comprehensive Analysis of Aquaporin Superfamily in Lung Adenocarcinoma
Guofu Lin, Luyang Chen, Lanlan Lin, Hai Lin, Zhifeng Guo, Yingxuan Xu, Chanchan Hu, Jinglan Fu, Qinhui Lin, Wenhan Chen, Yiming Zeng, Yuan Xu
Frontiers in Molecular Biosciences.2021;[Epub] CrossRef - Diagnostic accuracy of urinary aquaporin-1 as a biomarker for renal cell carcinoma
Abhilash Cheriyan, Arun Jose Nellickal, Nirmal Thampi John, Lakshmanan Jeyaseelan, Santosh Kumar, Antony Devasia, Nitin Kekre
Indian Journal of Urology.2021; 37(1): 59. CrossRef - Aquaporin 1, 3, and 5 Patterns in Salivary Gland Mucoepidermoid Carcinoma: Expression in Surgical Specimens and an In Vitro Pilot Study
Mérin Barbara Stamboni, Ágatha Nagli de Mello Gomes, Milena Monteiro de Souza, Katia Klug Oliveira, Claudia Fabiana Joca Arruda, Fernanda de Paula, Barbara Beltrame Bettim, Márcia Martins Marques, Luiz Paulo Kowalski, Clóvis Antônio Lopes Pinto, Victor El
International Journal of Molecular Sciences.2020; 21(4): 1287. CrossRef - Combined Systematic Review and Transcriptomic Analyses of Mammalian Aquaporin Classes 1 to 10 as Biomarkers and Prognostic Indicators in Diverse Cancers
Pak Hin Chow, Joanne Bowen, Andrea J Yool
Cancers.2020; 12(7): 1911. CrossRef - Aquaporins in lung health and disease: Emerging roles, regulation, and clinical implications
Ekta Yadav, Niket Yadav, Ariel Hus, Jagjit S. Yadav
Respiratory Medicine.2020; 174: 106193. CrossRef - Dissecting gene‐environment interactions: A penalized robust approach accounting for hierarchical structures
Cen Wu, Yu Jiang, Jie Ren, Yuehua Cui, Shuangge Ma
Statistics in Medicine.2018; 37(3): 437. CrossRef - Immunohistochemical Expression of Aquaporin-1 in Fluoro-Edenite-Induced Malignant Mesothelioma: A Preliminary Report
Giuseppe Angelico, Rosario Caltabiano, Carla Loreto, Antonio Ieni, Giovanni Tuccari, Caterina Ledda, Venerando Rapisarda
International Journal of Molecular Sciences.2018; 19(3): 685. CrossRef - Mechanisms of Aquaporin-Facilitated Cancer Invasion and Metastasis
Michael L. De Ieso, Andrea J. Yool
Frontiers in Chemistry.2018;[Epub] CrossRef - Aquaporin 1 suppresses apoptosis and affects prognosis in esophageal squamous cell carcinoma
Yuzo Yamazato, Atsushi Shiozaki, Daisuke Ichikawa, Toshiyuki Kosuga, Katsutoshi Shoda, Tomohiro Arita, Hirotaka Konishi, Shuhei Komatsu, Takeshi Kubota, Hitoshi Fujiwara, Kazuma Okamoto, Mitsuo Kishimoto, Eiichi Konishi, Yoshinori Marunaka, Eigo Otsuji
Oncotarget.2018; 9(52): 29957. CrossRef - Aquaporin 1 expression is associated with response to adjuvant chemotherapy in stage�II and III colorectal cancer
Hideko Imaizumi, Keiichiro Ishibashi, Seiichi Takenoshita, Hideyuki Ishida
Oncology Letters.2018;[Epub] CrossRef - Aquaporin 3 facilitates tumor growth in pancreatic cancer by modulating mTOR signaling
Xunwei Huang, Li Huang, Minhua Shao
Biochemical and Biophysical Research Communications.2017; 486(4): 1097. CrossRef - Prognostic implication of aquaporin 1 overexpression in resected lung adenocarcinoma†
Guido Bellezza, Jacopo Vannucci, Fortunato Bianconi, Giulio Metro, Rachele Del Sordo, Marco Andolfi, Ivana Ferri, Paola Siccu, Vienna Ludovini, Francesco Puma, Angelo Sidoni, Lucio Cagini
Interactive CardioVascular and Thoracic Surgery.2017; 25(6): 856. CrossRef
- The Expanding Role of Aquaporin-1, Aquaporin-3 and Aquaporin-5 as Transceptors: Involvement in Cancer Development and Potential Druggability
- Membranous Insulin-like Growth Factor-1 Receptor (IGF1R) Expression Is Predictive of Poor Prognosis in Patients with Epidermal Growth Factor Receptor (EGFR)-Mutant Lung Adenocarcinoma
- Eunhyang Park, Soo Young Park, Hyojin Kim, Ping-Li Sun, Yan Jin, Suk Ki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
- J Pathol Transl Med. 2015;49(5):382-388. Published online August 4, 2015
- DOI: https://doi.org/10.4132/jptm.2015.07.10
- 11,329 View
- 100 Download
- 23 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Insulin-like growth factor-1 receptor (IGF1R) is a membrane receptor-type tyrosine kinase that has attracted considerable attention as a potential therapeutic target, although its clinical significance in non-small cell lung cancer (NSCLC) is controversial. This study aimed to clarify the clinical significance of IGF1R expression in human NSCLC. Methods: IGF1R protein expression was evaluated using immunohistochemistry in 372 patients with NSCLC who underwent curative surgical resection (146 squamous cell carcinomas [SqCCs] and 226 adenocarcinomas [ADCs]). We then analyzed correlations between expression of IGF1R and clinicopathological and molecular features and prognostic significance. Results: Membranous and cytoplasmic IGF1R expression were significantly higher in SqCCs than in ADCs. In patients with SqCC, membranous IGF1R expression was associated with absence of vascular, lymphatic, and perineural invasion; lower stage; and better progression-free survival (PFS) (hazard ratio [HR], 0.586; p = .040). In patients with ADC, IGF1R expression did not have a significant prognostic value; however, in the subgroup of epidermal growth factor receptor (EGFR)-mutant ADC, membranous IGF1R expression was associated with lymphatic and perineural invasion, solid predominant histology, and higher cancer stage and was significantly associated with worse PFS (HR, 2.582; p = .009). Conclusions: Lung ADC and SqCC showed distinct IGF1R expression profiles that demonstrated prognostic significance. High membranous IGF1R expression was predictive of poor PFS in EGFR-mutant lung ADC, while it was predictive of better PFS in SqCC. These findings will help improve study design for subsequent investigations and select patients for future anti-IGF1R therapy. -
Citations
Citations to this article as recorded by- Expression of Amine Oxidase Proteins in Adrenal Cortical Neoplasm and Pheochromocytoma
Eun Kyung Kim, Ja Seung Koo
Biomedicines.2023; 11(7): 1896. CrossRef - Expression of EMP 1, 2, and 3 in Adrenal Cortical Neoplasm and Pheochromocytoma
Yoon Jin Cha, Ja Seung Koo
International Journal of Molecular Sciences.2023; 24(16): 13016. CrossRef - Clinico-pathological characteristics of IGFR1 and VEGF-A co-expression in early and locally advanced-stage lung adenocarcinoma
Wenting Liu, Junling Xia, Qingwu Du, Jingya Wang, Ting Mei, Tingting Qin
Journal of Cancer Research and Clinical Oncology.2023; 149(18): 16365. CrossRef - NT157 exerts antineoplastic activity by targeting JNK and AXL signaling in lung cancer cells
Lívia Bassani Lins de Miranda, Keli Lima, Juan Luiz Coelho-Silva, Fabiola Traina, Susumu S. Kobayashi, João Agostinho Machado-Neto
Scientific Reports.2022;[Epub] CrossRef - IRS2 Amplification as a Predictive Biomarker in Response to Ceritinib in Small Cell Lung Cancer
Mi-Sook Lee, Kyungsoo Jung, Ji-Young Song, Min-Jung Sung, Sung-Bin Ahn, Boram Lee, Doo-Yi Oh, Yoon-La Choi
Molecular Therapy - Oncolytics.2020; 16: 188. CrossRef - Understanding Lineage Plasticity as a Path to Targeted Therapy Failure in EGFR-Mutant Non-small Cell Lung Cancer
Tatiana Shaurova, Letian Zhang, David W. Goodrich, Pamela A. Hershberger
Frontiers in Genetics.2020;[Epub] CrossRef - Characterization of head and neck squamous cell carcinoma arising in young patients: Particular focus on molecular alteration and tumor immunity
Hyang Joo Ryu, Eun Kyung Kim, Byoung Chul Cho, Sun Och Yoon
Head & Neck.2019; 41(1): 198. CrossRef - Investigating Trk Protein Expression between Oropharyngeal and Non-oropharyngeal Squamous Cell Carcinoma: Clinical Implications and Possible Roles of Human Papillomavirus Infection
Yoon Ah Cho, Ji Myung Chung, Hyunmi Ryu, Eun Kyung Kim, Byoung Chul Cho, Sun Och Yoon
Cancer Research and Treatment.2019; 51(3): 1052. CrossRef - NOVA1 induction by inflammation and NOVA1 suppression by epigenetic regulation in head and neck squamous cell carcinoma
Eun Kyung Kim, Yoon Ah Cho, Mi-kyoung Seo, Hyunmi Ryu, Byoung Chul Cho, Yoon Woo Koh, Sun Och Yoon
Scientific Reports.2019;[Epub] CrossRef - Advances in studies of tyrosine kinase inhibitors and their acquired resistance
Qinlian Jiao, Lei Bi, Yidan Ren, Shuliang Song, Qin Wang, Yun-shan Wang
Molecular Cancer.2018;[Epub] CrossRef - The long coding RNA AFAP1-AS1 promotes tumor cell growth and invasion in pancreatic cancer through upregulating the IGF1R oncogene via sequestration of miR-133a
Bo Chen, Qinhua Li, Yongping Zhou, Xujing Wang, Qiqi Zhang, Yongkun Wang, Huiren Zhuang, Xiaohua Jiang, Wujun Xiong
Cell Cycle.2018; 17(16): 1949. CrossRef - Overexpression of lncRNA EGFR‑AS1 is associated with a poor prognosis and promotes chemotherapy resistance in non‑small cell lung cancer
Yu-Hua Xu, Jian-Ren Tu, Tian-Tian Zhao, Shi-Guang Xie, Sheng-Bo Tang
International Journal of Oncology.2018;[Epub] CrossRef - IGF-IR signaling in epithelial to mesenchymal transition and targeting IGF-IR therapy: overview and new insights
Heming Li, Izhar Singh Batth, Xiujuan Qu, Ling Xu, Na Song, Ruoyu Wang, Yunpeng Liu
Molecular Cancer.2017;[Epub] CrossRef - Insulin-like growth factor 1 receptor expression in advanced non-small-cell lung cancer and its impact on overall survival
Mojca Humar, Izidor Kern, Gregor Vlacic, Vedran Hadzic, Tanja Cufer
Radiology and Oncology.2017; 51(2): 195. CrossRef - IGF1R depletion facilitates MET-amplification as mechanism of acquired resistance to erlotinib in HCC827 NSCLC cells
Dianna Hussmann, Anne Tranberg Madsen, Kristine Raaby Jakobsen, Yonglun Luo, Boe Sandahl Sorensen, Anders Lade Nielsen
Oncotarget.2017; 8(20): 33300. CrossRef - Upregulated Neuro-oncological Ventral Antigen 1 (NOVA1) Expression Is Specific to Mature and Immature T- and NK-Cell Lymphomas
Eun Kyung Kim, Sun Och Yoon, Soo Hee Kim, Woo Ick Yang, Yoon Ah Cho, Soo Jeong Kim
Journal of Pathology and Translational Medicine.2016; 50(2): 104. CrossRef - The Clinical Significance of the Insulin-Like Growth Factor-1 Receptor Polymorphism in Non-Small-Cell Lung Cancer with Epidermal Growth Factor Receptor Mutation
Tu-Chen Liu, Ming-Ju Hsieh, Ming-Che Liu, Whei-Ling Chiang, Thomas Tsao, Shun-Fa Yang
International Journal of Molecular Sciences.2016; 17(5): 763. CrossRef
- Expression of Amine Oxidase Proteins in Adrenal Cortical Neoplasm and Pheochromocytoma
Brief Case Report
- Heterotopic Pancreas in Omphalomesenteric Duct Remnant Results in Persistent Umbilical Discharge
- Eunhyang Park, Hyojin Kim, Kyu Whan Jung, Jin-Haeng Chung
- Korean J Pathol. 2014;48(4):323-326. Published online August 26, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.4.323
- 7,998 View
- 44 Download
- 17 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Umbilical heterotopic pancreas in an infant: a case report
Abdulkarim Hasan, Basheer Abdullahi Jabo, Zakaria Elaskary, Khaldon Abdulrahman Alaghbari, Mohamed Abbas Ibrahim, Khalid Nafie
Journal of Pediatric Surgery Case Reports.2025; 120: 103053. CrossRef - Heterotopic pancreas: A diagnosis of exclusion not to ignore
Puneeth Thalasta, Yashwant Singh Rathore, Kamal Kataria, Sunil Chumber, Rajni Yadav, Gopal Puri, Prasanna Ramana Arumugaswamy, Gagan Soni, Ankit Anand
Saudi Surgical Journal.2024; 12(1): 9. CrossRef - Heterotopic Pancreas Mimicking Metastases From Renal Carcinoma
Deepanksha Datta, Rajesh Kumar, Peeyush Varshney, Sudeep Khera, Tanisha Gupta
Clinical Nuclear Medicine.2023; 48(2): e74. CrossRef - Ectopic pancreas, gastric, duodenal and colonic tissue in a case of persistent umbilical discharge
Pavithra Ayyanar, Bikash B. Tripathy, Akash B. Pati, Manoj K. Mohanty, Mukund Sable
Indian Journal of Pathology and Microbiology.2023; 66(2): 403. CrossRef - Amylase Levels Are Useful for Diagnosing Omphalomesenteric Cysts: A Case Report
Hiroko Yoshizawa, Keita Terui, Mitsuyuki Nakata, Tetsuya Mitsunaga, Shugo Komatsu, Takeshi Saito, Tomoro Hishiki
Pediatric Reports.2022; 14(1): 127. CrossRef - Persistent umbilical polyp in a 5-year-old boy – A rare case report with literature review
Asitava Deb Roy, Ritu Roy, Shilpa
IP Archives of Cytology and Histopathology Research.2022; 7(2): 126. CrossRef - Ectopic pancreas
Fang-Chin Hsu, Hai-Ning Hsu, Yi-Jen Peng, Kuo-Feng Hsu
Formosan Journal of Surgery.2021; 54(6): 244. CrossRef - Heterotopic Pancreas Located at the Gastroesophageal Junction in a Hiatal Hernia: A Case Report
Joshua K Jenkins, Forest Smith, Stephen Mularz, Shweta Chaudhary
Cureus.2021;[Epub] CrossRef - Histomorphology of the lesions of the umbilicus
Saranya Singaravel, Poonam C. Yadav
Indian Journal of Pathology and Microbiology.2021; 64(1): 91. CrossRef - Loss of GATA4 causes ectopic pancreas in the stomach
Elisa Rodríguez‐Seguel, Laura Villamayor, Noelia Arroyo, Mónica P De Andrés, Francisco X Real, Franz Martín, David A Cano, Anabel Rojas
The Journal of Pathology.2020; 250(4): 362. CrossRef - Bleeding Umbilical Papule: Answer
Cuong V. Nguyen, Patrick J. McMahon, Ata S. Moshiri, Tricia R. Bhatti, Adam I. Rubin
The American Journal of Dermatopathology.2020; 42(3): 224. CrossRef - Atypical presentations of ectopic pancreatic tissue
P.S. Sulser, S. Azarhoush, D.C. Aronson, S.J. Tharakan, N. Zweifel, U. Moehrlen
Journal of Pediatric Surgery Case Reports.2020; 58: 101450. CrossRef - Intramural ectopic pancreatic tissue of the stomach: A case report of an uncommon origin of a non-cancerous gastric tumour
Enrica Chiriatti, Paulina Kuczma, Domenico Galasso, E. Koliakos, Edgardo Pezzetta, Olivier Martinet
International Journal of Surgery Case Reports.2020; 73: 48. CrossRef - Surgical abdominal exploration in children with umbilical ectopic gastrointestinal tissue
Yi-Li Hou, Jao-Yu Lin
Journal of Pediatric Surgery Case Reports.2019; 49: 101281. CrossRef - Rare case of ectopic pancreas presenting with persistent umbilical discharge
Kazuhiko Nakame, Roko Hamada, Masaya Suzuhigashi, Atsushi Nanashima, Satoshi Ieiri
Pediatrics International.2018; 60(9): 891. CrossRef - Heterotopic Pancreas: Histopathologic Features, Imaging Findings, and Complications
Maryam Rezvani, Christine Menias, Kumaresan Sandrasegaran, Jeffrey D. Olpin, Khaled M. Elsayes, Akram M. Shaaban
RadioGraphics.2017; 37(2): 484. CrossRef - Heterotopic pancreas in the omphalomesenteric duct remnant in a 9-month-old girl: a case report and literature review
Zitong Zhao, Chiang Khi Sim, Sangeeta Mantoo
Diagnostic Pathology.2017;[Epub] CrossRef
- Umbilical heterotopic pancreas in an infant: a case report

 E-submission
E-submission

 First
First Prev
Prev



