Search
- Page Path
- HOME > Search
Case Study
- A Case of Malignant PEComa of the Uterus Associated with Intramural Leiomyoma and Endometrial Carcinoma
- Yoo Jin Choi, Jin Hwa Hong, Aeree Kim, Hankyeom Kim, Hyeyoon Chang
- J Pathol Transl Med. 2016;50(6):469-473. Published online July 25, 2016
- DOI: https://doi.org/10.4132/jptm.2016.04.20
- 10,113 View
- 201 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
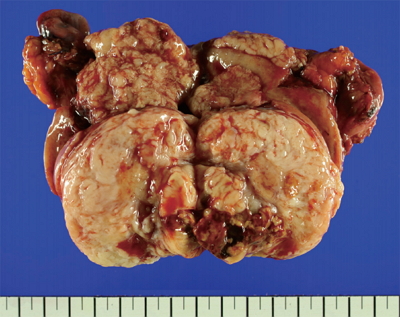
PDF - Perivascular epithelioid cell tumors (PEComas) refers to a family of mesenchymal neoplasms composed of angiomyolipomas, clear cell “sugar” tumors of the lung, and lymphangioleiomyomatoses. These tumors have a distinctive and common component of perivascular epithelioid cells that show an association with blood vessel walls and immunohistochemically display myomelanocytic differentiation. The unique neoplasms have been shown to have an expanded range through a variety of case reports, including visceral, intra-abdominal, soft tissue, and bone tumors. The retroperitoneum, abdominopelvic region, and uterus have been reported to be the most common sites. Most PEComas follow a benign course. However, reports of malignant PEComas are increasing. Many papers have described uterine PEComas, but to our knowledge, there have not yet been any reports of a malignant PEComa arising concomitant with another epithelial tumor and mesenchymal tumor. We report herein the case of a 67-year-old woman who experienced a malignant uterine PEComa infiltrating a preexisting intramural leiomyoma with synchronous well differentiated endometrial carcinoma and multiple liver and lung metastases.
-
Citations
Citations to this article as recorded by- Risk prediction criteria for the primary hepatic perivascular epithelioid cell tumour family, including angiomyolipoma: analysis of 132 cases with a literature review
Youngeun Yoo, Jihun Kim, In Hye Song
Histopathology.2025; 86(6): 979. CrossRef - Metastasis of Clear Cell Renal Cell Carcinoma to Uterine Leiomyoma: First Case Report and Review of Literature
Sarvenaz Karamooz, Paula D. Binsol, Jaya Ruth Asirvatham, Anjali Pargaonkar
International Journal of Surgical Pathology.2024; 32(8): 1552. CrossRef - Uterine collision tumor (PEComa and endometrioid carcinoma) in a tuberous sclerosis patient: a case report
Nektarios Koufopoulos, Ioannis S. Pateras, Christos Koratzanis, Alina-Roxani Gouloumis, Argyro-Ioanna Ieronimaki, Alexandros Fotiou, Ioannis G. Panayiotides, Nikolaos Vrachnis
Frontiers in Oncology.2023;[Epub] CrossRef - TFE3-associated perivascular epithelioid cell tumor with complete response to mTOR inhibitor therapy: report of first case and literature review
Roli Purwar, Kishan Soni, Mridula Shukla, Ashish Verma, Tarun Kumar, Manoj Pandey
World Journal of Surgical Oncology.2022;[Epub] CrossRef - A case of perivascular epithelioid nodules arising in an intramural leiomyoma
Yoldez Houcine, Karima Mekni, Emna Brahem, Mouna Mlika, Aida Ayadi, Chiraz Fekih, Imene Ridene, Faouzi El Mezni
Human Pathology: Case Reports.2021; 23: 200470. CrossRef - Perivascular epithelioid cell tumors (PEComa) of the female genital tract: A challenging question for gynaecologic oncologist and pathologist
Angiolo Gadducci, Gian Franco Zannoni
Gynecologic Oncology Reports.2020; 33: 100603. CrossRef - Five cases of uterine perivascular epithelioid cell tumors (PEComas) and review of literature
Weiwei Shan, Yue Shi, Qin Zhu, Bingyi Yang, Liying Xie, Bing Li, Chengcheng Ning, Qiaoying Lv, Yali Cheng, Bingying Xie, Mingzhu Bai, Yuhui Xu, Xiaojun Chen, Xuezhen Luo
Archives of Gynecology and Obstetrics.2019; 299(1): 185. CrossRef - Uterine PEComas
Jennifer A. Bennett, Ana C. Braga, Andre Pinto, Koen Van de Vijver, Kristine Cornejo, Anna Pesci, Lei Zhang, Vicente Morales-Oyarvide, Takako Kiyokawa, Gian Franco Zannoni, Joseph Carlson, Tomas Slavik, Carmen Tornos, Cristina R. Antonescu, Esther Oliva
American Journal of Surgical Pathology.2018; 42(10): 1370. CrossRef
- Risk prediction criteria for the primary hepatic perivascular epithelioid cell tumour family, including angiomyolipoma: analysis of 132 cases with a literature review
Letter to the Editor
- Reappraisal of 'The Korean Journal of Pathology, 2010; 44: 111-6' by Youngjoon Ryu et al. and Comments on 'The Korean Journal of Pathology, 2010; 44: 343-5' by Kyu Won Jung and Soong Deok Lee.
- Youngjoon Ryu, Bongkyung Shin, Baek Hui Kim, Aeree Kim, Hankyeom Kim
- Korean J Pathol. 2010;44(5):453-455.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.5.453
- 2,742 View
- 25 Download
Review Article
- Legal and Ethical Consideration in the Use of Human Biological Material.
- Youngjoon Ryu, Bongkyung Shin, Baek Hui Kim, Aeree Kim, Hankyeom Kim
- Korean J Pathol. 2010;44(2):111-116.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.111
- 3,650 View
- 39 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Traditionally, pathologists have used human biological material primarily for diagnostic purposes. More recently, advances in biomedical technology and changes in the research environment have placed new demands on pathologists and their handling of human materials. Moreover, these technological advances have required pathologists to be not only experts in diagnosis, but also managers of biobanks storing human biological material. Consequently, pathologists might now be confronted with unanticipated legal and ethical questions. We investigated seven examples of South Korean legislation concerning human biological material, including "The Bioethics and Safety Act" (2005), and we considered possible conflicts of interest between donors and researchers. We also reviewed international bioethical guidelines and legal precedents from several countries with special regard to pathologic glass slides, paraffin blocks, remaining specimens and other guidelines. We conclude that a better understanding of the legal and ethical questions concerning human biological material leads pathologists to safer and more conscientious management of these samples.
-
Citations
Citations to this article as recorded by- Proposal for the development of a human biological material management system for research hospitals
Young-Joon Ryu, Hankyeom Kim, Sejin Jang
Journal of the Korean Medical Association.2012; 55(3): 292. CrossRef
- Proposal for the development of a human biological material management system for research hospitals
Case Report
- Extramedullary B Lymphoblastic Crisis of CML, Presenting as a Leptomeningeal Tumor: A Case Report.
- Hoiseon Jeong, Bongkyung Shin, Sook Young Bae, Sangho Lee, Youngjune Ryu, Hankyeom Kim, Insun Kim
- Korean J Pathol. 2009;43(5):482-488.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.5.482
- 3,250 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF - We report here on a rare case of a patient who presented with an extramedullary B lymphoblastic crisis as an initial manifestation of chronic myelogenous leukemia (CML). A 71-year-old man visited the emergency room due to suddenly developed dysarthria and right side weakness. Emergency craniotomy was done under the presumptive diagnosis of subdural hemorrhage. During the operation, a poorly demarcated firm mass was identified in the leptomeningeal space. Microscopically, the majority of the tumor was composed of monotonous immature cells with blast morphology, and these cells were immunoreactive for TdT, CD34, CD10 and CD20, indicating the precursor B-cell phenotype. The peripheral area of the tumor consisted of myeloid cells in various stages of maturation, and these cells were reactive for myeloperoxidase, chloroacetate esterase, CD43 and CD15. FISH analysis using the LSI bcr-abl dual color probe showed gene fusion signals in both the B-lymphoblasts and myeloid cells. The peripheral blood and bone marrow findings were consistent with CML with no evidence of a blast crisis. Cytogenetic study of the bone marrow demonstrated the 46, XY, t(9;22)(q34;q11) chromosome. A diagnosis of extramedullary B lymphoblastic blast crisis in a patient with Philadelphia chromosome-positive CML was made. Despite treatment, the patient died 3 months after he was diagnosed.
Original Articles
- Pathological Characteristics of 20 Cases of Langerhans Cell Histiocytosis and Specificity of Immunohistochemical Stain of Langerin (CD207).
- Youngjoon Ryu, Hyunjoo Lee, Sangho Lee, Hoiseon Jeong, Bongkyung Shin, Aeree Kim, Hankyeom Kim, Insun Kim
- Korean J Pathol. 2009;43(2):113-119.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.2.113
- 3,964 View
- 40 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Langerhans cell histiocytosis (LCH) is a well-known neoplastic disorder of Langerhans cells which has characteristic findings, however, LCH has not been adequately studied in Korea.
METHODS
We analyzed the clinicopathologic features of 20 patients with LCH who were diagnosed between 1997 and 2006 at the Korea University Guro and Anam Hospitals.
RESULTS
The M:F ratio was 3:1 and the age ranged from 2-60 years (mean, 23.8 years [4 in 1st decade, 6 in 2nd decade, 2 in 3rd decade, 5 in 4th decade and 3> or =40 years of age). The cases were classified as unifocal unisystemic in 13 patients, multifocal unisystemic in 4 patients, and multifocal multisystemic in 3 patients. The bone was the most commonly involved organ (14), followed by lymph node (5), lung (2), skin (2) and ureter (1). The Langerhans cells were immunohistochemically stained with Langerin, CD1a, S-100 protein, and CD68. Langerin and CD1a were specific for Langerhans cells.
CONCLUSIONS
The distribution of the involved organs in patients with LCH was similar to the distribution in Western countries, but lymph node involvement was more frequent, whereas lung involvement was less common. Langerin is considered to be a specific marker for Langerhans cells. -
Citations
Citations to this article as recorded by- Treatment Outcome of Langerhans Cell Histocytosis
So Hak Chung, Jae Do Kim, Hyun Ik Jo
The Journal of the Korean Bone and Joint Tumor Society.2014; 20(1): 14. CrossRef
- Treatment Outcome of Langerhans Cell Histocytosis
- The Clinicopathological Characteristics of Gastrointestinal Neuroendocrine Tumors; An Analysis of 65 Cases.
- Hyunjoo Lee, Jungwoo Choi, Jung Suk An, Hyunchul Kim, Bong Kyung Shin, Aeree Kim, Hankyeom Kim, Insun Kim
- Korean J Pathol. 2007;41(3):149-157.
- 1,998 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Background
: This study was designed to investigate gastrointestinal neuroendocrine tumors with an emphasis on their clinicopathological characteristics.
Methods
: Sixty-five cases were reviewed and classified as typical carcinoid (TC), atypical carcinoid (AC), large cell neuroendocrine carcinoma (LCNEC) and small cell carcinoma (SmCC). We performed immunohistochemistry to characterize the expression of the immunoreactivity for synaptophysin, chromogranin, gastrin, somatostatin, thyroid transcription factor-1, p53 and Ki-67.
Results
: Most commonly, the tumors were located in the rectum (54%), followed by the stomach (23%) and colon (9%). Histologically, the tumors were classified as 49 TCs, 4 ACs, 6 LCNECs and 6 SmCCs. Most tumors were stained positive for synaptophysin and/or chromogranin. Four LCNECs and one SmCC were p53-positive. The carcinoids revealed a low level (<5%) of reactivity for Ki-67, while > or =30% of the cells showed reactivity for Ki-67 in the majority of LCNECs and SmCCs. Six patients with metastatic carcinoids were older than those patients without metastasis (64 vs 48 years, respectively, p=0.004). Furthermore, the size of tumors was larger for the patients with metastatic carcinoids than for the patients with nonmetastatic carcinoids (2.3 vs 0.5 cm, respectively, p=0.005).
Conclusion
: Old age, large tumor size and muscle invasion are associated with high grade neuroendocrine tumor and lymph node metastasis for those patients with carcinoids.

 E-submission
E-submission

 First
First Prev
Prev



