Search
- Page Path
- HOME > Search
- Clinicopathological characteristics of digestive system angioleiomyomas: case report and literature review
- Georgios Kalliopitsas, Christos Topalidis, Constantine Halkias, Theodora Gkeka, Konstantinos Sapalidis, Triantafyllia Koletsa
- J Pathol Transl Med. 2025;59(6):453-459. Published online October 28, 2025
- DOI: https://doi.org/10.4132/jptm.2025.08.04
- 2,437 View
- 104 Download
-
 Abstract
Abstract
 PDF
PDF - Angioleiomyomas are benign soft tissue tumors originating from the vascular wall. Although angioleiomyomas mainly occur in extremities, followed by head, neck, and trunk, they can also be found throughout the digestive system and especially in the oral cavity. Herein, the fourth case of a rectal angioleiomyoma in the English literature is reported and the clinicopathological features of digestive system angioleiomyomas were investigated. In contrast to their soft tissue counterparts, digestive system angioleiomyomas mainly affect males at a slightly younger age. Angioleiomyomas are mainly asymptomatic and only rarely elicit pain. Clinicians consider angioleiomyomas infrequently and instead include more common soft tissue or epithelial tumors in their differential diagnosis. To prevent angiomyolipoma misdiagnosis, pathologists should exercise caution when examining an angioleiomyoma composed of adipose tissue, smooth muscle, and blood vessels. Pathologists, radiologists, and surgeons should be aware that angioleiomyomas can occur in the digestive system.
- Elevated expression of Axin2 in intestinal metaplasia and gastric cancers
- Dong Hui Lee, In Ho Jeong, Bogun Jang
- J Pathol Transl Med. 2023;57(6):315-322. Published online November 7, 2023
- DOI: https://doi.org/10.4132/jptm.2023.10.12
- 4,946 View
- 233 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The Wnt signaling pathway regulates crucial cellular processes, including stem cell development and tissue repair. Dysregulation of this pathway, particularly β-catenin stabilization, is linked to colorectal carcinoma and other tumors. Axin2, a critical component in the pathway, plays a role in β-catenin regulation. This study examines Axin2 expression in normal gastric mucosa and various gastric pathologies.
Methods
Formalin-fixed and paraffin-embedded tissue samples from normal stomach, gastritis, intestinal metaplasia (IM), and gastric carcinoma were collected. Axin2 and β-catenin expression were evaluated using RNA in situ hybridization and immunohistochemistry, respectively. Histo-scores (H-scores) were calculated to quantify expression levels of Axin2. Associations between Axin2 expression and clinicopathological variables were examined.
Results
Axin2 expression was examined in normal stomach, gastritis, and IM tissues. Axin2 expression was mainly observed in the surface and isthmus areas in the normal stomach and gastritis, whereas Axin2 expression was markedly higher at the bases of IM. Axin2 H-scores were significantly elevated in IM (mean ± standard deviation [SD], 87.0 ± 38.9) compared to normal (mean ± SD, 18.0 ± 4.5) and gastritis tissues (mean ± SD, 33.0 ± 18.6). In total, 30% of gastric carcinomas showed higher Axin2 expression. Axin2 expression did not have significant associations with age, sex, Lauren classification, histological differentiation, invasion depth, and lymph node metastasis. However, a strong positive correlation was observed between Axin2 and nuclear β-catenin in gastric carcinomas (p < .001).
Conclusions
Axin2 expression was significantly increased in IM compared to normal and gastritis cases. In addition, Axin2 showed a strong positive association with nuclear β-catenin expression in gastric carcinomas, demonstrating a close relationship with abnormal Wnt/β-catenin signaling pathway. -
Citations
Citations to this article as recorded by- A review of potential mechanisms and treatments of gastric intestinal metaplasia
Yueyao Wu, Kehan Zhang, Yichao Zheng, Haifeng Jin
European Journal of Gastroenterology & Hepatology.2025; 37(4): 383. CrossRef - Refining NTRK Fusion Detection in Papillary Thyroid Carcinoma Through Pan-TRK Immunohistochemistry and Histopathologic Features
Hyun Lee, Sue Youn Kim, Ji Min Park, Seung-Hyun Jung, Ozgur Mete, Chan Kwon Jung
Endocrine Pathology.2025;[Epub] CrossRef - AXIN2 variants, tooth agenesis, and cancer risk: a systematic review
Nutthakarn Ratanasereeprasert, Narin Intarak, Chayanit Chaweewannakorn, Mushriq Abid, Anand Marya, Sung-dae Cho, Thantrira Porntaveetus
BMC Oral Health.2025;[Epub] CrossRef - Discovery of Atirmociclib (PF-07220060): A Potent and Selective CDK4 Inhibitor
Gary M. Gallego, Cynthia Palmer, Suvi Orr, Louise Bernier, Ping Chen, Sujin Cho-Schultz, Judith G. Deal, Klaus Dress, Martin Edwards, Mehran Jalaie, Eric Johnson, Robert Kania, John C. Kath, Jennifer Lafontaine, Sacha Ninkovic, Neal Sach, Hong Shen, Lars
Journal of Medicinal Chemistry.2025; 68(24): 26085. CrossRef - Listening to the Past, Shaping the Future: A Data-mining Based and Visual Analysis of Five Decades of Gastric Carcinogenesis Research
Tai Zhang, Xudong Tang
Biological Procedures Online.2025;[Epub] CrossRef - Postbiotics Combination Synergises the Antiproliferative Effects of Doxorubicin in Gastric Cancer Cells: A Cellular and Molecular Deep Dive
Radwa A. Eladwy, Mohamed Fares, Muhammad A. Alsherbiny, Dennis Chang, Chun-Guang Li, Deep Jyoti Bhuyan
International Journal of Molecular Sciences.2025; 27(1): 362. CrossRef
- A review of potential mechanisms and treatments of gastric intestinal metaplasia
- Solitary Peutz-Jeghers type harmartomatous polyp in duodenum with gastric foveolar epithelium: a case report
- Eugene Choi, Junghwan Lee, Youngsoo Park
- J Pathol Transl Med. 2023;57(2):128-131. Published online January 10, 2023
- DOI: https://doi.org/10.4132/jptm.2022.11.07
- 5,325 View
- 190 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Peutz-Jeghers type hamartomatous polyp is known to be associated with Peutz-Jeghers syndrome, which shows characteristic multiple hamartomatous polyp involvement in the gastrointestinal tract, combined with mucocutaneous symptom, familial history of Peutz- Jeghers syndrome or STK11/LTB1 mutation. However, some cases showing histologic appearance of the polyps discovered in Peutz- Jeghers syndrome while lacking other diagnostic criteria of the syndrome have been reported, and these are called solitary Peutz- Jeghers type polyps. Herein, we report a case of solitary Peutz-Jeghers type polyp covered with heterotopic epithelium. The patient was 47-year-old female without any mucocutaneous symptoms nor familial history of Peutz-Jeghers syndrome. Microscopic examination revealed Peutz-Jeghers type hamartomatous polyp in duodenum covered with gastric type foveolar epithelium. Considering the definition of hamartomatous polyp, which is, the abnormal overgrowth of the indigenous epithelial component, the histological feature of current case is noteworthy in a point that it shows proliferation of heterotopic component, rather than the indigenous component.
-
Citations
Citations to this article as recorded by- A Solitary Peutz-Jeghers Hamartomatous Polyp in the Gastric Body: A Case Report
Noelia Madera, Noemí Acevedo, Carmen González-Peralta, Rafael Castro, Vismelis Mezquita-Luna
Cureus.2024;[Epub] CrossRef
- A Solitary Peutz-Jeghers Hamartomatous Polyp in the Gastric Body: A Case Report
- Identification of PI3K-AKT signaling as the dominant altered pathway in intestinal type ampullary cancers through whole-exome sequencing
- Niraj Kumari, Rajneesh K. Singh, Shravan K. Mishra, Narendra Krishnani, Samir Mohindra, Raghvendra L.
- J Pathol Transl Med. 2021;55(3):192-201. Published online March 9, 2021
- DOI: https://doi.org/10.4132/jptm.2021.01.23
- 7,535 View
- 133 Download
- 7 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The genetic landscape of intestinal (INT) and pancreatobiliary (PB) type ampullary cancer (AC) has been evolving with distinct as well as overlapping molecular profiles.
Methods
We performed whole-exome sequencing in 37 cases of AC to identify the targetable molecular profiles of INT and PB tumors. Paired tumor-normal sequencing was performed on the HiSeq 2500 Illumina platform.
Results
There were 22 INT, 13 PB, and two cases of mixed differentiation of AC that exhibited a total of 1,263 somatic variants in 112 genes (2–257 variants/case) with 183 somatic deleterious variants. INT showed variations in 78 genes (1–31/case), while PB showed variations in 51 genes (1–29/case). Targetable mutations involving one or more major pathways were found in 86.5% of all ACs. Mutations in APC, CTNNB1, SMAD4, KMT2, EPHA, ERBB, and Notch genes were more frequent in INT tumors, while chromatin remodeling complex mutations were frequent in PB tumors. In the major signaling pathways, the phosphoinositide 3-kinase (PI3)/AKT and RAS/mitogen-activated protein kinase (MAPK) pathways were significantly mutated in 70% of cases (82% INT, 46% PB, p = .023), with PI3/AKT mutation being more frequent in INT and RAS/MAPK in PB tumors. Tumor mutation burden was low in both differentiation types, with 1.6/Mb in INT and 0.8/Mb in PB types (p =.217).
Conclusions
The exome data suggest that INT types are genetically more unstable than PB and involve mutations in tumor suppressors, oncogenes, transcription factors, and chromatin remodeling genes. The spectra of the genetic profiles of INT and PB types suggested primary targeting of PI3/AKT in INT and RAS/RAF and PI3/AKT pathways in PB carcinomas. -
Citations
Citations to this article as recorded by- Rare, Yet Targetable: New Perspectives on Ampullary Carcinomas
James Gutmans, Alex Friedlaender, Hiba Mechahougui
International Journal of Molecular Sciences.2026; 27(3): 1597. CrossRef - Identification of anoikis-related genes to develop a risk model and predict the prognosis and tumor microenvironment in rectal adenocarcinoma
Bing Zhao, Xuegui Tang
Frontiers in Genetics.2025;[Epub] CrossRef - Рак Фатерова сосочка
Л. Ю. Владимирова, А. К. Алькина, Е. А. Калабанова
Malignant tumours.2025; 15(3s1): 55. CrossRef - Molecular aspects of BRAF and HER2 in prognosis of periampullary carcinoma
Apurva, Nimisha, Abhay Kumar Sharma, Arun Kumar, Ejaj Ahmad, Seneha Santoshi, Sundeep Singh Saluja
Pancreatology.2024; 24(7): 1084. CrossRef - Comparison of clinical characteristics and prognostic factors in two site-specific categories of ampullary cancer
Jing-Zhao Zhang, Zhi-Wei Zhang, Xin-Yi Guo, Deng-Sheng Zhu, Xiao-Rui Huang, Ming Cai, Tong Guo, Ya-Hong Yu
World Journal of Gastroenterology.2024; 30(39): 4281. CrossRef - The role of histone post-translational modifications in cancer and cancer immunity: functions, mechanisms and therapeutic implications
Xiaohong Duan, Zhiyao Xing, Lu Qiao, Shan Qin, Xuejing Zhao, Yanhua Gong, Xueren Li
Frontiers in Immunology.2024;[Epub] CrossRef - Molecular pathways in periampullary cancer: An overview
Apurva, Real Sumayya Abdul Sattar, Asgar Ali, Nimisha, Abhay Kumar Sharma, Arun Kumar, Seneha Santoshi, Sundeep Singh Saluja
Cellular Signalling.2022; 100: 110461. CrossRef - Histologic subtyping of ampullary carcinoma for targeted therapy
Seung-Mo Hong
Journal of Pathology and Translational Medicine.2021; 55(3): 235. CrossRef
- Rare, Yet Targetable: New Perspectives on Ampullary Carcinomas
- Gastric IgG4-related disease presenting as a mass lesion and masquerading as a gastrointestinal stromal tumor
- Banumathi Ramakrishna, Rohan Yewale, Kavita Vijayakumar, Patta Radhakrishna, Balakrishnan Siddartha Ramakrishna
- J Pathol Transl Med. 2020;54(3):258-262. Published online March 4, 2020
- DOI: https://doi.org/10.4132/jptm.2020.02.10
- 7,604 View
- 159 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - IgG4-related disease of the stomach is a rare disorder, and only a few cases have been reported. We present two cases that were identified over a 2-month period in our center. Two male patients aged 52 and 48 years presented with mass lesion in the stomach, which were clinically thought to be gastrointestinal stromal tumor, and they underwent excision of the lesion. Microscopic examination revealed marked fibrosis, which was storiform in one case, associated with diffuse lymphoplasmacytic infiltration and an increase in IgG4-positive plasma cells on immunohistochemistry. Serum IgG4 level was markedly elevated. Although rare, IgG4-related disease should be considered in the differential diagnosis of gastric submucosal mass lesions.
-
Citations
Citations to this article as recorded by- Isolated IgG4-related disease of terminal ileum: Report of a rare case and review of literature
Subham Bhowmik, Hemanga K. Bhattacharjee, Joyner Abraham, Raju Sharma, Prasenjit Das
Journal of Cancer Research and Therapeutics.2025; 21(1): 200. CrossRef - Great Mimics in Oncology: A Retrospective Study from a Tertiary Care Centre of Eastern India
Suvendu Maji, Jayesh kumar Jha, Vikram Chaturvedi
Indian Journal of Surgical Oncology.2025; 16(1): 64. CrossRef - Systemic diseases affecting the GI tract: A review of clinical and histopathologic manifestations
Maryam K. Pezhouh, Dora Lam-Himlin, Atif Zaheer, Lysandra Voltaggio
Annals of Diagnostic Pathology.2024; 73: 152351. CrossRef - Utilizing Immunoglobulin G4 Immunohistochemistry for Risk Stratification in Patients with Papillary Thyroid Carcinoma Associated with Hashimoto Thyroiditis
Faridul Haq, Gyeongsin Park, Sora Jeon, Mitsuyoshi Hirokawa, Chan Kwon Jung
Endocrinology and Metabolism.2024; 39(3): 468. CrossRef - Compromiso gástrico por enfermedad relacionada con IgG4
Gilberto Jaramillo Trujillo, Oscar Fernando Ruiz, Melissa González Pabón, Maria Andrea Jaramillo Trujillo
Revista Repertorio de Medicina y Cirugía.2024; 33(3): 319. CrossRef - CGB5, INHBA and TRAJ19 Hold Prognostic Potential as Immune Genes for Patients with Gastric Cancer
Bei Ji, Lili Qiao, Wei Zhai
Digestive Diseases and Sciences.2023; 68(3): 791. CrossRef - IgG4-related diseases of the digestive tract
J.-Matthias Löhr, Miroslav Vujasinovic, Jonas Rosendahl, John H. Stone, Ulrich Beuers
Nature Reviews Gastroenterology & Hepatology.2022; 19(3): 185. CrossRef - Clinicopathological characteristics of gastric IgG4‐related disease: Systematic scoping review
Haruki Sawada, Torrey Czech, Krixie Silangcruz, Landon Kozai, Adham Obeidat, Eric Andrew Wien, Midori Filiz Nishimura, Asami Nishikori, Yasuharu Sato, Yoshito Nishimura
Journal of Gastroenterology and Hepatology.2022; 37(10): 1865. CrossRef - Utility of gastric biopsy in diagnosing IgG4‐related gastrointestinal disease
Kaori Uchino, Kenji Notohara, Takeshi Uehara, Yasuhiro Kuraishi, Junya Itakura, Akihiro Matsukawa
Pathology International.2021; 71(2): 124. CrossRef
- Isolated IgG4-related disease of terminal ileum: Report of a rare case and review of literature
- Molecular and Clinicopathological Features of Gastrointestinal Stromal Tumors in Vietnamese Patients
- Quoc Dat Ngo, Quoc Thang Pham, Dang Anh Thu Phan, Anh Vu Hoang, Thi Ngoc Ha Hua, Sao Trung Nguyen
- J Pathol Transl Med. 2019;53(6):361-368. Published online September 16, 2019
- DOI: https://doi.org/10.4132/jptm.2019.08.27
- 8,279 View
- 160 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Gastrointestinal stromal tumors (GISTs) are the most frequent mesenchymal neoplasms of the gastrointestinal tract. Management of GIST patients is currently based on clinicopathological features and associated genetic changes. However, the detailed characteristics and molecular genetic features of GISTs have not yet been described in the Vietnamese population.
Methods
We first identified 155 patients with primary GIST who underwent surgery with primary curative intent between 2011 and 2014 at University Medical Center at Ho Chi Minh City, Vietnam. We evaluated the clinicopathological features and immunohistochemical reactivity to p53 and Ki-67 in these patients. Additionally, KIT genotyping was performed in 100 cases.
Results
The largest proportion of GISTs was classified as high-risk (43.2%). Of the 155 GISTs, 52 (33.5%) were positive for Ki-67, and 58 (37.4%) were positive for p53. The expression of Ki-67 and p53 were correlated with mitotic rate, tumor size, risk assessment, and tumor stage. Out of 100 GIST cases, KIT mutation was found in 68%, of which 62 (91.2%) were found in exon 11, two (2.9%) in exon 9, and four (5.8%) in exon 17. No mutation in exon 13 was identified. Additionally, KIT mutations did not correlate with any clinicopathological features.
Conclusions
The expression of Ki-67 and p53 were associated with high-risk tumors. Mutations in exon 11 were the most commonly found, followed by exon 17 and exon 9. Additionally, KIT mutation status was not correlated with any recognized clinicopathological features. -
Citations
Citations to this article as recorded by- Ki67 for evaluating the prognosis of gastrointestinal stromal tumors: A systematic review and meta‑analysis
Ji Li, An-Ran Wang, Xiao-Dong Chen, Hong Pan, Shi-Qiang Li
Oncology Letters.2022;[Epub] CrossRef - Endoscopic ultrasound‐guided fine‐needle aspiration cytology in the diagnosis of the gastrointestinal stromal tumor of the stomach
José‐Fernando Val‐Bernal, Elena Yllera, María Moris, Ihab Abdulkader Nallib, Angel Vázquez‐Boquete, María Martino
Diagnostic Cytopathology.2020; 48(9): 833. CrossRef
- Ki67 for evaluating the prognosis of gastrointestinal stromal tumors: A systematic review and meta‑analysis
- Prognostic Impact of Fusobacterium nucleatum Depends on Combined Tumor Location and Microsatellite Instability Status in Stage II/III Colorectal Cancers Treated with Adjuvant Chemotherapy
- Hyeon Jeong Oh, Jung Ho Kim, Jeong Mo Bae, Hyun Jung Kim, Nam-Yun Cho, Gyeong Hoon Kang
- J Pathol Transl Med. 2019;53(1):40-49. Published online December 26, 2018
- DOI: https://doi.org/10.4132/jptm.2018.11.29
- 19,946 View
- 253 Download
- 50 Web of Science
- 53 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
This study aimed to investigate the prognostic impact of intratumoral Fusobacterium nucleatum in colorectal cancer (CRC) treated with adjuvant chemotherapy.
Methods
F. nucleatumDNA was quantitatively measured in a total of 593 CRC tissues retrospectively collectedfrom surgically resected specimens of stage III or high-risk stage II CRC patients who had receivedcurative surgery and subsequent oxaliplatin-based adjuvant chemotherapy (either FOLFOXor CAPOX). Each case was classified into one of the three categories: F. nucleatum–high, –low, or –negative.
Results
No significant differences in survival were observed between the F.nucleatum–high and –low/negative groups in the 593 CRCs (p = .671). Subgroup analyses accordingto tumor location demonstrated that disease-free survival was significantly better in F.nucleatum–high than in –low/negative patients with non-sigmoid colon cancer (including cecal,ascending, transverse, and descending colon cancers; n = 219; log-rank p = .026). In multivariateanalysis, F. nucleatum was determined to be an independent prognostic factor in non-sigmoidcolon cancers (hazard ratio, 0.42; 95% confidence interval, 0.18 to 0.97; p = .043). Furthermore,the favorable prognostic effect of F. nucleatum–high was observed only in a non-microsatellite instability-high (non-MSI-high) subset of non-sigmoid colon cancers (log-rank p = 0.014), but not ina MSI-high subset (log-rank p = 0.844), suggesting that the combined status of tumor locationand MSI may be a critical factor for different prognostic impacts of F. nucleatum in CRCs treatedwith adjuvant chemotherapy.
Conclusions
Intratumoral F. nucleatum load is a potential prognosticfactor in a non-MSI-high/non-sigmoid/non-rectal cancer subset of stage II/III CRCs treatedwith oxaliplatin-based adjuvant chemotherapy. -
Citations
Citations to this article as recorded by- Microbiota and tumor epigenetics: deep interconnections and emerging therapeutic perspectives
Lei Duan, Dan Hu, Haoling Zhang, Yan Liao
Critical Reviews in Clinical Laboratory Sciences.2026; : 1. CrossRef - Unraveling the Role of Fusobacterium nucleatum in Colorectal Cancer: Molecular Mechanisms and Pathogenic Insights
Linda Galasso, Fabrizio Termite, Irene Mignini, Giorgio Esposto, Raffaele Borriello, Federica Vitale, Alberto Nicoletti, Mattia Paratore, Maria Elena Ainora, Antonio Gasbarrini, Maria Assunta Zocco
Cancers.2025; 17(3): 368. CrossRef - Emerging roles of intratumoral microbiota: a key to novel cancer therapies
Pengzhong Fang, Jing Yang, Huiyun Zhang, Diankui Shuai, Min Li, Lin Chen, Liping Liu
Frontiers in Oncology.2025;[Epub] CrossRef - Association of Fusobacterium nucleatum with colorectal cancer molecular subtypes and its outcome: a systematic review
Luana Greco, Federica Rubbino, Clarissa Ferrari, Michela Cameletti, Fabio Grizzi, Fabrizio Bonelli, Alberto Malesci, Massimiliano Mazzone, Luigi Ricciardiello, Luigi Laghi
Gut Microbiome.2025;[Epub] CrossRef - The Interplay Between the Gut Microbiota and Colorectal Cancer: A Review of the Literature
Marco Cintoni, Marta Palombaro, Eleonora Zoli, Giuseppe D’Agostino, Gabriele Pulcini, Elena Leonardi, Pauline Raoul, Emanuele Rinninella, Flavio De Maio, Esmeralda Capristo, Antonio Gasbarrini, Maria Cristina Mele
Microorganisms.2025; 13(6): 1410. CrossRef - Harnessing intratumoral microbiota: new horizons in immune microenvironment and immunotherapy
Jinhe Zhang, Zinan You, Xinqiao Li, Jinpeng Hu, Jiamu Li, Zhitao Jing
Journal of Translational Medicine.2025;[Epub] CrossRef - Prognostic impact of Fusobacterium nucleatum on survival in colorectal cancer: A systematic review and meta-analysis
Tianyu Wang, Shengcheng Lin, Yong Ji, Ciren Puqiong, Jidong Gao, Shuluan Li
Journal of Cancer Research and Therapeutics.2025; 21(4): 796. CrossRef - Fusobacterium nucleatum in Health and Disease
Xinyi Yang, Shutian Zhang, Tingting Ning, Jing Wu
MedComm.2025;[Epub] CrossRef - Periodontitis and Oral Pathogens in Colorectal Cancer: A Systematic Review, Meta-Analysis, and Trial Sequential Analysis
Luis Chauca-Bajaña, Andrea Ordoñez Balladares, Alejandro Ismael Lorenzo-Pouso, Rosangela Caicedo-Quiroz, Rafael Xavier Erazo Vaca, Rolando Fabricio Dau Villafuerte, Yajaira Vanessa Avila-Granizo, Carlos Hans Salazar Minda, Miguel Amador Salavarria Vélez,
Dentistry Journal.2025; 13(12): 595. CrossRef - Composition of the colon microbiota in the individuals with inflammatory bowel disease and colon cancer
Ceren Acar, Sibel Kucukyildirim Celik, H. Ozgur Ozdemirel, Beril Erdem Tuncdemir, Saadet Alan, Hatice Mergen
Folia Microbiologica.2024; 69(2): 333. CrossRef - Intratumoral microorganisms in tumors of the digestive system
Mengjuan Xuan, Xinyu Gu, Yingru Liu, Li Yang, Yi Li, Di Huang, Juan Li, Chen Xue
Cell Communication and Signaling.2024;[Epub] CrossRef - Prognostic impact of oral microbiome on survival of malignancies: a systematic review and meta-analysis
Shuluan Li, Tianyu Wang, Ya Ren, Zhou Liu, Jidong Gao, Zhi Guo
Systematic Reviews.2024;[Epub] CrossRef - Exploring the Potential of Humoral Immune Response to Commensal Bifidobacterium as a Biomarker for Human Health, including Both Malignant and Non-Malignant Diseases: A Perspective on Detection Strategies and Future Directions
Kyogo Itoh, Satoko Matsueda
Biomedicines.2024; 12(4): 803. CrossRef - Unveiling intratumoral microbiota: An emerging force for colorectal cancer diagnosis and therapy
Jinjing Zhang, Penghui Wang, Jiafeng Wang, Xiaojie Wei, Mengchuan Wang
Pharmacological Research.2024; 203: 107185. CrossRef - Spatial transcriptomic analysis reveals local effects of intratumoral fusobacterial infection on DNA damage and immune signaling in rectal cancer
William P. Duggan, Batuhan Kisakol, Ina Woods, Mohammedreza Azimi, Heiko Dussmann, Joanna Fay, Tony O’Grady, Barry Maguire, Ian S. Reynolds, Manuela Salvucci, Daniel J. Slade, Deborah A. McNamara, John P. Burke, Jochen H.M. Prehn
Gut Microbes.2024;[Epub] CrossRef - Gut microbiota characteristics of colorectal cancer patients in Hubei, China, and differences with cohorts from other Chinese regions
Jianguo Shi, Hexiao Shen, Hui Huang, Lifang Zhan, Wei Chen, Zhuohui Zhou, Yongling Lv, Kai Xiong, Zhiwei Jiang, Qiyi Chen, Lei Liu
Frontiers in Microbiology.2024;[Epub] CrossRef - The role of Fusobacterium nucleatum in cancer and its implications for clinical applications
Wanyi Luo, Juxi Han, Xian Peng, Xuedong Zhou, Tao Gong, Xin Zheng
Molecular Oral Microbiology.2024; 39(6): 417. CrossRef - Gut Microbiome and colorectal cancer: discovery of bacterial changes with metagenomics application in Turkısh population
Yakup Ulger, Anıl Delik, Hikmet Akkız
Genes & Genomics.2024; 46(9): 1059. CrossRef - Intratumoral Microbiota: Metabolic Influences and Biomarker Potential in Gastrointestinal Cancer
Xueyuan Bi, Jihan Wang, Cuicui Liu
Biomolecules.2024; 14(8): 917. CrossRef - Intratumoral Microbiota: Insights from Anatomical, Molecular, and Clinical Perspectives
Claudia Lombardo, Rosanna Fazio, Marta Sinagra, Giuseppe Gattuso, Federica Longo, Cinzia Lombardo, Mario Salmeri, Guido Nicola Zanghì, Carla Agata Erika Loreto
Journal of Personalized Medicine.2024; 14(11): 1083. CrossRef - Exploring the role of Fusobacterium nucleatum in colorectal cancer: implications for tumor proliferation and chemoresistance
Leila Dadgar-Zankbar, Zahra Elahi, Aref Shariati, Azad Khaledi, Shabnam Razavi, Amin Khoshbayan
Cell Communication and Signaling.2024;[Epub] CrossRef - Fusobacterium nucleatum Abundance is Associated with Cachexia in Colorectal Cancer Patients: The ColoCare Study
Mmadili N. Ilozumba, Tengda Lin, Sheetal Hardikar, Doratha A. Byrd, June L. Round, W. Zac Stephens, Andreana N. Holowatyj, Christy A. Warby, Victoria Damerell, Christopher I. Li, Jane C. Figueiredo, Adetunji T. Toriola, David Shibata, Gary C. Fillmore, Ba
Cancer Medicine.2024;[Epub] CrossRef - Intratumoral microbiota: roles in cancer initiation, development and therapeutic efficacy
Li Yang, Aitian Li, Ying Wang, Yi Zhang
Signal Transduction and Targeted Therapy.2023;[Epub] CrossRef - Increased Fusobacterium tumoural abundance affects immunogenicity in mucinous colorectal cancer and may be associated with improved clinical outcome
William P. Duggan, Manuela Salvucci, Batuhan Kisakol, Andreas U. Lindner, Ian S. Reynolds, Heiko Dussmann, Joanna Fay, Tony O’Grady, Daniel B. Longley, Fiona Ginty, Elizabeth Mc Donough, Daniel J. Slade, John P. Burke, Jochen H. M. Prehn
Journal of Molecular Medicine.2023; 101(7): 829. CrossRef -
Fusobacterium nucleatum Load Correlates with KRAS Mutation and Sessile Serrated Pathogenesis in Colorectal Adenocarcinoma
Koki Takeda, Minoru Koi, Yoshiki Okita, Sija Sajibu, Temitope O. Keku, John M. Carethers
Cancer Research Communications.2023; 3(9): 1940. CrossRef - La asociación entre Fusobacterium nucleatum y el cáncer colorrectal: una revisión sistemática y metaanálisis
Paola Villar-Ortega, Manuela Expósito-Ruiz, Miguel Gutiérrez-Soto, Miguel Ruiz-Cabello Jiménez, José María Navarro-Marí, José Gutiérrez-Fernández
Enfermedades Infecciosas y Microbiología Clínica.2022; 40(5): 224. CrossRef - The association between Fusobacterium nucleatum and cancer colorectal: A systematic review and meta-analysis
Paola Villar-Ortega, Manuela Expósito-Ruiz, Miguel Gutiérrez-Soto, Miguel Ruiz-Cabello Jiménez, José María Navarro-Marí, José Gutiérrez-Fernández
Enfermedades infecciosas y microbiologia clinica (English ed.).2022; 40(5): 224. CrossRef - Suppression of Berberine and Probiotics (in vitro and in vivo) on the Growth of Colon Cancer With Modulation of Gut Microbiota and Butyrate Production
Chao Huang, Ying Sun, Sheng-rong Liao, Zhao-xin Chen, Han-feng Lin, Wei-zeng Shen
Frontiers in Microbiology.2022;[Epub] CrossRef - Prognostic and clinicopathological significance of Fusobacterium nucleatum in colorectal cancer: a systemic review and meta-analysis
Younghoon Kim, Nam Yun Cho, Gyeong Hoon Kang
Journal of Pathology and Translational Medicine.2022; 56(3): 144. CrossRef - Iron accelerates Fusobacterium nucleatum–induced CCL8 expression in macrophages and is associated with colorectal cancer progression
Taishi Yamane, Yohei Kanamori, Hiroshi Sawayama, Hiromu Yano, Akihiro Nita, Yudai Ohta, Hironori Hinokuma, Ayato Maeda, Akiko Iwai, Takashi Matsumoto, Mayuko Shimoda, Mayumi Niimura, Shingo Usuki, Noriko Yasuda-Yoshihara, Masato Niwa, Yoshifumi Baba, Taka
JCI Insight.2022;[Epub] CrossRef - Clinicopathological differences of high Fusobacterium nucleatum levels in colorectal cancer: A review and meta-analysis
Yi Wang, Yuting Wen, Jiayin Wang, Xin Lai, Ying Xu, Xuanping Zhang, Xiaoyan Zhu, Chenglin Ruan, Yao Huang
Frontiers in Microbiology.2022;[Epub] CrossRef - Clinical Significance of Fusobacterium nucleatum and Microsatellite Instability in Evaluating Colorectal Cancer Prognosis
Yanxuan Xie, Xiaoyang Jiao, Mi Zeng, Zhiqiang Fan, Xin Li, Yumeng Yuan, Qiaoxin Zhang, Yong Xia
Cancer Management and Research.2022; Volume 14: 3021. CrossRef - Influence of the Microbiome Metagenomics and Epigenomics on Gastric Cancer
Precious Mathebela, Botle Precious Damane, Thanyani Victor Mulaudzi, Zilungile Lynette Mkhize-Khwitshana, Guy Roger Gaudji, Zodwa Dlamini
International Journal of Molecular Sciences.2022; 23(22): 13750. CrossRef - Circulating IgA Antibodies Against Fusobacterium nucleatum Amyloid Adhesin FadA are a Potential Biomarker for Colorectal Neoplasia
Jung Eun Baik, Li Li, Manish A. Shah, Daniel E. Freedberg, Zhezhen Jin, Timothy C. Wang, Yiping W. Han
Cancer Research Communications.2022; 2(11): 1497. CrossRef - Differential immune microenvironmental features of microsatellite-unstable colorectal cancers according to Fusobacterium nucleatum status
Ji Ae Lee, Seung-Yeon Yoo, Hyeon Jeong Oh, Seorin Jeong, Nam-Yun Cho, Gyeong Hoon Kang, Jung Ho Kim
Cancer Immunology, Immunotherapy.2021; 70(1): 47. CrossRef - Fusobacterium nucleatum and Clinicopathologic Features of Colorectal Cancer: Results From the ColoCare Study
Yannick Eisele, Patrick M. Mallea, Biljana Gigic, W. Zac Stephens, Christy A. Warby, Kate Buhrke, Tengda Lin, Juergen Boehm, Petra Schrotz-King, Sheetal Hardikar, Lyen C. Huang, T. Bartley Pickron, Courtney L. Scaife, Richard Viskochil, Torsten Koelsch, A
Clinical Colorectal Cancer.2021; 20(3): e165. CrossRef - Role of gut microbiota in epigenetic regulation of colorectal Cancer
Yinghui Zhao, Chuanxin Wang, Ajay Goel
Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.2021; 1875(1): 188490. CrossRef - Fusobacterium nucleatum: caution with interpreting historical patient sample cohort
Kate L. F. Johnstone, Sinead Toomey, Stephen Madden, Brian D. P. O’Neill, Bryan T Hennessy
Journal of Pathology and Translational Medicine.2021; 55(6): 415. CrossRef -
Fusobacterium nucleatum colonization is associated with decreased survival of helicobacter pylori-positive gastric cancer patients
Yung-Yu Hsieh, Shui-Yi Tung, Hung-Yu Pan, Te-Sheng Chang, Kuo-Liang Wei, Wei-Ming Chen, Yi-Fang Deng, Chung-Kuang Lu, Yu-Hsuan Lai, Cheng-Shyong Wu, Chin Li
World Journal of Gastroenterology.2021; 27(42): 7311. CrossRef - Analysis of changes in microbiome compositions related to the prognosis of colorectal cancer patients based on tissue-derived 16S rRNA sequences
Sukjung Choi, Jongsuk Chung, Mi-La Cho, Donghyun Park, Sun Shim Choi
Journal of Translational Medicine.2021;[Epub] CrossRef - Gastrointestinal tumors and infectious agents: A wide field to explore
Miriam López-Gómez, Belén García de Santiago, Pedro-David Delgado-López, Eduardo Malmierca, Jesús González-Olmedo, César Gómez-Raposo, Carmen Sandoval, Pilar Ruiz-Seco, Nora Escribano, Jorge Francisco Gómez-Cerezo, Enrique Casado
World Journal of Meta-Analysis.2021; 9(6): 505. CrossRef - Gut Microbiota Profiles in Early- and Late-Onset Colorectal Cancer: A Potential Diagnostic Biomarker in the Future
Murdani Abdullah, Ninik Sukartini, Saskia Aziza Nursyirwan, Rabbinu Rangga Pribadi, Hasan Maulahela, Amanda Pitarini Utari, Virly Nanda Muzellina, Agustinus Wiraatmadja, Kaka Renaldi
Digestion.2021; 102(6): 823. CrossRef - The effect of periodontal bacteria infection on incidence and prognosis of cancer
Li Xiao, Qianyu Zhang, Yanshuang Peng, Daqing Wang, Ying Liu
Medicine.2020; 99(15): e19698. CrossRef - The impact of the gut microbiota on prognosis after surgery for colorectal cancer – a systematic review and meta‐analysis
Emilie Palmgren Colov, Thea Helene Degett, Hans Raskov, Ismail Gögenur
APMIS.2020; 128(2): 162. CrossRef - Can the microbiota predict response to systemic cancer therapy, surgical outcomes, and survival? The answer is in the gut
Khalid El Bairi, Rachid Jabi, Dario Trapani, Hanae Boutallaka, Bouchra Ouled Amar Bencheikh, Mohammed Bouziane, Mariam Amrani, Said Afqir, Adil Maleb
Expert Review of Clinical Pharmacology.2020; 13(4): 403. CrossRef - Predictive Values of Colon Microbiota in the Treatment Response to Colorectal Cancer
Jorge Galan-Ros, Verónica Ramos-Arenas, Pablo Conesa-Zamora
Pharmacogenomics.2020; 21(14): 1045. CrossRef - The gut microbiome and potential implications for early-onset colorectal cancer
Reetu Mukherji, Benjamin A Weinberg
Colorectal Cancer.2020;[Epub] CrossRef -
Fusobacterium nucleatum in the Colorectum and Its Association with Cancer Risk and Survival: A Systematic Review and Meta-analysis
Christian Gethings-Behncke, Helen G. Coleman, Haydee W.T. Jordao, Daniel B. Longley, Nyree Crawford, Liam J. Murray, Andrew T. Kunzmann
Cancer Epidemiology, Biomarkers & Prevention.2020; 29(3): 539. CrossRef - CpG Island Methylation in Sessile Serrated Adenoma/Polyp of the Colorectum: Implications for Differential Diagnosis of Molecularly High-Risk Lesions among Non-dysplastic Sessile Serrated Adenomas/Polyps
Ji Ae Lee, Hye Eun Park, Seung-Yeon Yoo, Seorin Jeong, Nam-Yun Cho, Gyeong Hoon Kang, Jung Ho Kim
Journal of Pathology and Translational Medicine.2019; 53(4): 225. CrossRef - Fusobacterium nucleatum tumor DNA levels are associated with survival in colorectal cancer patients
Andrew T. Kunzmann, Marcela Alcântara Proença, Haydee WT Jordao, Katerina Jiraskova, Michaela Schneiderova, Miroslav Levy, Václav Liska, Tomas Buchler, Ludmila Vodickova, Veronika Vymetalkova, Ana Elizabete Silva, Pavel Vodicka, David J. Hughes
European Journal of Clinical Microbiology & Infectious Diseases.2019; 38(10): 1891. CrossRef - Gut Microbiome: A Promising Biomarker for Immunotherapy in Colorectal Cancer
Sally Temraz, Farah Nassar, Rihab Nasr, Maya Charafeddine, Deborah Mukherji, Ali Shamseddine
International Journal of Molecular Sciences.2019; 20(17): 4155. CrossRef - The Four Horsemen in Colon Cancer
Marco Antonio Hernández-Luna, Sergio López-Briones, Rosendo Luria-Pérez
Journal of Oncology.2019; 2019: 1. CrossRef - The role of Fusobacterium nucleatum in colorectal cancer: from carcinogenesis to clinical management
Chun‐Hui Sun, Bin‐Bin Li, Bo Wang, Jing Zhao, Xiao‐Ying Zhang, Ting‐Ting Li, Wen‐Bing Li, Di Tang, Miao‐Juan Qiu, Xin‐Cheng Wang, Cheng‐Ming Zhu, Zhi‐Rong Qian
Chronic Diseases and Translational Medicine.2019; 5(3): 178. CrossRef
- Microbiota and tumor epigenetics: deep interconnections and emerging therapeutic perspectives
- Perivascular Epithelioid Cell Tumor in the Stomach
- Sun Ah Shin, Jiwoon Choi, Kyung Chul Moon, Woo Ho Kim
- J Pathol Transl Med. 2017;51(4):428-432. Published online April 4, 2017
- DOI: https://doi.org/10.4132/jptm.2016.09.16
- 9,934 View
- 141 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Perivascular epithelioid cell tumors or PEComas can arise in any location in the body. However, a limited number of cases of gastric PEComa have been reported. We present two cases of gastric PEComas. The first case involved a 62-year-old woman who presented with a 4.2 cm gastric subepithelial mass in the prepyloric antrum, and the second case involved a 67-year-old man with a 5.0 cm mass slightly below the gastroesophageal junction. Microscopic examination revealed that both tumors were composed of perivascular epithelioid cells that were immunoreactive for melanocytic and smooth muscle markers. Prior to surgery, the clinical impression of both tumors was gastrointestinal stromal tumor (GIST), and the second case was erroneously diagnosed as GIST even after microscopic examination. Although gastric PEComa is a very rare neoplasm, it should be considered in the differential diagnosis of gastric submucosal lesions.
-
Citations
Citations to this article as recorded by- A Perivascular Epithelioid Cell Tumor in the Ascending Colon: A Rare Case Involving a Patient With Tuberous Sclerosis
Kai Seharada, Masato Kitazawa, Satoshi Nakamura, Yuta Yamamoto, Yuji Soejima
Cureus.2025;[Epub] CrossRef - Malignant Perivascular Epithelioid Cell Tumor of Ovary: A Rare Case Report
Anuradha Sharma, Reetika Sharma, Jyoti Bala, Monika Sharma
Journal of Mid-life Health.2025; 16(1): 107. CrossRef - Unusual paediatric sigmoid perivascular epithelioid cell tumour with regional lymph node metastasis treated using gemcitabine and docetaxel: a case report and literature review
Hsiu-Chung Cheng, Chia-Yu Kuo, Ching-Wen Huang, Hsiang-Hung Shih, Chih-Hung Lin, Jaw-Yuan Wang
Journal of International Medical Research.2021;[Epub] CrossRef - Gastric Perivascular Epithelioid Cell Tumor (PEComa)
Jinghong Xu, Yu Yan, Xueping Xiang, Peter Jiang, Xiangrong Hu, Wenjun Yang
American Journal of Clinical Pathology.2019; 152(2): 221. CrossRef - Robotic wedge resection of a rare gastric perivascular epithelioid cell tumor: A case report
Alessandra Marano, Francesca Maione, Yanghee Woo, Luca Pellegrino, Paolo Geretto, Diego Sasia, Mirella Fortunato, Giulio Fraternali Orcioni, Roberto Priotto, Renato Fasoli, Felice Borghi
World Journal of Clinical Cases.2019; 7(23): 4011. CrossRef
- A Perivascular Epithelioid Cell Tumor in the Ascending Colon: A Rare Case Involving a Patient With Tuberous Sclerosis
- PHH3 as an Ancillary Mitotic Marker in Gastrointestinal Stromal Tumors
- Yooju Shin, Jiyeon Hyeon, Boram Lee, Sang Yun Ha, Min Eui Hong, In Gu Do, Kyoung-Mee Kim
- J Pathol Transl Med. 2015;49(1):23-29. Published online January 15, 2015
- DOI: https://doi.org/10.4132/jptm.2014.10.08
- 11,302 View
- 81 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Counting mitoses is subjective and time-consuming. The adjunctive diagnostic utility of a recently reported mitotic marker, phosphohistone H3 (PHH3), was investigated in gastrointestinal stromal tumors (GISTs). Methods: We reviewed 77 GISTs for several proliferative indices. These included the mitotic count per 50 high power fields (HPFs), the immunohistochemical Ki- 67 labeling index and the immunohistochemical PHH3 mitotic index (MI). For comparison, Spearman’s rank correlation and interclass correlation coefficient were used. Results: Mitotic counts ranged from 0–138 (mean, 7.57±2.34) and the PHH3 MI ranged from 0–126 per 50 HPFs (mean, 9.61±2.27). We found a positive correlation between mitotic counts and PHH3 MI (r=0.810, p<.001). The inter-observer correlation coefficient for three participants was 0.975 for mitotic counts and 0.940 for the PHH3 MI. When using the PHH3 MI instead of mitotic counts in the Armed Forces Institute of Pathology (AFIP) stratification criteria, 10 cases were reclassified. In one patient with a mitotic count of 2 and a PHH3 MI of 6 per 50 HPFs, distant metastasis occurred. Conclusions: In GISTs, the PHH3 MI correlated adequately with mitotic counts and can be used as a useful adjunctive to count mitotic figures efficiently. -
Citations
Citations to this article as recorded by- Potential of Proliferative Markers in Pancreatic Cancer Management: A Systematic Review
Aryan Salahi‐Niri, Paniz Zarand, Negar Mansouri, Parvaneh Rastgou, Omid Yazdani, Romina Esbati, Fatemeh Shojaeian, Behnaz Jahanbin, Zhaleh Mohsenifar, Hamid Asadzadeh Aghdaei, Farid Azmoudeh Ardalan, Seyed Amir Ahmad Safavi‐Naini
Health Science Reports.2025;[Epub] CrossRef - A retrospective study on expression and clinical significance of PHH3, Ki67 and P53 in bladder exophytic papillary urothelial neoplasms
Gaoxiu Qi, Jinmeng Liu, Shuqi Tao, Wenyuan Fan, Haoning Zheng, Meihong Wang, Hanchao Yang, Yongting Liu, Huancai Liu, Fenghua Zhou
PeerJ.2023; 11: e15675. CrossRef - Loss of Slfn3 induces a sex-dependent repair vulnerability after 50% bowel resection
Emilie E. Vomhof-DeKrey, Jack T. Lansing, Diane C. Darland, Josey Umthun, Allie D. Stover, Christopher Brown, Marc D. Basson
American Journal of Physiology-Gastrointestinal and Liver Physiology.2021; 320(2): G136. CrossRef - Phosphohistone H3 (PHH3) as a surrogate of mitotic figure count for grading in meningiomas: a comparison of PHH3 (S10) versus PHH3 (S28) antibodies
Napaporn Puripat, Kongsak Loharamtaweethong
Virchows Archiv.2019; 474(1): 87. CrossRef - Gastrointestinal Stromal Tumors Risk Stratification Utilizing Phospho-Histone H3 Evaluated by Manual Counting and Computer-Assisted Image Analysis
Cao Jin, Yan Huang, Mansoor Nasim, Yihe Yang, Lili Lee
International Journal of Surgical Pathology.2019; 27(7): 706. CrossRef - The utility of phosphohistone H3 in early prediction of benign and borderline phyllodes tumor recurrence
AymenM El-Saka, MohamedA Mlees, YomnaA Zamzam
Egyptian Journal of Pathology.2019; 39(2): 402. CrossRef - Identification of Phosphohistone H3 Cutoff Values Corresponding to Original WHO Grades but Distinguishable in Well-Differentiated Gastrointestinal Neuroendocrine Tumors
Min Jeong Kim, Mi Jung Kwon, Ho Suk Kang, Kyung Chan Choi, Eun Sook Nam, Seong Jin Cho, Hye-Rim Park, Soo Kee Min, Jinwon Seo, Ji-Young Choe, Hyoung-Chul Park
BioMed Research International.2018; 2018: 1. CrossRef - Tumor Digital Masking Allows Precise Patient Triaging: A Study Based on Ki-67 Scoring in Gastrointestinal Stromal Tumors
Piotr Lewitowicz, Jaroslaw Matykiewicz, Magdalena Chrapek, Dorota Koziel, Agata Horecka-Lewitowicz, Martyna Gluszek-Osuch, Iwona Wawrzycka, Stanisław Gluszek
Scanning.2018; 2018: 1. CrossRef - The mitosis‐specific marker phosphohistone‐H3 (PHH3) is an independent prognosticator in uterine smooth muscle tumours: an outcome‐based study
Kin‐Long Chow, Ka‐Yu Tse, Ching‐Lung Cheung, Ka‐Wing Wong, Annie N Y Cheung, Richard W C Wong, Alice N H Chan, Nancy W F Yuen, Hextan Y S Ngan, Philip P C Ip
Histopathology.2017; 70(5): 746. CrossRef
- Potential of Proliferative Markers in Pancreatic Cancer Management: A Systematic Review
- Update on the Proposal for Creating a Guideline for Cancer Registration of the Gastrointestinal Tumors (I-2)
- Eun Sun Jung, Yun Kyung Kang, Mee-Yon Cho, Joon Mee Kim, Won Ae Lee, Hee Eun Lee, Sunhoo Park, Jin Hee Sohn, So-Young Jin
- Korean J Pathol. 2012;46(5):443-453. Published online October 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.5.443
- 12,086 View
- 188 Download
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Cancer registries play a fundamental role in cancer control and multicenter collaborative research. Recently, the need for reassessment of cancer registry criteria has arisen due to the newly released 2010 World Health Organization (WHO) classification. Accordingly, development of new coding guidelines for cancer is necessary to improve the quality of cancer registries, as well as to prevent conflicts that may arise when seeking medical insurance compensation.
Methods With funding from the Management Center for Health Promotion, 35 members of the Gastrointestinal Pathology Study Group and the Cancer Registration Committee of the Korean Society of Pathologists (KSP) participated in a second workshop for gastrointestinal tumor registration in Korea.
Results The topics of gastric epithelial tumor, colonic intramucosal carcinoma, neuroendocrine tumor (NET), gastrointestinal stromal tumor (GIST) and appendiceal mucinous tumor were discussed for new coding guidelines. A survey was then conducted among 208 members of the KSP for a consensus of the guidelines proposed in the workshop.
Conclusions Although a few issues were set aside for further discussion, such as coding for non-gastric GIST and some types of NET, the members agreed upon most of the proposed guidelines. Therefore, we suggest using the newly revised International Classification of Diseases for Oncology, 3rd edition (ICD-O-3) coding guidelines for registering gastrointestinal tumors in Korea.
-
Citations
Citations to this article as recorded by- Gastrointestinal Stromal Tumor: History, Molecular Subtypes, and Risk Stratification
In Hye Song, Soomin Ahn, Hyung-Don Kim, Jeong-Hyeon Jo, Jinho Shin, Min-Hee Ryu, Young Soo Park
Journal of Gastric Cancer.2026;[Epub] CrossRef - Variation in mitotic counting and risk classification practices for gastrointestinal stromal tumors: a survey of pathologists in South Korea
In Hye Song, Soomin Ahn, Jeong-Hyeon Jo, Young Soo Park
Journal of Pathology and Translational Medicine.2025; 59(5): 348. CrossRef - Different miRNAs Related to FBXW7 Mutations or High Mitotic Indices Contribute to Rectal Neuroendocrine Tumors: A Pilot Study
Ho Suk Kang, Ha Young Park, Hyun Lim, Il Tae Son, Min-Jeong Kim, Nan Young Kim, Min Jeong Kim, Eun Sook Nam, Seong Jin Cho, Mi Jung Kwon
International Journal of Molecular Sciences.2023; 24(7): 6329. CrossRef - Clinicopathologic Impact of Peptide Hormonal Expression in Rectal Neuroendocrine Tumors
Jisup Kim, Dong-Hoon Yang, HaeSung Jung, HyungJun Cho, Hyeung-Jin Jang, Changhoon Yoo, In Ja Park, Baek-Yeol Ryoo, Jin-Sook Ryu, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2023; 147(7): 797. CrossRef - Prognostic nomogram and novel risk-scoring system for small cell lung cancer with different patterns of metastases
Hongli Ruan, Huali Sun, Yu Guo, Yan Ding, Yanmei Liu, Shenpeng Ying, Peipei Lin
General Thoracic and Cardiovascular Surgery.2022; 70(12): 1022. CrossRef - Development of a nomogram model to predict survival outcomes in patients with primary hepatic neuroendocrine tumors based on SEER database
Ziteng Zhang, Xin Zhao, Zhiyan Li, Youchun Wu, Yao Liu, Zhiwei Li, Guobao Li
BMC Cancer.2021;[Epub] CrossRef - Standardization of the pathologic diagnosis of appendiceal mucinous neoplasms
Dong-Wook Kang, Baek-hui Kim, Joon Mee Kim, Jihun Kim, Hee Jin Chang, Mee Soo Chang, Jin-Hee Sohn, Mee-Yon Cho, So-Young Jin, Hee Kyung Chang, Hye Seung Han, Jung Yeon Kim, Hee Sung Kim, Do Youn Park, Ha Young Park, So Jeong Lee, Wonae Lee, Hye Seung Lee,
Journal of Pathology and Translational Medicine.2021; 55(4): 247. CrossRef - Analysis of the Incidence and Clinical Features of Colorectal Nonadenocarcinoma in Korea: A National Cancer Registry-Based Study
Soomin Nam, Dongwook Kim, Kyuwon Jung, Yoon Jung Choi, Jung Gu Kang
Annals of Coloproctology.2020; 36(6): 390. CrossRef - Novel Finding of Paired Box 5 (PAX5) Cytoplasmic Staining in Well-differentiated Rectal Neuroendocrine Tumors (Carcinoids) and Its Diagnostic and Potentially Prognostic Utility
Zhiyan Fu, Chunlai Zuo, Christine E. Sheehan, Deepa T. Patil, Jingmei Lin, Zhaohai Yang, Hwajeong Lee
Applied Immunohistochemistry & Molecular Morphology.2019; 27(6): 454. CrossRef - Lymphovascular invasion as a prognostic value in small rectal neuroendocrine tumor treated by local excision: A systematic review and meta-analysis
Ho Suk Kang, Mi Jung Kwon, Tae-Hwan Kim, Junhee Han, Young-Su Ju
Pathology - Research and Practice.2019; 215(11): 152642. CrossRef - Management Colorectal Gastrointestinal Stromal Tumors (Gists) in Surabaya
Yuda Handaya, Sutamto Wibowo, Iwan Kristian
Open Journal of Gastroenterology.2016; 06(04): 97. CrossRef - Non-L-cell Immunophenotype and Large Tumor Size in Rectal Neuroendocrine Tumors Are Associated With Aggressive Clinical Behavior and Worse Prognosis
Joo Young Kim, Ki-Suk Kim, Kyung-Jo Kim, In Ja Park, Jong Lyul Lee, Seung-Jae Myung, Yangsoon Park, Young Soo Park, Chang Sik Yu, Jin Cheon Kim, Eunsil Yu, Hyeung-Jin Jang, Seung-Mo Hong
American Journal of Surgical Pathology.2015; 39(5): 632. CrossRef - Diagnostic Coding for Intramucosal Carcinoma and Neuroendocrine Tumor in the Colorectum: Proposal for Avoiding Confusing Coding in Korea
Dong Soo Han, Jin Hee Sohn, Jeong-Sik Byeon, Hwang Choi, Joon Mee Kim
Clinical Endoscopy.2015; 48(3): 216. CrossRef - Prognostic Significance of Defining L-Cell Type on the Biologic Behavior of Rectal Neuroendocrine Tumors in Relation with Pathological Parameters
Jin Hee Sohn, Mee-Yon Cho, Yangsoon Park, Hyunki Kim, Woo Ho Kim, Joon Mee Kim, Eun Sun Jung, Kyoung-Mee Kim, Jae Hyuk Lee, Hee Kyung Chan, Do Youn Park, Mee Joo, Sujin Kim, Woo Sung Moon, Mi Seon Kang, So-Young Jin, Yun Kyung Kang, Sun Och Yoon, HyeSeung
Cancer Research and Treatment.2015; 47(4): 813. CrossRef - Diminutive and Small Colorectal Polyps: The Pathologist's Perspective
Yun Kyung Kang
Clinical Endoscopy.2014; 47(5): 404. CrossRef - Highlights from the 50th Seminar of the Korean Society of Gastrointestinal Endoscopy
Eun Young Kim, Il Ju Choi, Kwang An Kwon, Ji Kon Ryu, Seok Ho Dong, Ki Baik Hahm
Clinical Endoscopy.2014; 47(4): 285. CrossRef - Early Colorectal Epithelial Neoplasm in Korea: A Multicenter Survey of Pathologic Diagnosis
Yun Kyung Kang, So-Young Jin, Mee Soo Chang, Jung Yeon Kim, Gyeong Hoon Kang, Hye Seung Lee, Jin Hee Sohn, Ho Sung Park, Kye Won Kwon, Mi Jin Gu, Young Hee Maeng, Jong Eun Joo, Haeng Ji Kang, Hee Kyung Kim, Kee-Taek Jang, Mi Ja Lee, Hee Kyung Chang, Joon
Korean Journal of Pathology.2013; 47(3): 245. CrossRef - Expression of metallothionein‐1 and metallothionein‐2 as a prognostic marker in hepatocellular carcinoma
Yangsoon Park, Eunsil Yu
Journal of Gastroenterology and Hepatology.2013; 28(9): 1565. CrossRef
- Gastrointestinal Stromal Tumor: History, Molecular Subtypes, and Risk Stratification
- CpG Island Hypermethylation in Gastric Carcinoma and Its Premalignant Lesions
- Gyeong Hoon Kang
- Korean J Pathol. 2012;46(1):1-9. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.1
- 11,048 View
- 50 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Gastric cancers arise through a multistep process characterized by the progressive accumulation of molecular alterations in which genetic and epigenetic mechanisms have been implicated. Gastric cancer is one of the human malignancies in which aberrant promoter CpG island hypermethylation is frequently found.
Helicobacter pylori and Epstein-Barr virus, which are known carcinogens for gastric cancer, are closely associated with enhanced hypermethylation of CpG island loci in gastric non-neoplastic epithelial cells and cancer cells, respectively. Aberrant CpG island hypermethylation occurs early in the multistep cascade of gastric carcinogenesis and tends to increase with the step-wise progression of the lesion. Approximately 400 genes that are actively expressed in normal gastric epithelial cells are estimated to be inactivated in gastric cancers as a result of promoter CpG island hypermethylation. In this review, a variety of information is summarized regarding CpG island hypermethylation in gastric cancer.-
Citations
Citations to this article as recorded by- Pathogenicity of Helicobacter pylori-associated gastric cancer
Shamshul Ansari, Nada Ahmed
World Journal of Clinical Oncology.2025;[Epub] CrossRef - Genome-wide characterization of extrachromosomal circular DNA in gastric cancer and its potential role in carcinogenesis and cancer progression
Xianming Jiang, Xiaoguang Pan, Wenchao Li, Peng Han, Jiaying Yu, Jing Li, Haoran Zhang, Wei Lv, Ying Zhang, Yulong He, Xi Xiang
Cellular and Molecular Life Sciences.2023;[Epub] CrossRef - Analysis of DNA methylation in endometrial biopsies to predict risk of endometrial cancer
Francesco Multinu, Jun Chen, Joseph D. Madison, Michelle Torres, Jvan Casarin, Daniel Visscher, Viji Shridhar, Jamie Bakkum-Gamez, Mark Sherman, Nicolas Wentzensen, Andrea Mariani, Marina Walther-Antonio
Gynecologic Oncology.2020; 156(3): 682. CrossRef - Helicobacter pylori severely reduces expression of DNA repair proteins PMS2 and ERCC1 in gastritis and gastric cancer
Yasir Raza, Ayaz Ahmed, Adnan Khan, Arif Ali Chishti, Syed Shakeel Akhter, Muhammad Mubarak, Carol Bernstein, Beryl Zaitlin, Shahana Urooj Kazmi
DNA Repair.2020; 89: 102836. CrossRef - Genomic and Epigenomic Profiling of High-Risk Intestinal Metaplasia Reveals Molecular Determinants of Progression to Gastric Cancer
Kie Kyon Huang, Kalpana Ramnarayanan, Feng Zhu, Supriya Srivastava, Chang Xu, Angie Lay Keng Tan, Minghui Lee, Suting Tay, Kakoli Das, Manjie Xing, Aliya Fatehullah, Syed Muhammad Fahmy Alkaff, Tony Kiat Hon Lim, Jonathan Lee, Khek Yu Ho, Steven George Ro
Cancer Cell.2018; 33(1): 137. CrossRef -
Decreased Methylation of
IFNAR
Gene Promoter from Peripheral Blood Mononuclear Cells Is Associated with Oxidative Stress in Chronic Hepatitis B
Jing-wen Wang, Jing-wei Wang, Jun Zhang, Chen-si Wu, Yu Fang, Wei-wei Su, Yu-chen Fan, Kai Wang
Journal of Interferon & Cytokine Research.2018; 38(11): 480. CrossRef - Genomic landscape of gastric cancer: molecular classification and potential targets
Jiawei Guo, Weiwei Yu, Hui Su, Xiufeng Pang
Science China Life Sciences.2017; 60(2): 126. CrossRef - Hypermethylation of the galectin-3 promoter is associated with poor prognosis of acute-on-chronic hepatitis B liver failure
Jing Zhao, Yu-Chen Fan, Xin-Yuan Liu, Ze-Hua Zhao, Feng Li, Kai Wang
Digestive and Liver Disease.2017; 49(6): 664. CrossRef - Proteomics-Based Identification and Analysis of Proteins Associated with Helicobacter pylori in Gastric Cancer
Jianjiang Zhou, Wenling Wang, Yuan Xie, Yan Zhao, Xian Chen, Wenjie Xu, Yan Wang, Zhizhong Guan, Hiromu Suzuki
PLOS ONE.2016; 11(1): e0146521. CrossRef - Lack of Correlation between Aberrant p16, RAR-β2, TIMP3, ERCC1, and BRCA1 Protein Expression and Promoter Methylation in Squamous Cell Carcinoma Accompanying Candida albicans-Induced Inflammation
Yui Terayama, Tetsuro Matsuura, Kiyokazu Ozaki, Javier S Castresana
PLOS ONE.2016; 11(7): e0159090. CrossRef - Helicobacter pylori CagA induces tumor suppressor gene hypermethylation by upregulating DNMT1 via AKT-NFκB pathway in gastric cancer development
Bao-gui Zhang, Lei Hu, Ming-de Zang, He-xiao Wang, Wei Zhao, Jian-fang Li, Li-ping Su, Zhifeng Shao, Xiaodong Zhao, Zheng-gang Zhu, Min Yan, Bingya Liu
Oncotarget.2016; 7(9): 9788. CrossRef - Promoter methylation status and expression of PPAR-γ gene are associated with prognosis of acute-on-chronic hepatitis B liver failure
Ze-Hua Zhao, Yu-Chen Fan, Qi Zhao, Cheng-Yun Dou, Xiang-Fen Ji, Jing Zhao, Shuai Gao, Xin-You Li, Kai Wang
Clinical Epigenetics.2015;[Epub] CrossRef - Role of Epigenetics in EBV Regulation and Pathogenesis
Hans Helmut Niller, Zsófia Tarnai, Gábor Decsi, Ádám Zsedényi, Ferenc Bánáti, Janos Minarovits
Future Microbiology.2014; 9(6): 747. CrossRef - Helicobacter pylori Induces Hypermethylation of CpG Islands Through Upregulation of DNA Methyltransferase: Possible Involvement of Reactive Oxygen/Nitrogen Species
Hye-Kyung Na, Jeong-Hwa Woo
Journal of Cancer Prevention.2014; 19(4): 259. CrossRef - Mallory–Denk Body (MDB) formation modulates ufmylation expression epigenetically in alcoholic hepatitis (AH) and non-alcoholic steatohepatitis (NASH)
Hui Liu, Ming Gong, Barbara A. French, Jun Li, Brittany Tillman, Samuel W. French
Experimental and Molecular Pathology.2014; 97(3): 477. CrossRef - RETRACTED ARTICLE: Role of p16 gene promoter methylation in gastric carcinogenesis: a meta-analysis
He-Ling Wang, Ping-Yi Zhou, Peng Liu, Yu Zhang
Molecular Biology Reports.2014; 41(7): 4481. CrossRef - Exportin 4 gene expression and DNA promoter methylation status in chronic hepatitis B virus infection
F. Zhang, Y.‐C. Fan, N.‐N Mu, J. Zhao, F.‐K. Sun, Z.‐H. Zhao, S. Gao, K. Wang
Journal of Viral Hepatitis.2014; 21(4): 241. CrossRef - Microarray-based DNA methylation study of Ewing’s sarcoma of the bone
HYE-RIM PARK, WOON-WON JUNG, HYUN-SOOK KIM, YONG-KOO PARK
Oncology Letters.2014; 8(4): 1613. CrossRef - Pathologic Diagnosis of Gastric Intestinal Metaplasia
Nari Shin, Do Youn Park
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2013; 13(2): 84. CrossRef
- Pathogenicity of Helicobacter pylori-associated gastric cancer
- An Approach to Diagnosing Gastrointestinal Stromal Tumors Using Immunohistochemistry of c-kit and PDGFRA with Molecular Analysis.
- Jeong Shik Kim, Jae Hoon Kim, Hyun Jin Oh, In Soo Suh, Jong Gwang Kim, Byung Wook Kang, Wan Sik Yu, Ho Young Chung, Han Ik Bae
- Korean J Pathol. 2010;44(2):173-178.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.173
- 4,082 View
- 46 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors in the gastrointestinal tract. Recently, many methods for the diagnosis of GIST have been developed including molecular diagnosis.
METHODS
We selected 90 cases of GIST that had presented at Kyungpook National University Hospital between 1998 and 2007. Tissue microarrays were made using core areas of tumor tissues. Immunohistochemical staining for c-kit, protein kinase C-theta, and platelet-derived growth factor receptor alpha (PDGFRA) was done. Direct sequencing of hot spot exonal areas for c-kit and PDGFRA were done using extracted DNAs of all 90 paraffin block tissues.
RESULTS
Among the 90 cases, 83.3% (75/90) were c-kit positive, 16.6% (15/90) were c-kit negative, 93.3% (84/90) were PDGFRA positive, and 6.6% (6/90) cases were PDGFRA negative. Fifteen cases of c-kit negative GIST included 1 case of PDGFRA negative and 5 cases of PDGFRA negative GIST were ckit positive. The one case in which both c-kit and PDGFRA were negative, showed a c-kit mutation in exon 11.
CONCLUSIONS
Combined immunohistochemical staining of c-kit, discovered on GIST 1 (DOG1) and PDGFRA is helpful for the diagnosis of GIST. When all staining tests are negative for immunoreactivity, c-kit mutation analysis for exon 11, 9 should be done. Genotyping of kit and PDGFRA do not need to be examined initially, if it is only for the diagnosis of GIST.
- Histopathological Evaluation of Pediatric Intestinal Pseudo-Obstruction: Quantitative Morphometric Analysis of Pathological Changes in the Enteric Nervous System.
- Hyung Kyung Kim, Harin Cheong, Hanna Kang, Ji Yoon Bae, Dong Eun Song, Min Sun Cho, Sun Hee Sung, Woon Sup Han, Heasoo Koo
- Korean J Pathol. 2010;44(2):162-172.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.162
- 4,437 View
- 43 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was done to obtain comprehensive data on changes in the structural components of the enteric nervous system in pediatric patients with intestinal pseudo-obstruction (IPO). We evaluated routinely processed, in formalin-fixed tissues by quantitative morphometric analysis. In addition, we used formalin-fixed tissue to explore the possibility of using previously proposed diagnostic criteria to evaluate frozen serial sections for intestinal neuronal dysplasia (IND) type B and hypoganglionosis.
METHODS
We analyzed data for 19 IPO cases. Morphometric analysis for quantification of ganglia and ganglion cells (GCs) was done for the myentric and the submucous plexus. In addition, we determined the presence of immature GCs and the distribution of nerve fibers and interstitial cells of Cajal (ICC).
RESULTS
Nine patients showed combined hypoganglionosis, IND, and decreased ICC; others showed various combinations of these. Several morphometric factors were significantly different between patient groups as well as being different than the control group.
CONCLUSIONS
Our pediatric IPO cases showed extensive overlapping of pathological findings. And the findings suggest the utility of using previously proposed morphometrically measured factors in multiple frozen sections as diagnostic criteria for IND type B and hypoganglionosis in formalin-fixed tissue. -
Citations
Citations to this article as recorded by- Histomorphology of enteric neurons and enteric ganglia in different layers of human fetal colon
Chacchu Bhattarai, Phanindra P. Poudel, Arnab Ghosh, Sneha G. Kalthur
Journal of Taibah University Medical Sciences.2022; 17(4): 556. CrossRef - Diagnostic utility of Bcl-2 immunohistochemical expression in pediatric functional bowel obstruction cases with ganglionated specimens
Lobna Abd El Fattah Mohamed, Nedal Ahmed Hegazy, Faten Abd El Aziz Ghazal, Ahmed Mohy El Din Zaki, Ahmed Bassiouny Radwan, Sarah Adel Hakim
Annals of Pediatric Surgery.2022;[Epub] CrossRef - PTEN Immunohistochemistry
Simone Antunes Terra, Pedro Luiz Toledo de Arruda Lourenção,, Maria Aparecida Marchesan Rodrigues
Archives of Pathology & Laboratory Medicine.2022; 147(5): 577. CrossRef - Challenges in the diagnosis of intestinal neuronal dysplasia type B: A look beyond the number of ganglion cells
Simone Antunes Terra, Anderson Cesar Gonçalves, Pedro Luiz Toledo de Arruda Lourenção, Maria Aparecida Marchesan Rodrigues
World Journal of Gastroenterology.2021; 27(44): 7649. CrossRef - Morphometric profile of large intestinal neuronal plexuses in normal perinatal autopsies and Hirschsprung disease
H. Subramanian, B. A. Badhe, P. C. Toi, K. Sambandan
Neurogastroenterology & Motility.2017;[Epub] CrossRef
- Histomorphology of enteric neurons and enteric ganglia in different layers of human fetal colon
- Usefulness of DOG1 Expression in the Diagnosis of Gastrointestinal Stromal Tumors.
- Jun Mo Kim, Aeri Kim, Joon Hyuk Choi, Young Kyung Bae
- Korean J Pathol. 2010;44(2):141-148.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.141
- 7,212 View
- 82 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors in the gastrointestinal tract. Expression of KIT protein (CD117) is an important diagnostic criterion of GIST. However, about 5% of GISTs are CD117 negative. Discovered on GIST 1 (DOG1) was introduced recently as a promising marker for GIST. We tested this new antibody in 105 GISTs tissue specimens, including 6 cases of metastatic GISTs, to determine the usefulness of DOG1 expression in the diagnosis of GISTs.
METHODS
We performed immunohistochemical (IHC) staining for DOG1 and CD117 on tissue microarrays that included 70 gastric GISTs, 29 small intestinal GISTs, 6 metastatic GISTs, 14 gastric leiomyomas and 16 gastric schwannomas.
RESULTS
DOG1 was positive in 98.1% (103/105) of GISTs and CD117 was positive in 97.1% (102/105) of GISTs. Only 1 case was negative for both markers. Two (66.7%) out of 3 GISTs tested CD117 negative were tested DOG1 positive. All leiomyomas and schwannomas were negative for both DOG1 and CD117.
CONCLUSIONS
DOG1 was highly expressed in GIST including CD117 negative cases. Adding DOG1 testing to the IHC panel for diagnosing GIST will help to identify GIST patients who are CD117 negative but may otherwise benefit from targeted therapy. -
Citations
Citations to this article as recorded by- Gastrointestinal tract spindle cell tumors with interstitial cells of Cajal: Prevalence excluding gastrointestinal stromal tumors
So Jung Lee, Chung Su Hwang, Ahrong Kim, Kyungbin Kim, Kyung Un Choi
Oncology Letters.2016; 12(2): 1287. CrossRef
- Gastrointestinal tract spindle cell tumors with interstitial cells of Cajal: Prevalence excluding gastrointestinal stromal tumors
- Gastrointestinal Stromal Tumor of the Colon Mimicking Inflammatory Fibroid Polyp with a Novel 63 bp c-kit Deletion Mutation: A Case Report.
- In Gu Do, Cheol Keun Park, Sung Hyun Yoon, John Goldblum, Kyoung Mee Kim
- Korean J Pathol. 2009;43(4):374-377.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.374
- 3,631 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Colonic gastrointestinal stromal tumors (GISTs) are rare and behave aggressively compared to GISTs in other parts of the gastrointestinal tract. Therefore, accurate diagnosis of GISTs and their distinction from other mesenchymal tumors is important for proper patient management and follow-up. Herein, we present an unusual case of a colonic GIST mimicking an inflammatory fibroid polyp with a novel 63 bp deletion mutation in exon 11 of the c-kit gene, which has not previously been reported. The tumor consisted of loosely arranged spindle cells and many inflammatory cells scattered throughout the tumor. Immunohistochemically, the tumor cells were focally and weakly positive for c-kit and diffusely positive for CD34, but were negative for PKC-theta, SMA, S-100 protein, ALK-1, and desmin. Our case re-emphasizes the broad morphologic spectrum of GISTs.
- Morphological Features of Metastatic Gastrointestinal Stromal Tumors after Gleevec Treatment: Two Cases Report.
- Joon Hyuk Choi, Young Kyung Bae, Sun Kyo Song, Hong Jin Kim, Min Chul Shim, Kyung Hee Lee
- Korean J Pathol. 2009;43(4):368-373.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.368
- 3,619 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - We report two patients with metastatic gastrointestinal stromal tumors (GISTs) with a focus on the morphological features related to Gleevec treatment. In case 1, a 50-year-old woman presented with a 1.8 cm metastatic GIST in the liver after resection of a gastric GIST. Majority of the metastatic tumor showed fibrosis and hyalinization after 8 weeks of Gleevec treatment. CD117-positive cells were present in approximately 1% of the overall tumor. In case 2, a 2 cm and 14 cm metastatic liver masses were found in a 54-year-old man who had a rectal GIST. After 4 weeks of Gleevec treatment, metastatic tumors showed a decrease in size on CT scan. The metastatic tumors showed a decrease in number of tumor cells. The hemorrhage, cystic changes, necrosis, and fibrosis made up approximately 90% of the tumor. The morphological features related to Gleevec treatment are important for correct diagnosis and evaluation of tumor response and prognosis.
- The Expressions of E2F1 and p53 in Gastrointestinal Stromal Tumors and Their Prognostic Significance.
- Mi Jung Kwon, Eun Sook Nam, Seong Jin Cho, Hye Rim Park, Hyung Sik Shin, Jong Seok Lee, Chan Heun Park, Woon Geon Shin
- Korean J Pathol. 2009;43(3):212-220.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.3.212
- 4,758 View
- 34 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
E2F1 plays a critical role in the G1-to-S phase transition by inducing various genes that encode S phase-activating proteins and that modulate such diverse cellular functions as DNA synthesis, mitosis and apoptosis. The purpose of this study was to assess the E2F1 expression in relation to the clinicopathologic parameters and other tumor markers in gastrointestinal stromal tumors.
METHODS
Immunohistochemical stainings for obtaining the E2F1, p53, and Ki-67 labeling indices were performed on a tissue microarray of 72 gastrointestinal stromal tumor specimens. The clinicopathologic parameters that were analyzed including the risk grade system by Miettinen et al. and the disease-free survival (DFS) rate.
RESULTS
1) An E2F1 expression was correlated with a larger tumor size, a p53 expression and a shorter period of DFS (p=0.014, p=0.007, and p=0.039). 2) A p53 expression was significantly associated with a high risk grade, a larger tumor size, high mitotic counts and a shorter period of DFS (p=0.003, p=0.044, p<0.001, and p<0.0001). 3) A high-risk grade and the epithelioid type were significantly associated with a shorter period of DFS (p=0.0006 and p=0.0008).
CONCLUSIONS
E2F1, as well as p53, may be a potentially novel independent prognostic factor for predicting a worse outcome for those patients suffering with Gastrointestinal stromal tumors. -
Citations
Citations to this article as recorded by- Comparison of tissue microarray and full section in immunohistochemistry of gastrointestinal stromal tumors
Mi Jung Kwon, Eun Sook Nam, Seong Jin Cho, Hye Rim Park, Hyung Sik Shin, Jun Ho Park, Chan Heun Park, Won Jae Lee
Pathology International.2009; 59(12): 851. CrossRef
- Comparison of tissue microarray and full section in immunohistochemistry of gastrointestinal stromal tumors
- Endoscopic Ultrasound-Guided Fine Needle Aspiration Cytology in the Diagnosis of a Gastrointestinal Stromal Tumor of the Stomach: A Case Report.
- Lucia Kim, Hyung Gil Kim, Young Chae Chu, In Suh Park, Suk Jin Choi, Jee Young Han, Sun Hee Kim, Don Haeng Lee, Joon Mee Kim
- J Pathol Transl Med. 2008;19(2):178-182.
- DOI: https://doi.org/10.3338/kjc.2008.19.2.178
- 2,718 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - We report here a case of a gastrointestinal stromal tumor (GIST) in the stomach that was diagnosed by endoscopic ultrasound-guided fine needle aspiration cytology (EUS-FNA). A 67 year old male patient underwent regular check-ups for five years due to the presence of a submucosal tumor that was found in the fundus of the stomach incidentally. EUS-FNA was performed to evaluate the tumor, which had increased in size from 1cm to 2.8cm. A cytologic smear revealed cohesive sheets or clusters of spindle cells with elongated nuclei. Immunohistochemical staining revealed a strong positive reaction for c-kit and CD34, without any reaction for smooth muscle actin and Ki-67. Therefore, a diagnosis of GIST was made.
- A Case of Intestinal Anthrax with Recovery after Surgical Intervention .
- Jong Im Lee, Jung Ran Kim, Dong Hoon Kim, Byoung Ook Jeoung
- Korean J Pathol. 1995;29(2):268-271.
- 1,931 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Anthrax in man is usually cutaneous, resulting from contact with materials derived from infected livestock. Internal organs are infrequently involved,. This report concerns a case of primary anthrax of intestine. The first case of primary anthrax of intestine is to our knowledge in Korea. The patient was a 14-year-old male who has complained of nausea, vomiting and acute abdominal pain. History was otherwise noncontributory except for ingestion raw meat of the dead cattle, one day before the onset of the disease. The cattle presumably died due to Bacillus anthracis in a village Bae-Ban Dong in the city of Kyung ju, Kyung Pook. Among 15 sufferers, 2 cases died 3 days later. Bacillus anthracis isolated from the raw beef, blood samples of two patients and throat culture of one patient. At laparotomy, the peritoneal cavity was full of serosanginous fluid. Right hemicolectomy including partial resection of ileum was done. The bowel was segmentally dilated, hemorrhagic and necrotic, especially at terminal ileum. The mucosa was edematous and largely ulcerated covered with greenish yellow exudate. The intense vascular congestion with hemorrhage and numerous colonization of bacteria were present through the entire wall. The organisms were large, gram-positive and PAS-negative bacilli in long chain. Bacterial emboli were scattered in lymphatics. The other feature was band like lymphoid cell infiltration in ulcer base and submucosal layer. Payer's patches were prominent and the germinal centers were necrotic. Interfollicular spaces exhibited aggregates of numerous atypical lymphoid cells. The cells were five times larger than resting lymphocytes and had several prominent nucleoli and abundant amphophilic cytoplasm. On immunohistochemical staining, most of atypical cells were positive for T-cell marker and Ki-I Ag. The mesenteric lymph nodes were enlarged, showing reactive feature, and the atypical cells were also demonstrated. The patient recovered completely.
- An Image Analytical Study on the Structural Spectrum of Intestinal Metaplasia-Dysplasia-Carcinoma of the Stomach.
- Sang Woo Juhng, Dong Ha Park, Ji Shin Lee, Kyu Hyuk Cho
- Korean J Pathol. 1993;27(1):50-57.
- 2,147 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - Intestinal metaplasia and dysplasia of the stomach have been stressed as precursors of gastric carcinoma of the intestinal type, although their preneoplastic nature is still debated. In this study, the cytomorphometric and cytokinetic spectra of the suggested preneoplastic and neoplastic lesions of the stomach were investigated. From the resected stomachs of early gastric carcinoma of intestinal type, areas of normal, intestinal metaplasia, dysplasia, and carcinoma were selected. They were immunostained for proliferating cell nuclear antigen, counterstained with propidium iodide, and various nuclear parameters were measured by image analysis. Normal and intestinal metaplastic mucosae differed by the localization of proliferation zone, but not by nuclear profile area, circular shape factor, and proliferation index. In dysplasia, proliferation zone covered large parts of the dysplastic area. Nuclear profile area and proliferation index were larger whereas circular shape factor was smaller than in normal or intestinal metaplasia. Carcinomatous lesion had diffuse proliferation activity, the largest nuclear profile area and proliferating index, and circular shape factor in-between those of normal or intestinal metaplasia and dysplasia. The above results showed a structural spectrum among normal of intestinal metaplasia, dysplasia, and carcinoma of intestinal type in cytomorphometric and cytokinetic terms. The structural spectrum raises the possibility that dysplasia of the stomach is a preneoplastic lesion.
- Chronic Intestinal Pseudoobstruction Associated with Inflammatory Visceral Neuropathy: A Case Report.
- Young Kyung Bae, Joon Hyuk Choi, Mi Jin Kim, Dong Sug Kim, Won Kyu Park, Jae Hwang Kim
- Korean J Pathol. 2004;38(3):191-195.
- 2,068 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - The pathogenesis of chronic intestinal pseudoobstruction (CIP) presents a broad spectrum of etiologies. Among them, visceral neuropathy and myopathy are two major pathologic conditions. We report here on a very rare case of CIP associated with inflammatory visceral neuropathy involving the terminal ileum, appendix and entire colon in a 64-year-old woman who did not have any detectable neoplasm or family history of this disease. Microscopically, the submucosal and myenteric plexuses showed a severe and diffuse lymphoplasmacytic infiltrate with degenerative changes of the ganglion cells and nerve fibers. The pathogenesis of the inflammatory reaction is unclear for our patient, but we think that this would be a rare example of idiopathic and sporadic visceral neuropathy resulting in chronic intestinal pseudoobstruction.
- Malignant Gastrointestinal Stromal Tumor of the Esophagus: A Case Report.
- Hae Joung Sul, Kyeong Hee Kim, Dae Young Kang
- Korean J Pathol. 2001;35(3):252-255.
- 2,117 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Gastrointestinal stromal tumors (GISTs) predominate in the stomach and small intestine but have rarely been documented in the esophagus. We report a rare case of GIST of the esophagus in a 47-year-old woman. Histologically, the tumors showed a combination of solid, myxoid, and perivascular collar-like patterns, with spindle and epithelioid cells. The tumor cells were positive for CD117, CD34, and S-100 protein and negative for desmin and -smooth muscle actin.
- Morphological Observation on the Prenatal Development of the Human Gastrointestinal Tract.
- Yeon Lim Suh, Je G Chi
- Korean J Pathol. 1990;24(2):103-119.
- 2,588 View
- 31 Download
-
 Abstract
Abstract
 PDF
PDF - A total of 322 fetuses and 29 embryos were examined light microscopically to evaluate the morphological development of the human gastrointestinal tract with increasing gestational age. The human embryos were analysed by reconstruction of serial section slides. One hundred and forty fetuses ranging from 15 to 41 weeks of gestation were used for correlating the gestational age and the body weight with the measurement of the small and large intestines. 1) The esophagus develps from the distal part of the foregut through a partition of the tracheoesophageal septum. Initially the esophagus is short, but it elongates rapidly and reaches its final relative length and position by the seventh week. The epithelium of the esophagus proliferates and completely obliterates the lumen by the seventh week, but recanalization occurs by the ninth week. The esophageal epithelia consist of three different groups of cells; stratified squamoid cells, ciliated columnar cells and tall columnar cells by the 21th week. 2) The stomach appears as a fusiform enlargement of the caudal part of the esophagus at the fourth week. During next two weeks the stomach acquires its adult shape and final position. The primordial gastric pits and the parietal cells appear at the eighth and eleventh weeks, respectively. 3) As the midgut elongates, it forms a ventral U-shaped loop, called primitive intestinal loop by the fifth week. At this stage the cecum appears as a swelling from the caudal limb of the intestinal loop. By the seventh week the bulks of the caudal limb of the intestine herniate into the umbilical cord, in which the loop rotates 90 degrees counterclockwise around the axis of the superior mesenteric artery. During the tenth week, the intestine returns to the abdomen and undergoes a further 180 degrees counterclockwise rotatation. 4) The cloaca is divided into two parts by a urorectal septum at the fifth week. By the seventh week the urorectal septum has fused with the cloacal membrane, dividing it into a dorsal anal membrane and ventral urogenital membrane. The anal membrane ruptures at the eighth week. 5) During the sixth week the duodenal lumen becomes completely filled with proliferating epithelium. The villi project from the mucosa of the small and large intestines at the eighth and eleventh weeks, respectively. The villi of large intestine become resorbed again after the 21th week. At the fifth week Paneth cells appear through the entire length of the intestine including the rectum, but disappear in the colon and the rectum after the 36th week. 6) The developing Auerbach's plexuses are well recognized along the outside of muscle coat throughout the gastrointestinal tract, but demonstrate no immunoreactivity for the anti-neuron specific enolase antibody. The neuroblasts in the myenteric plexus reveal strong positivity for the anti-neuron specific enolase antibody at the eleventh week, but the ganglion cells differentiate by the fourteenth week. 7) Differentiation of the gastrointestinal wall and development of the myenteric plexus begin form the esophagus and progress caudally down to the colon. But the anorectal wall is differentiated from the cloaca more earlier than the esophagus, stomach and colon are. 8) The small and the large intestines elongate progressively with the increasing gestational age and body weight and increase approximately 5.6 and 5.4 folds, respectively during the 25 weeks from the 15th to 41th week of gestation. At the 40th gestational week the small intestine is 5.68 times the length of the colon. 9) The correlation between the body weight (BW), crown-rump length (CR) and intestianl length (small intestine (SI), large itestine (LI) is presented as: SI (cm)= -33.67 + 4.14CR + 11.62 (BW)(1/3), LI (cm)= 5.56 + 0.76CR + 0.007BW (gm), CR (cm)= 7.82 + 0.015 SI + 0.41 (BW)(1/2).
- Primary Extragastrointestinal Stromal Tumor (EGIST) of the Greater Omentum.
- Kyung Un Choi, Jee Yeun Kim, Do Youn Park, Chang Hun Lee, Mee Young Sol, Kang Suek Suh, Jun Woo Lee
- Korean J Pathol. 2001;35(4):347-350.
- 3,953 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - Gastrointestinal stromal tumors (GISTs) were recently defined as spindle cell, epithelioid, or occasionally, pleomorphic mesenchymal tumors of the gastrointestinal tract that express the CD117 (proto-oncogene c-kit protein, stem cell factor receptor), as detected using immunohistochemistry. And they show a new tendency to include the CD117-positive mesenchymal spindle cell or epithelioid neoplasms primary in the omentum and mesentery, and is so termed extragastrointestinal stromal tumors (EGISTs). Omental EGISTs are very rare and similar to their gastrointestinal counterpart. We present a case of primary EGIST of the greater omentum in a 58-year-old man. The resected tumor mass measured 20X15X5 cm and weighed 1,150 g. The cut surface displayed a central cystic change and partial mural nodules. Microscopically, most parts of the tumor were composed of round or polygonal cells, with many of them containing perinuclear vacuoles. The mitotic count was less than one per 50 high-power-fields. Immunohistochemically, the tumor cells were diffusely positive for CD117 and vimentin, and focally for smooth muscle actin and CD34. Ultrastructurally, partially smooth muscle differentiation was confirmed in this case.
- Flow Cytometric DNA Analysis of Gastrointestinal Stromal Tumors .
- Mee Yon Cho, Soon Won Hong, Soon Hee Jung, Hogeun Kim, Chanil Park
- Korean J Pathol. 1997;31(7):608-616.
- 2,108 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - To evaluate the correlation between the histologic grade and DNA ploidy or proliferation index/S phase fraction (SPF) of gastrointestinal stromal tumors, we performed the DNA analysis using the flow cytometry. Paraffin embedded tissue samples of 57 gastrointestinal stromal tumors were used. The sites of the tumors were: stomach (28), small intestine (23), and large intestine(6). DNA index, proliferative index, and SPF by the flow cytomery were compared with histologic grade. The histologic grade of the gastric tumors were benign (12), borderline (10), and malignant (6). Those of the small intestinal timors were benign (2), borderline (13), and malignant(8). The large intestine were borderline (2), and malignant (4). In stomach, aneuploidy was found in 25.0% of benign, 40.0% of borderline, and 100% of malignant. And there was statistically significant correlation between the histologic grade and ploidy (p < 0.05). By contrast, small and large intestinal tumors showed more frequent aneuploidy in benign than in malignant. The proliferative index was correlated with the histologic grade in gastric tumors (p<0.05), but the SPF was not. In conclusion, the ploidy and proliferative index of gastric tumors are closely correlated to the histologic grade. However, aneuploidy in tumors of the small and large intestine were difficult to predict the malignancy.
- Porposal for Creating a Guideline for Cancer Registration of the Gastrointestinal Tumors (I).
- Mee Yon Cho, Yun Kyung Kang, Kyoung Mee Kim, Hee Kyung Chang, Hee Jin Chang, Mee Soo Chang, Joon Mee Kim, Dae Young Kang, Chanil Park, Jin Hee Sohn
- Korean J Pathol. 2008;42(3):140-150.
- 2,636 View
- 47 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cancer registries are fundamental for cancer control and multicenter collaborative research. However, there have been discrepancies among pathologists in classifying cancer and assigning the codes according to the International Classification of Disease Oncology 3 (ICD-O3). To improve the quality of cancer registries as well as to prevent the conflict with medical insurance compensation, a guideline for the coding of cancer is mandatory.
METHODS
AND RESULTS: Funded by the Management Center for Health Promotion, 40 members of the Gastrointestinal Pathology Study Group and the Cancer Registration Committee of the Korean Society of Pathologists participated in the 1st workshop for gastrointestinal tumor registration. The subjects of gastric epithelial tumor, intramucosal carcinoma of the colon, carcinoid tumor, gastrointestinal stromal tumor and appendiceal mucinous tumor were discussed to create a guideline. A survey to obtain consensus for the guideline proposed by the workshop was carried out by the members of the Korean Society of Pathologists and 240 members completed the questionnaire.
CONCLUSION
Although there are some issues to be discussed further, such as coding of high grade dysplasia/adenoma and intramucosal carcinoma of stomach and colon, the members agreed upon most parts of the proposed guideline. Therefore, we suggest using the ICD-O3 coding guideline for gastrointestinal tumor.
- Immunohistochemical Expression of CD117, CD34, Vimentin and alpha-Smooth Muscle Actin in Gastrointestinal Stromal Tumors.
- Jong Kuk Kim, O Jun Kwon, Byung Heon Kim
- Korean J Pathol. 2001;35(6):506-512.
- 4,740 View
- 10 Download
-
 Abstract
Abstract
- BACKGROUND
The interstitial cell of Cajal (ICC), the cell of origin for gastrointestinal stromal tumor (GIST), expresses CD117 (c-kit) which is a receptor for KIT ligand in cell membranes. It is immunohistochemically positive for CD117, CD34 and vimentin, but not for alpha-smooth muscle actin (SMA).
METHODS
We performed the immunohistochmical study with anti-CD117, anti-CD34, anti-VMT and anti-alpha-SMA in paraffin-embedded tissue of 28 GISTs and 19 smooth muscle tumors arising in the gastrointestinal tract, mesentery, omentum and retroperitoneum (GISMT) to determine the precise nature of GIST cells.
RESULTS
The positive rates of CD117, CD34 and vimentin in extraGISTs were significantly higher than in GISMTs. The positive rate of alpha-SMA in GIST was not significantly different than in GISMTs.
CONCLUSIONS
A subset of GISTs may express alpha-SMA as well as CD117 and the cell of their origin may be a ICC precursor cell which is capable of differentiating bidirectionally into ICC and smooth muscle cell. This explains why GISTs may arise out of gut where ICC is not present and that they may represent the tumors arising from ICC precursor cell present around the gastrointestinal tract.
- Ovarian Sertoli-Leydig Cell Tumors with Heterologous Gastrointestinal Type Epithelium or with Striated Skeletal Muscle: report of two cases.
- Ki Ouk Min, Eun Joo Seo, Young Shin Kim, Kyo Young Lee, Sang In Shim
- Korean J Pathol. 1996;30(1):50-56.
- 2,183 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF - Sertoli-Leydig cell tumors of the ovary are rare, accounting for no more than 0.5% of all ovarian neoplasms. These tumors occur predominantly in women 10 to 30 years of age. Heterologous elements are found in over 20% of the moderately and poorly differentiated Sertoli- Leydig cell tumors. The most common element is gastrointestinal mucin-secreting epithelium, found in approximately 20% of all cases. Approximately 4% of Sertoli-Leydig cell tumors contain immature skeletal muscle and/or cartilaginous elements. The origin of these neoplasms is regarded as neometaplasia of the mesodermal neoplastic element. While the degree of differentiation of Sertoli-Leydig cell tumors is probably of greater importance in determining prognosis than the presence of heterologous components, recent evidence does point to an unfavorable effect on clinical outcome when heterologous mesenchymal components such as cartilage and striated muscle are present. We experienced two cases of ovarian heterologous Sertoli-Leydig cell tumors with gastrointestinal type epithelium and striated skeletal muscle in 20 and 21 year-old females, respectively. One case involved a patient who had complained of amenorrhea for 3 years while the other case involved a patient who had complained of left lower abdominal tenderness and amenorrhea for one and one half years. It was determined by ultrasonography of the pelvis that the two patients suffered from right and left ovarian masses. Both patients underwent adnexectomy. These tumors were large with partly solid and partly cystic areas. Based on light microscopic examination one case was classified as an intermediate Sertoli-Leydig cell tumor with heterologous gastrointestinal type epithelium, while the other case was classified as a poorly differentiated Sertoli-Leydig cell tumor with heterologous striated skeletal muscle.
- Synchronous Development of Gastrointestinal Stromal Tumor and Arteriovenous Malformation in the Jejunum: A Case Report.
- Sang Hwa Shim, Yoon Hee Han, Ji Eun Kwak, Sun Hee Chang, Hanseong Kim, Je G Chi, Mee Joo
- Korean J Pathol. 2008;42(3):185-188.
- 2,429 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - Vascular malformations associated with neoplasms are extremely rare. Herein we report an extraordinary coincidence of arteriovenous malformation (AVM) and gastrointestinal stromal tumor (GIST) in the jejunum. A 44-year-old woman presented with melena and anemia. Abdominal computed tomography revealed a highly vascularized, strong early arterial enhancing soft tissue mass in the jejunum, which was confirmed by angiography to be an AVM supplied by the distal jejunal branch of the superior mesenteric artery. An emergency operation was performed due to active gastrointestinal (GI) bleeding. The resected jejunum showed a protruding, mostly solid subserosal mass. The mass was confirmed to be a spindle cell type GIST and was intermingled with the AVM located in the overlying submucosa and muscularis propria. To our knowledge, this is the first reported case of an AVM associated with a GIST. This case masqueraded radiologically as an AVM alone and presented clinically with GI bleeding.
- CD34 Antigen Expression in Gastrointestinal Stromal Tumors.
- Sun Hee Sung, Min Sun Cho, Woon Sup Han
- Korean J Pathol. 1997;31(11):1166-1171.
- 4,278 View
- 13 Download
-
 Abstract
Abstract
- Gastrointestinal stromal tumor (GIST) is known as considerable controversal tumor about it's histogenesis, differentiation and biologic behavior. It is traditionally regarded as smooth muscle tumor. To evaluate and clarify the origin of tumor, we performed immunohistochemical study of 23 cases of GIST on CD34 antigen, alpha-smooth muscle actin, S-100 protein, and compared the result with 4 cases of typical leiomyoma of GI tract. The results were as follows. CD34 antigen expression was noted in 21 cases (91.3%) of GIST, while typical leiomyoma was all negative. There were no difference of CD34 expression according to the biologic behavior. However, it's staining pattern was significantly different (p<0.05). Focal or multifocal expression was dominant in benign GIST (58.3%), while diffuse expression was dominant in malignant GIST (80%). Actin was expressed in 5 cases of benign GIST (38.5%) and 1 of malignant GIST (16.7%) focally. All typical leiomyoma showed diffuse strong positivity on alpha-smooth muscle actin. S-100 protein was expressed in 2 cases of benign GIST (16.7%) only. The pattern of CD34 expression was focal in the actin or S-100 protein positive cases. In conclusion CD34 antigen is useful marker in the separation of GIST, from typical smooth muscle tumor. Also it suggest that most GISTs are histogenetically primitive mesenchymal cell origin. However, CD34 expression was unrelated with biologic behavior of GIST.
- Helicobacter pylori Infection and Histopathological Features of Gastric Mucosa.
- Gyung Hyuck Ko, Cheol Keun Park, Chun Sik Choi, Heung Bae Park, Jeong Hee Lee, Hye Jung Lee, Hyun Ju Kim, Kwang Ho Rhee
- Korean J Pathol. 1996;30(3):199-209.
- 2,142 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - A microscopic examination of 1,000 cases of gastroscopic biopsy specimens revealed that the prevalence and severity of chronic gastritis, neutrophilic infiltration, and Helicobacter pylori infection increased with advancing age until the age reached about 40, but they decreased thereafter in accordance with the increasing prevalence of intestinal metaplasia. The prevalence and severity of Helicobacter pylori infection, chronic gastritis, and neutrophilic infiltration were proportionately related to each other and to gastric peptic ulcer, but inversely related with intestinal metaplasia and gastric carcinoma. The results suggested that chronic gastritis and gastric peptic ulcer may be associated with Helicobacter pylori infection and that if these lesions persist, intestinal metaplasia may develop with decreased severity of chronic gastritis and Helicobacter pylori infection but, instead, increase of the risk of gastric carcinoma. And it is thought that the cause of the high incidence of gastric carcinoma in Korea may be related to the fact that chronic gastritis and Helicobacter pylori infection develop earlier in life and therefore the prevalence of intestinal metaplasia is higher in Korea than in other countries.
- Enteric Cyst in the Tongue.
- Jeong Yun Shim, Ho Guen Kim
- Korean J Pathol. 1997;31(11):1237-1239.
- 1,891 View
- 10 Download
-
 Abstract
Abstract
- A case of enteric cyst in the anterior two-thirds of the tongue is reported. The patient, a 42 day-old female infant, presented with a protruding tongue mass since birth. Under the impression of ectopic thyroid gland or leiomyoma, complete resection was performed. The mass proved to be an enteric cyst, lined by small intestinal mucosa with an underlying coat of smooth muscle. Enteric cysts arising in the tongue is rare and only 8 such cases have been reported in the literature.
- Pneumatosis Cystoides Intestinalis of Adult Ileum: A Case Report.
- Seoung Wan Chae, Hye Kyung Ahn, Jin Hee Sohn
- Korean J Pathol. 2002;36(2):119-121.
- 2,105 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Pneumatosis cystoides intestinalis is an uncommon condition characterized by the presence of multiple gas-filled cysts within the gastrointestinal wall. This lesion occurs in association with a large variety of gastrointestinal and non-gastrointestinal conditions. Herein, we describe a case of pneumatosis cystoides intestinalis of the small intestine that developed in a 31-year-old man with a history of duodenal ulcer and pyloric stenosis. Emergency exploro-laparotomy was done due to a suspicion of ulcer perforation. Primary closure for duodenal ulcer perforation and segmental resection of ileum were done. Resected ileum showed diffuse sponge-like changes in the wall. Microscopically, variable-sized cystic lesions, lined by flat or multinucleated giant cells, were noted throughout the intestinal wall.
- Gastrointestinal Cytomegalovirus Infection: A clinicopathologic analysis of 8 cases.
- Yun Kyung Kang, Sang Yong Song, Woo Ho Kim, Yong Il Kim
- Korean J Pathol. 1994;28(1):22-29.
- 1,923 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - We analysed 8 cases of gastrointestinal cytomegalovirus(CMV) infection including one autopsy, three surgically resected and four endoscopic biopsy cases. Involved sites were colon in four,stomach in three and small intestine in one. Three of them were associated with immu-nosuppressed condition but others had no clinical evidence of immune deficiency. Multiple aphthous mucosal ulceration was a common presentation, but one revealed a mucosal ulcer with segmental narrowing and thickening of wall. Microscopically, six showed cytomegalic inclusions in endothelial cells and fibroblasts, one in mucosal epithelial cells and the remaining one in both endothelial cells and mucosal epithelial cells. Immunohistochemical staining using monoclonal antibody against CMV confirmed postive result in seven cases. Serum IgM anti-CMV antibody was elevated in one case. We conclude that gastrointestinal CMV infection is currently not a rare condition and frequently associated with non-immunosuppressed condition, and thus a thorough histologic examination is required especially in the gastrointestinal ulcerative lesion. Once cytomegalic inclusion is suspected, immunohistochemical identification of CMV seems essential for specific diagnosis.
- Correlation of the Intestinal Metaplasia Subtypes and Gastric Carcinoma.
- Hwa Eun Oh, Mee Ja Park, Jong Sang Choi
- Korean J Pathol. 1997;31(12):1272-1281.
- 2,193 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Helicobacter pylori, loss of basement membrane, atrophy, type III intestinal metaplasia, adenomatous polyposis coli (APC) gene mutations and altered p53 function were believed as a factor to develop the gastric adenocarcinomas. To investigate the incidence and prevalence of Helicobacter pylori, intestinal metaplasia and atrophy, 120 gastrectomy specimens collected from patients with gastric adenocarcinoma (100 cases) and non-neoplastic conditions (20 cases) were studied. Intestinal metaplasia can be classified as type I (complete), type II (incomplete, sulfomucin-negative) and type III (incomplete, sulfomucin-positive) by Filipe and Jass. The incidence of intestinal metaplasia of gastric adenocarcinoma was 96% compared with the incidence of 75% in non-neoplastic conditions. The type I and type II were more common than type III and were present in both non-neoplastic conditions (75%) and adenocarcinoma (74%). In contrast, type III intestinal metaplasia was seen in only 20% of intestinal metaplasia-positive cases, all of which (22 of 22) were from patients with adenocarcinoma. The high specificity of type III intestinal metaplasia might be acceptable for screening purposes, but its sensitivity of 22% for gastric adenocarcinoma is low. Helicobacter pylori were detected in 96% of adenocarcinoma cases and 100% of non-neoplastic cases. Atrophy was detected in 50% of non-neoplastic cases and in 57% of adenocarcinoma cases. The data thus confirms a significant relation between incomplete sulfomucin-secreting intestinal metaplasia (type III) and gastric carcinoma, especially intestinal type (p<0.01). Thus, the type III intestinal metaplasia should be considered a risk factor and its presence in a biopsy specimen should prompt close surveillance.
- Prognosis of Gastrointestinal Stromal Tumors Arising in the Stomach and Small Intestine: A Retrospective Study of 126 Cases from a Single Institution.
- Sang Hee Seok, Jun Mo Kim, Jung Min Bae, Se Won Kim, Sang Woon Kim, Sun Kyo Song, Young Kyung Bae
- Korean J Pathol. 2008;42(6):335-343.
- 2,549 View
- 43 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor in the gastrointestinal tract. As all GISTs have the potential for aggressive clinical behavior, the guidelines for defining the risk of aggressive behavior have been developed and they have been recently revised to precisely assess these patients' prognosis.
METHODS
We analyzed 94 gastric and 32 small intestinal GISTs to compare the patients' survival with the risk stratification (original and revised). RESULTS: For gastric GISTs, 10 mitoses/50HPF was an important cutoff value for the risk of metastasis (1.3% vs 29.4%, respectively), whereas 16.7% of all the small intestinal GISTs with less than 5 mitoses/50HPF metastasized. The small intestinal GISTs showed higher frequencies of mucosal invasion and coagulation necrosis than did the gastric ones. Gastric GISTs had a significantly lower incidence of metastasis/recurrence than did the small intestinal ones in the same risk group. On multivariate analysis, the anatomic location (small intestine), the tumor size (>10 cm) and the mitotic count (>10/50HPF) were independent prognostic factors for a shorter disease-free survival for patients with GISTs. The mitotic count was more important than tumor size for both gastric and small intestinal GISTs.
CONCLUSION
Small intestinal GIST is a more aggressive tumor than gastric GIST and the mitotic count is the most important prognostic factor for GISTs.
- A Case of Heterophyid Trematode Infection with Intestinal Obstruction.
- Jin Young Yoo, Sang In Shim
- Korean J Pathol. 1994;28(1):65-67.
- 2,152 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - This report describes a case of ileal obstruction in a 31-year-old male with acute abdominal pain. A plain film of the abdomen showed segmental obstruction of small intestine. The patient underwent laparoscopic resection of the segment. Microscopic examination demonstrated foci of ulceration, submucosal edema, transmural inflammation, mural and neural hyperplasia and noncaseating granulomas, mimicking Crohn's disease. However, there were microabscesses predominantly composed of eosinophils. Furthermore, a section of an adult heterophyid trematode was identified in the crypt. Heterophydiasis usually causes diffuse enteritis. Therefore, this case with intestinal obstruction seems to be a rare manifestation of intestinal heterophydiasis.
- Angiodysplasia Arising in the Bowels: Two cases report.
- Soo Kee Min, Hee Jeung Cha, Joon Mee Kim, Young Chae Chu
- Korean J Pathol. 1997;31(12):1308-1313.
- 2,114 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Gastrointestinal angiodysplasia is a distinct disease entity which causes frequent gastrointestinal bleeding. It predominantly arises at the stomach and duodenum in the upper gastrointestinal tract and cecum and ascending colon in the lower gastrointestinal tract. The general histological finding of the angiodysplasia is a submucosal vascular ectasia and tortuosity. We have experienced two cases of the intestinal angiodysplasia. The first case occurred on a jejunum in a 22-year-old woman who had anemia. The second case occurred on a sigmoid colon in a 59-year-old man who had constipation. In addition to the general histologic finding of the angiodysplasia, the microscopic findings of the first case revealed some capillary hemangioma-like areas; and in the second case, there was a marked ischemic change and the thickening of the wall.
- Histopathologic Study of Primary Gastrointestinal Lymphoma: Gross and immunohistochemical analysis of 30 cases.
- Hye Jae Cho, Jeong Eun Joo, Ill Hyang Ko
- Korean J Pathol. 1994;28(2):118-125.
- 1,968 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - A histopathologic study including iramunohistochemical stains was made in 30 patients who were presented with gastrointestinal lymphoma. The occurrence was 13 in the stomach, 8 in the ileocecum, 7 in the small intestine and 2 in the colon. The disease more frequently affected males than females and the average ages were 53 years in the patients of gastric lymphoma and 44 years in the patients of intestinal lymphoma. Gastric lymphomas were usually presented with a single lesion, and the antrum and/or body were the most common sites. But intestinal lymphomas were presented with a single or multiple lesion, and the ileocecum was the most common site. The most common gross type of gastrointestinal lymphomas was the ulceroinfiltrating type and most are of the diffuse large noncleaved cell type of B-cell lymphoma, histologically. There were 2 cases of T-cell lymphoma presented in the intestine as the superficially ulcerative gross pattern and diffuse immunoblastic cell type. The distinct MALToma was seen in only one case of stomach but the feature was partially remained in each two cases of stomach and intestine. Their coexistent findings may suggest that diffuse large of immunoblastic component arises through blastic transformation of the low-grade M ALToma component.
- The Loss of Expression of Caveolin-1 in Gastrointestinal Stromal Tumors.
- Eo Jin Kim, Jin Hee Sohn, Min Kyung Kim, Seoung Wan Chae, Hye Seung Lee, Eun Yoon Cho, Woo Ho Kim
- Korean J Pathol. 2005;39(5):338-344.
- 2,403 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The down-regulation of caveolin-1, a putative tumor suppressor gene, has been demonstrated in several types of sarcomas. However, it's not known whether or not the gastrointestinal stromal tumors (GISTs) express caveolin-1. We carried out this study to investigate the caveolin-1 expression in GISTs and to determine the correlation between the clinicopathologic profiles of GISTs and the expression of caveolin-1.
METHODS
One hundred eight cases of formalin-fixed and paraffin-embedded tissues of GISTs were immunohistochemically evaluated for the expression of caveolin-1 by using the tissue-array method. Survival data of 98 cases of primary GISTs was analysed according to the expression status of caveolin-1.
RESULTS
Ninety three cases (86.1%) of 108 GISTs did not express caveolin-1 protein. There was no correlation between the caveolin-1 expression status and any of the clinicopathologic variables, including mitosis (p=0.948) and tumor grade (p=0.334). The expression of caveolin-1 was not correlated with other immunohistochemical marker proteins including, c-kit (p=0.373), CD34 (p=0.437) and SMA (p=0.831). On the univariate analysis, the caveolin-1 expression status (p=0.635) was not a significant predictor of the disease-free survival for GIST patients.
CONCLUSIONS
The results of this study suggest that caveolin-1 might act as a tumor suppressor gene in the GIST oncogenesis, but it has no function as a prognostic marker for disease free survival.
- Carcinoid Tumors of the Gastrointestinal Tract: Analysis of 36 Cases.
- Kyeong Cheon Jung, Hee Sung Kim, Sang Yong Song, Ghee Young Choe, Yong Il Kim
- Korean J Pathol. 1996;30(5):396-407.
- 2,025 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - We reviewed a total of 36 cases of gastrointestinal carcinoid tumors during a period of ten and a half years at Seoul National University Hospital, looking at their histologic and ultrastructural features, as well as immunohistochemical results, then we correlated these with location. The primary sites of carcinoid tumors were rectum(39%), stomach(25%), appendix(22%), small intestine(8%) and colon(6%), in order of frequency. The predominant histologic types by organ were mixed and solid(A) types in all location, the solid type(type A) in the stomach, and tubular type(type C) in the rectum. Six out of 8 cases of appendiceal carcinoid were type A and the other two cases were mucinous carcinoid. Tubular adenoma or adenocarcinoma was associated with 36% of the rectal carcinoids, with one case of carcinoid in the small intestine, and one(11%) of the gastric carcinoids was found near an adenocarcinoma. Metastasis was found in one case of ileal carcinoid(100%), one case of cecal carcinoid, 3 of gastric carcinoid(33%) and 2 of rectal carcinoid(14%). Primary tumor size ranged from 1 to 7 cm. Tumor necrosis and endolymphatic tumor emboli were found in 57% and 43% of the metastatic carcinoids, respectively. PCNA index showed a borderline significant difference between metastatic and nonmetastatic groups(P value=0.063). The low prevalence of appendiceal carcinoid and the relatively high prevalence of gastric-rectal carcinoid may reflect a low chance of incidental appendectomy and frequent detection of gastrointestinal endoscopy.
- Bleeding from Dieulafoy's Vascular Malformation of the Proximal Ileum: A case report .
- Hee Jung Kim, Jun Keun Jung, Young Min Suh, Kyung Sook Kim, Hoguen Kim
- Korean J Pathol. 1999;33(12):1207-1210.
- 2,009 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Dieulafoy's vascular malformation is a rare cause of massive gastrointestinal bleeding. Most often it occurs in stomach within 6 cm from the gastroesophageal junction. Only a few cases have been reported to occur in the small intestine and colon. Occasionally, Dieulafoy's lesion of small intestine is difficult to recognize because of rarity, a paucity of symptoms and negative findings on barium studies. Therefore, this lesion needs to be considered in a patient with massive lower gastrointestinal bleeding. We report a case of Dieulafoy's vascular malformation in ileum 2 m proximal to ileocecal value in a 41-year-old woman who visited emergency clinic because of hematemesis, dizziness and vomiting. Small intestine revealed a wide-caliber artery within the submucosa showing intimal thickening, medial muscular hypertrophy and thrombosis.
- Idiopathic Entero-colic Lymphocytic Phlebitis: A case report.
- Seung Sam Paik, Young Ha Oh, Eun Kyung Hong, Jung Dal Lee
- Korean J Pathol. 1996;30(6):533-538.
- 2,350 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Localized enterocolic lymphocytic phlebitis is characterized by selective phlebitis involving the small to medium-sized veins and venules, infiltration exclusively by lymphocytes, and no other systemic vasculitis or inflammatory bowel disease. This vasculitis can be a rare cause of intestinal ischemia. We experienced a case of enterocolic lymphocytic phlebitis in a 72-year-old woman, who presented with abdominal pain and distension. The resected colon and terminal ileum showed striking lymphocytic phlebitis affecting the veins and venules of the bowel and mesentery which resulted in ischemic injury of the bowel. This vasculopathy was the only demonstrable cause of ischemia. Arteritis and arteriolitis was not found. There is no clinical or laboratory evidence or a history of extraintestinal vasculitis. The etiology of this clinicopathological entity has not been elucidated. Herein, we report the clinicopathological findings in this patient who presented with ischemic intestinal necrosis caused by localized intestinal lymphocytic phlebitis associated with thrombosis.
- Idiopathic Intestinal Lymphangiectasia.
- Kun Chang Song, Chan Il Park
- Korean J Pathol. 1994;28(3):319-321.
- 2,127 View
- 10 Download
-
 Abstract
Abstract
- This is a case report of idiopathic intestinal lymphangiectasia occurring in a 3-year-old boy. Idiopathic intestinal lymphangiectasia is believed to be a part of the generalized congenital disorder of lymphatic system. The present case revealed markedly ectatic lymphatics in the lamina propria of duodenal villi with lymphorrhagia. Clinical features were typical of the protein-losing enteropathy; hypoalbuminemia, hypocalcemia, chylous ascites, edema of the lower extremities and mild lymphocytopenia. This case indicates that serious protein loss may ensue, even in cases of intestinal lymphangiectasia without abnormalities of extraintestinal lymphatics.
- Histologic Variations of Intramural Heterotopic Pancreas in Gastrointestinal Tract Analysis of 15 Cases.
- Seung Sook Lee, Yong Il Kim, Woo Ho Kim, Eun Sil Yu
- Korean J Pathol. 1991;25(6):520-527.
- 2,011 View
- 13 Download
-
 Abstract
Abstract
 PDF
PDF - We reviewed a total of 15 cases of heterotopic pancreatic tissue within the gastrointestinal wall(intramural type), and compared with 3 extramural ones. Intramural heterotopic pancreatic lesions were located in the antrum(33%), pylorus(20%), and body of stomach(7%), and the remainders in the duodenum(40%). Only two cases presented with chinical symptoms by their existence. Two of them were situated within the submucosa, 3 in the muscularis, 6 in submucosa-muscularis, 2 in the muscularis-subserosa, and 1 in the susbmucosa-subserosa. Intramural type was featured with their structural heterogeneity compared to the extramural ones; 10 cases showed participation of gastrointestinal mucosal elements, and some accompanied tissue elements that were indistinguishable from submucosal epithelial heterotopia or microduplication cyst of the stomach. Langerhans islets were found in 67%, and one developed islet cell tumor. The above results suggest that the initially engrafted heterotopic pancreatic tissue becomes modified and presents with heterogeneity of endodermal and mesodermal tissue-derived components by its intramural growth during the gastrointestinal organogenesis; failure of opening of its drainage system into the gastrointestinal lumen may result in the increase of intraductal pressure with subsequent atrophy of the acinar tissue and various metaplastic changes of ductal epithelium, aside from induction of smooth muscle coat around the heterotopic tissue.
- Pathological Predictor for Prognosis in Gastrointestinal Mesenchymal Neoplasms.
- Mee Yon Cho, Ho Guen Kim, Chan Il Park, Yoo Bock Lee
- Korean J Pathol. 1991;25(6):528-538.
- 2,066 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - To evaluate the prognostic predictor and clinicopathologic characteristics of the gastrointestinal (GI) mesenchymal neoplasm, we examined 75 cases of GI mesenchymal tumors surgically resected during 8 years from 1983 to 1990. Various histological parameters referrable to the prognosis, including the Ag-NORs count, were analysed. Fifty cases were followed-up for 1 to 7 years. Sixteen out of these fifty cases died during this period. The location of tumor was the stomach in 33 cases, the small intestine in 31 cases and the large intestine in 11 cases, and the tumor size was variable from 2 to 35 cm in diameter. The GI mesenchymal neoplasm appeared as an extraluminal mass in 50 cases, an intramural mass in 17 cases, and an intraluminal mass in 8 cases. Each tumor was composed of spindle or epithelioid cells, the former cell type being more common than the latter (45 vs 30 cases). Mitotic count of the tumor showed the best correlationship with the survival of patients(p<0.05), although the tumor size and necrosis appeared to have some values. The Ag-NORs count was variable and was not significantly correlated with the patient's prognosis(p>0.05). These results indicate that the mitotic count is the most valuable pathological predictor for the prognosis in GI mesenchymal neoplasms.
- An Imported Case of Intestinal Capillariasis Presenting as Protein-Losing Enteropathy.
- Youngmee Kwon, Hwoon Yong Jung, Hyun Kwon Ha, Inchul Lee
- Korean J Pathol. 2000;34(3):235-238.
- 2,393 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF - Intestinal capillariasis is caused by a small trichurid nematode, Capillaria philippinensis, which infects freshwater fish as intermediate hosts and subsequently fish eating birds as definitive hosts. It has occurred in areas such as the Philippines and Thailand where people eat raw fish. We report an imported case of intestinal capillariasis in a 31-year-old Korean man who lived in Saipan for ten years. He suffered from diarrhea with weight loss, abdominal distension, and pitting edema in the lower extremities for two years. He ate raw freshwater fish in the Saipan 2 years ago. The diagnosis was confirmed by jejunal biopsy. Flat mucosal surface without villi contained sections of numerous round worms with stichosome, larvae, and eggs which were identified as Capillaria philippinensis. The patient was successfully treated with albendazole.
- Gastrointestinal Stromal Tumors associated with Neurofibromatosis Type I: A Report of Two Cases.
- Joo Heon Kim, Ock Seong In, Seong Kyu Lee, Haing Woon Baik, Seong Ho Kim, Dong Wook Kang, Kyung Hee Kim, Mee Ja Park, Yong Il Kim
- Korean J Pathol. 2006;40(2):137-141.
- 2,232 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - Gastrointestinal stromal tumor (GIST) is the most common non-epithelial neoplasm arising in the gastrointestinal tract, but this tumor is rarely seen in association with type 1 neurofibromatosis (NF-1). We report here on two cases of multiple GISTs of the small intestine that occurred in NF-1 patients. We also analyzed the mutations of c-kit exons 9, 11, 13 and 17 and the plateletderived growth factor receptor-alpha (PDGFRA) exons 12 and 18 in two GIST patients. Histologically, the NF-1-associated GISTs were similar to those of non-the NF-1 GISTs, but they characteristically revealed hyperplastic interstitial cells of Cajal around the GISTs. Immunohistochemically, these tumors showed strong co-expressions of CD117 and CD34. The molecular genetic analysis of the GISTs showed that all of the c-kit and PDGFRA exons that were analyzed in the GISTs of the two patients were the wild-type, suggesting a limited role for the c-kit and PDGFRA mutations in the tumorigenesis of NF-1-associated GISTs.
- Clinicopathologic Analysis of Gastrointestinal Polyps.
- Hye Rim Park, In Sun Kim, Seung Yong Paik
- Korean J Pathol. 1988;22(3):232-243.
- 1,903 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Pathologists play an important role in proper evaluation of endoscopically removed polyps of the gastrointestinal tract. This study is purposed to reclassify the polyps and review the clinicopathologic features of each histologic subtypes and their malignant potential. Our material consists of total 345 gastrointestinal polyps obtained from Jan. 1986 to Dec. 1987. The results are as follows: 1) A total of 345 gastrointestinal polyps was removed from stomach is 151 cases, from colon in 180 cases, and from small intestine in 14 cases. 2) Hyperplastic polyps were the most common type of polyps I stomach (53.6%) whereas neoplastic polyps were the most common in colon (56.1%). 3) Hyperplastic polyps of the stomach occur in any age after the 3rd decade of life and neoplastic polyps predominantly developed between the 5th and 8th decades. Juvenile retention polyps were frequently noted before the 3rd decade of age. 4) Approximately 267 cases (77.4%) of patients had a single polyp and the remainders had multiple polyps. The gastric polyps were usually located at the antrum and the colonic polyps were at the sigmoid colon and rectum. 5) Epithelial atypia was exclusively noted in the neoplastic polyps of stomach (72.7%) and colon (72.3%). Malignancy in the polyp was observed in the neoplastic polyps only (13 cases). 6) Different types of polyp may occur in the same organ.
- Classification of Gastrointestinal B-cell Lymphoma and Expression of Cyclin D1, bcl-2, bcl-6, p53 Protein and PCNA.
- Ji Han Jung, An Hee Lee, Chang Suk Kang, Byung Kee Kim
- Korean J Pathol. 2000;34(6):437-445.
- 2,100 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Until recently, the gastrointestinal lymphomas were classified according to the criteria developed for the node-based lymphomas. In recent years, the REAL classification provided a new category of MALT lymphoma and Mantle cell lymphoma in B-cell lymphomas. Low-grade MALT lymphomas have been well characterized clinically, histologically, and immunophenotypically. We retrospectively recategorized 41 cases of the primary gastrointestinal B-cell lymphoma and investigated the expression of cyclin D1, bcl-2, bcl-6, p53 protein, and PCNA by immunohistochemical method. The cases were categorized in 5 groups, low grade MALToma, low/high grade MALToma, high grade MALToma, diffuse large cell lymphoma, and mantle cell lymphoma according to the morphological findings. The expression of cyclin D1 protein was restricted to the cases of mantle cell lymphoma. The bcl-2 protein expression was higher in the low grade MALT lymphoma than in the high grade lymphoma (P=0.006). The bcl-2 protein expression was higher in the low grade area than in the high grade area in the low/high grade MALT lymphoma (P=0.005). The bcl-6 and p53 protein expression was higher in the high grade MALT lymphoma than in the low grade lymphoma (P=0.022, P<0.018). However, the bcl-6 protein expression of the tumor cells was higher in high grade area than in low grade area in the low/high grade MALT lymphoma (P=0.004). The degree of the PCNA expression was positively correlated with the grade of the malignant lymphoma (P=0.003). The above results suggest that the cellular proliferation assessed by PCNA index correlates with the histologic grade. And the bcl-2, bcl-6, p53 protein may be effective in the transition from the low grade MALT lymphoma to the high grade lymphoma. Therefore, we can differentiate the low grade lymphoma from the high grade lymphoma by the immunohistochemical staining for cyclin D1, bcl-2, bcl-6, p53 protein and can predict the prognosis of the patients in accordance with the grade of the tumor.

 E-submission
E-submission
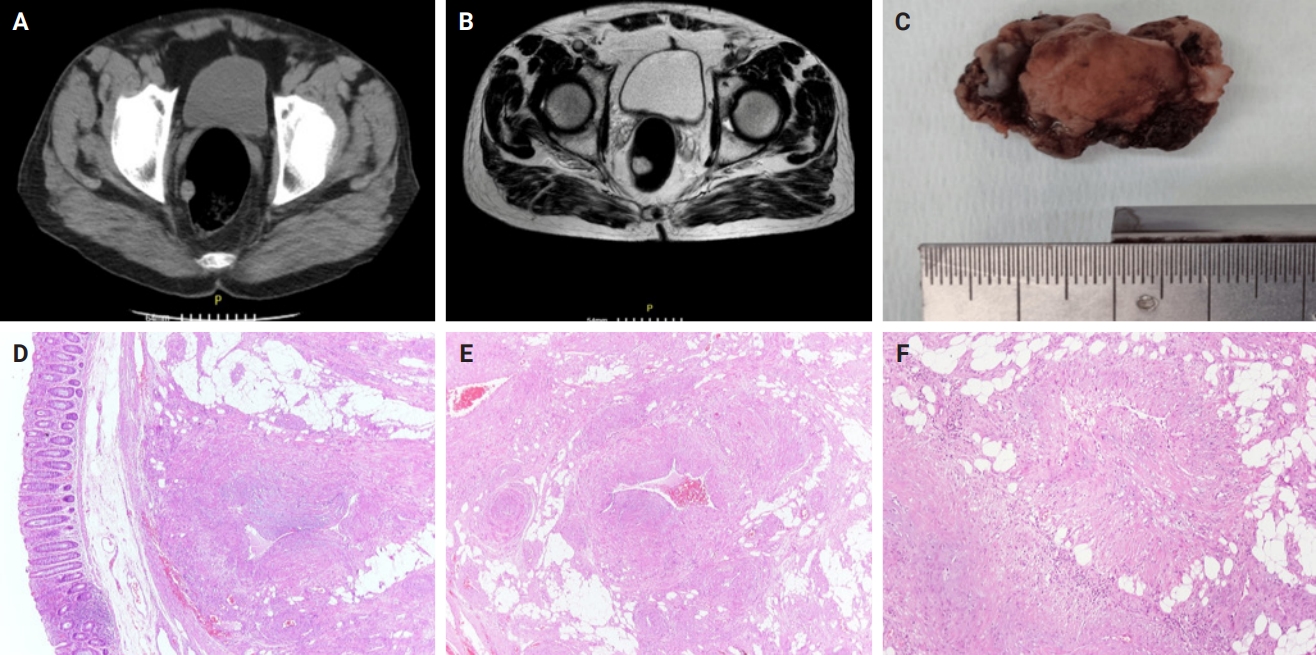






 First
First Prev
Prev



