Search
- Page Path
- HOME > Search
- Histopathological characteristics of Epstein-Barr virus (EBV)–associated encephalitis and colitis in chronic active EBV infection
- Betty A Kasimo, James J Yahaya, Sun Och Yoon, Se Hoon Kim, Minsun Jung
- J Pathol Transl Med. 2025;59(3):188-194. Published online April 16, 2025
- DOI: https://doi.org/10.4132/jptm.2025.02.21
- 4,468 View
- 171 Download
-
 Abstract
Abstract
 PDF
PDF - Chronic active Epstein-Barr virus (CAEBV) can induce complications in various organs, including the brain and gastrointestinal tract. A 3-year-old boy was referred to the hospital with a history of fever and seizures for 15 days. A diagnosis of encephalitis based on computed tomography (CT) and magnetic resonance imaging findings and clinical correlation was made. Laboratory tests showed positive serology for Epstein-Barr virus (EBV) and negative for Rotavirus antigen and IgG and IgM antibodies for cytomegalovirus, herpes simplex virus, and varicella zoster virus, respectively. Abdominal CT showed diffuse wall thickening with fluid distension of small bowel loops, lower abdomen wall thickening, and a small amount of ascites. The biopsy demonstrated positive Epstein-Barr encoding region in situ hybridization in cells within the crypts and lamina propria. The patient was managed with steroids and hematopoietic stem cell transplantation (HSCT). This case showed histopathological characteristics of concurrent EBV-associated encephalitis and colitis in CAEBV infection. The three-step strategy of immunosuppressive therapy, chemotherapy, and allogeneic HSCT should be always be considered for prevention of disease progression.
- Clinical practice recommendations for the use of next-generation sequencing in patients with solid cancer: a joint report from KSMO and KSP
- Miso Kim, Hyo Sup Shim, Sheehyun Kim, In Hee Lee, Jihun Kim, Shinkyo Yoon, Hyung-Don Kim, Inkeun Park, Jae Ho Jeong, Changhoon Yoo, Jaekyung Cheon, In-Ho Kim, Jieun Lee, Sook Hee Hong, Sehhoon Park, Hyun Ae Jung, Jin Won Kim, Han Jo Kim, Yongjun Cha, Sun Min Lim, Han Sang Kim, Choong-Kun Lee, Jee Hung Kim, Sang Hoon Chun, Jina Yun, So Yeon Park, Hye Seung Lee, Yong Mee Cho, Soo Jeong Nam, Kiyong Na, Sun Och Yoon, Ahwon Lee, Kee-Taek Jang, Hongseok Yun, Sungyoung Lee, Jee Hyun Kim, Wan-Seop Kim
- J Pathol Transl Med. 2024;58(4):147-164. Published online January 10, 2024
- DOI: https://doi.org/10.4132/jptm.2023.11.01
- 9,446 View
- 496 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - In recent years, next-generation sequencing (NGS)–based genetic testing has become crucial in cancer care. While its primary objective is to identify actionable genetic alterations to guide treatment decisions, its scope has broadened to encompass aiding in pathological diagnosis and exploring resistance mechanisms. With the ongoing expansion in NGS application and reliance, a compelling necessity arises for expert consensus on its application in solid cancers. To address this demand, the forthcoming recommendations not only provide pragmatic guidance for the clinical use of NGS but also systematically classify actionable genes based on specific cancer types. Additionally, these recommendations will incorporate expert perspectives on crucial biomarkers, ensuring informed decisions regarding circulating tumor DNA panel testing.
-
Citations
Citations to this article as recorded by- Apport de la génomique dans la prise en charge des cancers
Étienne Rouleau, Lucie Karayan-Tapon, Marie-Dominique Galibert, Alexandre Harlé, Isabelle Soubeyran
Revue Francophone des Laboratoires.2025; 2025(568): 67. CrossRef - The Redox–Adhesion–Exosome (RAX) Hub in Cancer: Lipid Peroxidation-Driven EMT Plasticity and Ferroptosis Defense with HNE/MDA Signaling and Lipidomic Perspectives
Moon Nyeo Park, Jinwon Choi, Rosy Iara Maciel de Azambuja Ribeiro, Domenico V. Delfino, Seong-Gyu Ko, Bonglee Kim
Antioxidants.2025; 14(12): 1474. CrossRef
- Apport de la génomique dans la prise en charge des cancers
- Clinicopathologic characterization of cervical metastasis from an unknown primary tumor: a multicenter study in Korea
- Miseon Lee, Uiree Jo, Joon Seon Song, Youn Soo Lee, Chang Gok Woo, Dong-Hoon Kim, Jung Yeon Kim, Sun Och Yoon, Kyung-Ja Cho
- J Pathol Transl Med. 2023;57(3):166-177. Published online May 10, 2023
- DOI: https://doi.org/10.4132/jptm.2023.04.12
- 6,505 View
- 171 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Research regarding cervical metastasis from an unknown primary tumor (CUP) according to human papillomavirus (HPV) and Epstein-Barr virus (EBV) status in Korea has been sporadic and small-scale. This study aims to analyze and understand the characteristics of CUP in Korea according to viral and p16 and p53 status through a multicenter study.
Methods
Ninety-five cases of CUP retrieved from six hospitals in Korea between January 2006 and December 2016 were subjected to high-risk HPV detection (DNA in situ hybridization [ISH] or real-time polymerase chain reaction), EBV detection (ISH), and immunohistochemistry for p16 and p53.
Results
CUP was HPV-related in 37 cases (38.9%), EBV-related in five cases (5.3%), and unrelated to HPV or EBV in 46 cases (48.4%). HPV-related CUP cases had the best overall survival (OS) (p = .004). According to the multivariate analysis, virus-unrelated disease (p = .023) and longer smoking duration (p < .005) were prognostic factors for poor OS. Cystic change (p = .016) and basaloid pattern (p < .001) were more frequent in HPV-related cases, and lymphoepithelial lesion was frequent in EBV-related cases (p = .010). There was no significant association between viral status and p53 positivity (p = .341), smoking status (p = .728), or smoking duration (p = .187). Korean data differ from Western data in the absence of an association among HPV, p53 positivity, and smoking history.
Conclusions
Virus-unrelated CUP in Korea had the highest frequency among all CUP cases. HPV-related CUP is similar to HPV-mediated oropharyngeal cancer and EBVrelated CUP is similar to nasopharyngeal cancer in terms of characteristics, respectively. -
Citations
Citations to this article as recorded by- Management of squamous cell carcinoma of unknown primary in the head and neck: current evidence-based diagnostic and treatment strategies
Marcel Kloppenburg, Matthias Santer, Lukas Schmutzler, Felix Johnson, Benedikt Hofauer, Teresa Steinbichler
memo - Magazine of European Medical Oncology.2026; 19(1): 45. CrossRef - Differenzierung von benignen und malignen Halszysten – eine diagnostische Herausforderung
Christina Sauter, Matthias Sand, Karim Plath, Michaela Maria Plath
Laryngo-Rhino-Otologie.2025; 104(05): 296. CrossRef - Unlocking the Hidden: Advancing Imaging Techniques in Diagnosing Cancers of Unknown Primary in the Head and Neck Region
Daniela Messineo, Filippo Valentini, Giovanni Francesco Niccolini, Federica Zoccali, Francesca Ripari, Enrico Marotta, Marcello Caratozzolo, Pasquale Frisina
Applied Sciences.2025; 15(4): 2194. CrossRef - Characterization of undifferentiated carcinoma of the salivary gland: clinicopathological and immunohistochemical analyses in comparison with lymphoepithelial carcinoma
Sangjoon Choi, Gyuheon Choi, Hee Jin Lee, Joon Seon Song, Yoon Se Lee, Seung-Ho Choi, Kyung-Ja Cho
Journal of Pathology and Translational Medicine.2025; 59(6): 361. CrossRef - Expansion of tumor-infiltrating lymphocytes from head and neck squamous cell carcinoma to assess the potential of adoptive cell therapy
Sangjoon Choi, Mofazzal Hossain, Hyun Lee, Jina Baek, Hye Seon Park, Chae-Lyul Lim, DoYeon Han, Taehyun Park, Jong Hyeok Kim, Gyungyub Gong, Mi-Na Kweon, Hee Jin Lee
Cancer Immunology, Immunotherapy.2024;[Epub] CrossRef
- Management of squamous cell carcinoma of unknown primary in the head and neck: current evidence-based diagnostic and treatment strategies
- Molecular Testing of Lymphoproliferative Disorders: Current Status and Perspectives
- Yoon Kyung Jeon, Sun Och Yoon, Jin Ho Paik, Young A Kim, Bong Kyung Shin, Hyun-Jung Kim, Hee Jeong Cha, Ji Eun Kim, Jooryung Huh, Young-Hyeh Ko
- J Pathol Transl Med. 2017;51(3):224-241. Published online May 10, 2017
- DOI: https://doi.org/10.4132/jptm.2017.04.09
- 22,189 View
- 712 Download
- 14 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Molecular pathologic testing plays an important role for the diagnosis, prognostication and decision of treatment strategy in lymphoproliferative disease. Here, we briefly review the molecular tests currently used for lymphoproliferative disease and those which will be implicated in clinical practice in the near future. Specifically, this guideline addresses the clonality test for B- and T-cell proliferative lesions, molecular cytogenetic tests for malignant lymphoma, determination of cell-of-origin in diffuse large B-cell lymphoma, and molecular genetic alterations incorporated in the 2016 revision of the World Health Organization classification of lymphoid neoplasms. Finally, a new perspective on the next-generation sequencing for diagnostic, prognostic, and therapeutic purpose in malignant lymphoma will be summarized.
-
Citations
Citations to this article as recorded by- Pediatric lymphoproliferative disorders – Emerging insights and management: A narrative review
Emmanuel Ifeanyi Obeagu
Medicine.2026; 105(4): e47367. CrossRef - Presence of minimal residual disease determined by next-generation sequencing is not a reliable prognostic biomarker in children with acute lymphoblastic leukemia
Elizabeta Krstevska Bozhinovikj, Nadica Matevska-Geshkovska, Marija Staninova Stojovska, Emilija Gjorgievska, Aleksandra Jovanovska, Nevenka Ridova, Irina Panovska Stavridis, Svetlana Kocheva, Aleksandar Dimovski
Leukemia & Lymphoma.2025; 66(6): 1121. CrossRef - Haematogenous seeding in mycosis fungoides and Sézary syndrome: current evidence and clinical implications
Robert Gniadecki, Emmanuella Guenova, Christiane Querfeld, Jan P Nicolay, Julia Scarisbrick, Lubomir Sokol
British Journal of Dermatology.2025; 192(3): 381. CrossRef - Exploring External Quality Control Methods for PCR–Polyacrylamide Gel Electrophoresis–Based Lymphocyte Receptor Gene Rearrangement Assays in Korea
Jieun Kim, Ho Hyun Song, Soobin Chae, GeonWoo Choi, Jeong Won Shin
Journal of Laboratory Medicine and Quality Assurance.2025; 47(2): 43. CrossRef - Laboratory analysis of 182 cases of B-cell lymphoproliferative disorders other than typical chronic lymphocytic leukemia: Single-center study
Shams Salah Mahdi, Nuha Abd Ali Al-Sarai
Iraqi Journal of Hematology.2025; 14(2): 218. CrossRef - Assessment of Bone Marrow Involvement in B‐Cell non‐Hodgkin Lymphoma Using Immunoglobulin Gene Rearrangement Analysis with Next‐Generation Sequencing
Min Ji Jeon, Eun Sang Yu, Dae Sik Kim, Chul Won Choi, Ha Nui Kim, Jung Ah Kwon, Soo‐Young Yoon, Jung Yoon
Journal of Clinical Laboratory Analysis.2024;[Epub] CrossRef - Thymus and lung mucosa-associated lymphoid tissue lymphoma with adenocarcinoma of the lung: a case report and literature review
Yu Pang, Daosheng Li, Yiqian Chen, Qinqin Liu, Yuheng Wu, Qingliang Teng, Yuyu Liu
World Journal of Surgical Oncology.2023;[Epub] CrossRef - Development and implementation of an automated and highly accurate reporting process for NGS-based clonality testing
Sean T. Glenn, Phillip M. Galbo, Jesse D. Luce, Kiersten Marie Miles, Prashant K. Singh, Manuel J. Glynias, Carl Morrison
Oncotarget.2023; 14(1): 450. CrossRef - A comparison of capillary electrophoresis and next-generation sequencing in the detection of immunoglobulin heavy chain H and light chain κ gene rearrangements in the diagnosis of classic hodgkin’s lymphoma
Juan-Juan Zhang, Yu-Xin Xie, Li-Lin Luo, Xuan-Tao Yang, Yi-Xing Wang, Yue Cao, Zheng-Bo Long, Wan-Pu Wang
Bioengineered.2022; 13(3): 5868. CrossRef - Lymphoproliferative disorder involving body fluid: diagnostic approaches and roles of ancillary studies
Jiwon Koh, Sun Ah Shin, Ji Ae Lee, Yoon Kyung Jeon
Journal of Pathology and Translational Medicine.2022; 56(4): 173. CrossRef - Diagnostic Workup of Primary Cutaneous B Cell Lymphomas: A Clinician's Approach
Giulia Tadiotto Cicogna, Martina Ferranti, Mauro Alaibac
Frontiers in Oncology.2020;[Epub] CrossRef - Kappa and lambda immunohistochemistry and in situ hybridization in the evaluation of atypical cutaneous lymphoid infiltrates
Alexandra C. Hristov, Nneka I. Comfere, Claudia I. Vidal, Uma Sundram
Journal of Cutaneous Pathology.2020; 47(11): 1103. CrossRef - Primary lung mucosa-associated lymphoid tissue lymphoma accompanied by multiple sclerosis
Ke-Ke Yu, Lei Zhu, Ji-Kai Zhao, Rui-Ying Zhao, Yu-Chen Han
Chinese Medical Journal.2019; 132(13): 1625. CrossRef - Diagnostic accuracy of SOX11 immunohistochemistry in mantle cell lymphoma: A meta-analysis
Woojoo Lee, Eun Shin, Bo-Hyung Kim, Hyunchul Kim, Riccardo Dolcetti
PLOS ONE.2019; 14(11): e0225096. CrossRef - Views of dermatopathologists about clonality assays in the diagnosis of cutaneous T‐cell and B‐cell lymphoproliferative disorders
Nneka Comfere, Uma Sundram, Maria Yadira Hurley, Brian Swick
Journal of Cutaneous Pathology.2018; 45(1): 39. CrossRef - A Next-Generation Sequencing Primer—How Does It Work and What Can It Do?
Yuriy O. Alekseyev, Roghayeh Fazeli, Shi Yang, Raveen Basran, Thomas Maher, Nancy S. Miller, Daniel Remick
Academic Pathology.2018; 5: 2374289518766521. CrossRef
- Pediatric lymphoproliferative disorders – Emerging insights and management: A narrative review
- Long Non-coding RNA HOTAIR Expression in Diffuse Large B-Cell Lymphoma: In Relation to Polycomb Repressive Complex Pathway Proteins and H3K27 Trimethylation
- Eun Ji Oh, Soo Hee Kim, Woo Ick Yang, Young Hyeh Ko, Sun Och Yoon
- J Pathol Transl Med. 2016;50(5):369-376. Published online August 22, 2016
- DOI: https://doi.org/10.4132/jptm.2016.06.06
- 11,158 View
- 174 Download
- 27 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
A long non-coding RNA hox transcript antisense intergenic RNA (HOTAIR) is involved in epigenetic regulation through chromatin remodeling by recruiting polycomb repressive complex 2 (PRC2) proteins (EZH2, SUZ12, and EED) that induce histone H3 trimethylation at lysine 27 (H3K27me3). Deregulation of c-MYC and interaction between c-MYC and EZH2 are well known in lymphomagenesis; however, little is known about the expression status of HOTAIR in diffuse large B-cell lymphomas (DLBCLs).
Methods
The expression status of PRC2 (EZH2, SUZ12, and EED), H3K27me3, c-MYC, and BCL2 was analyzed using immunohistochemistry (n = 231), and HOTAIR was investigated by a quantification real-time polymerase chain reaction method (n = 164) in DLBCLs.
Results
The present study confirmed the positive correlation among PRC2 proteins, H3K27me3, and c-MYC in DLBCLs. Expression level of HOTAIR was also positively correlated to EZH2 (p < .05, respectively). Between c-MYC and HOTAIR, and between c- MYC/BCL2 co-expression and HOTAIR, however, negative correlation was observed in DLBCLs (p < .05, respectively). High level of H3K27me3 was determined as an independent prognostic marker in poor overall survival (hazard ratio, 2.0; p = .023) of DLBCL patients. High expression of HOTAIR, however, was associated with favorable overall survival (p = .004) in the univariate analysis, but the impact was not significant in the multivariate analysis. The favorable outcome of DLBCL with HOTAIR high expression levels may be related to the negative correlation with c- MYC expression or c-MYC/BCL2 co-expression.
Conclusions
HOTAIR expression could be one of possible mechanisms for inducing H3K27me3 via EZH2-related PRC2 activation, and induced H3K27me3 may be strongly related to aggressive DLBCLs which show poor patient outcome. -
Citations
Citations to this article as recorded by- EZH2 Dysregulation and Its Oncogenic Role in Human Cancers
Shiv Verma, Nikita Goyal, Suhani Goyal, Parminder Kaur, Sanjay Gupta
Cancers.2025; 17(19): 3111. CrossRef - HOTAIR in cancer: diagnostic, prognostic, and therapeutic perspectives
Majid Nazari, Emad Babakhanzadeh, Arghavan Mollazadeh, Mohadese Ahmadzade, Elham Mohammadi Soleimani, Elnaz Hajimaqsoudi
Cancer Cell International.2024;[Epub] CrossRef - Long noncoding RNAs (lncRNAs) in human lymphomas
Ali Gholami, Khosro Farhadi, Fatemeh Sayyadipour, Masoud Soleimani, Fakhredin Saba
Genes & Diseases.2022; 9(4): 900. CrossRef - Long noncoding RNAs (lncRNAs) in HIV-mediated carcinogenesis: Role in cell homeostasis, cell survival processes and drug resistance
Lilian Makgoo, Salerwe Mosebi, Zukile Mbita
Non-coding RNA Research.2022; 7(3): 184. CrossRef - Biomedical impact of the expression of HOX locus-associated LncRNAs HOTAIR and HOTTIP in diffuse large B cell lymphoma
Mona Salah Eldin Habieb, Suzy Fawzy Goher, Abd-Elmonem Abd-Elkader El-Torgman, Ibrahim El Tantawy El Sayed, Najlaa Zanati Ali Abd-Elfattah
Human Gene.2022; 34: 201112. CrossRef - Mechanism of LncHOTAIR Regulating Proliferation, Apoptosis, and Autophagy of Lymphoma Cells through hsa-miR-6511b-5p/ATG7 Axis
Fu Gui, Xinyi Yu, Yemeng Wu, Chao Wu, Yulan Zhang, Peng-Yue Zhang
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef -
Circulating RNA biomarkers in diffuse large B-cell lymphoma: a systematic review
Philippe Decruyenaere, Fritz Offner, Jo Vandesompele
Experimental Hematology & Oncology.2021;[Epub] CrossRef - Circulating long non-coding RNAs HOTAIR, Linc-p21, GAS5 and XIST expression profiles in diffuse large B-cell lymphoma: association with R-CHOP responsiveness
Mahmoud A. Senousy, Aya M. El-Abd, Raafat R. Abdel-Malek, Sherine M. Rizk
Scientific Reports.2021;[Epub] CrossRef - An immunotherapeutic approach to decipher the role of long non-coding RNAs in cancer progression, resistance and epigenetic regulation of immune cells
Krishnapriya M. Varier, Hemavathi Dhandapani, Wuling Liu, Jialei Song, Chunlin Wang, Anling Hu, Yaacov Ben-David, Xiangchun Shen, Yanmei Li, Babu Gajendran
Journal of Experimental & Clinical Cancer Research.2021;[Epub] CrossRef - Cancer‑associated fibroblast‑derived CCL5 contributes to cisplatin resistance in A549 NSCLC cells partially through upregulation of lncRNA HOTAIR expression
Xiangjun Sun, Zhijie Chen
Oncology Letters.2021;[Epub] CrossRef - Competitive Endogenous RNA Network Involving miRNA and lncRNA in Non-Hodgkin Lymphoma: Current Advances and Clinical Perspectives
Mara Fernandes, Herlander Marques, Ana Luísa Teixeira, Rui Medeiros
Biomedicines.2021; 9(12): 1934. CrossRef - EZH2 expression is dependent on MYC and TP53 regulation in diffuse large B‐cell lymphoma
Eduardo Henrique Neves Filho, Carlos Gustavo Hirth, Igor Allen Frederico, Rommel Mario Burbano, Thiago Carneiro, Silvia Helena Rabenhorst
APMIS.2020; 128(4): 308. CrossRef Long Noncoding RNAs in Diffuse Large B-Cell Lymphoma: Current Advances and Perspectives
Xianbo Huang, Wenbin Qian, Xiujin Ye
OncoTargets and Therapy.2020; Volume 13: 4295. CrossRef- Lnc SMAD5-AS1 as ceRNA inhibit proliferation of diffuse large B cell lymphoma via Wnt/β-catenin pathway by sponging miR-135b-5p to elevate expression of APC
Chen-Chen Zhao, Yang Jiao, Yi-Yin Zhang, Jie Ning, Yi-Ruo Zhang, Jing Xu, Wei Wei, Gu Kang-Sheng
Cell Death & Disease.2019;[Epub] CrossRef - H3K18Ac as a Marker of Cancer Progression and Potential Target of Anti-Cancer Therapy
Marta Hałasa, Anna Wawruszak, Alicja Przybyszewska, Anna Jaruga, Małgorzata Guz, Joanna Kałafut, Andrzej Stepulak, Marek Cybulski
Cells.2019; 8(5): 485. CrossRef - HOTAIR as a Prognostic Predictor for Diverse Human Cancers: A Meta- and Bioinformatics Analysis
Halil Ibrahim Toy, Didem Okmen, Panagiota I. Kontou, Alexandros G. Georgakilas, Athanasia Pavlopoulou
Cancers.2019; 11(6): 778. CrossRef - Long Noncoding RNA HOTAIR Promotes Endometrial Carcinoma Cell Proliferation by Binding to PTEN via the Activating Phosphatidylinositol 3-Kinase/Akt Signaling Pathway
Xiao-Hui Zhang, Pin Hu, Yang-Qin Xie, Yong-Jun Kang, Min Li
Molecular and Cellular Biology.2019;[Epub] CrossRef - EZH2 abnormalities in lymphoid malignancies: underlying mechanisms and therapeutic implications
Boheng Li, Wee-Joo Chng
Journal of Hematology & Oncology.2019;[Epub] CrossRef - The prognostic impact of long noncoding RNA HOTAIR in leukemia and lymphoma: a meta-analysis
Yun Lin, Zhihong Fang, Zhijuan Lin, Zhifeng Li, Jintao Zhao, Yiming Luo, Bing Xu
Hematology.2018; 23(9): 600. CrossRef - Retracted: Downregulation of Long Noncoding RNA HOTAIR and EZH2 Induces Apoptosis and Inhibits Proliferation, Invasion, and Migration of Human Breast Cancer Cells
Lu Han, Hai-Chao Zhang, Li Li, Cai-Xia Li, Xu Di, Xin Qu
Cancer Biotherapy and Radiopharmaceuticals.2018; 33(6): 241. CrossRef - Long Non-Coding RNAs Guide the Fine-Tuning of Gene Regulation in B-Cell Development and Malignancy
Mette Dahl, Lasse Sommer Kristensen, Kirsten Grønbæk
International Journal of Molecular Sciences.2018; 19(9): 2475. CrossRef - HOTAIR, a long noncoding RNA, is a marker of abnormal cell cycle regulation in lung cancer
Minghui Liu, Hongyi Zhang, Ying Li, Rui Wang, Yongwen Li, Hongbing Zhang, Dian Ren, Hongyu Liu, Chunsheng Kang, Jun Chen
Cancer Science.2018; 109(9): 2717. CrossRef - The evolving concept of cancer stem-like cells in thyroid cancer and other solid tumors
Heather Hardin, Ranran Zhang, Holly Helein, Darya Buehler, Zhenying Guo, Ricardo V Lloyd
Laboratory Investigation.2017; 97(10): 1142. CrossRef - Emerging roles for long noncoding RNAs in B-cell development and malignancy
M. Winkle, J.L. Kluiver, A. Diepstra, A. van den Berg
Critical Reviews in Oncology/Hematology.2017; 120: 77. CrossRef
- EZH2 Dysregulation and Its Oncogenic Role in Human Cancers
- Upregulated Neuro-oncological Ventral Antigen 1 (NOVA1) Expression Is Specific to Mature and Immature T- and NK-Cell Lymphomas
- Eun Kyung Kim, Sun Och Yoon, Soo Hee Kim, Woo Ick Yang, Yoon Ah Cho, Soo Jeong Kim
- J Pathol Transl Med. 2016;50(2):104-112. Published online February 29, 2016
- DOI: https://doi.org/10.4132/jptm.2016.02.08
- 11,348 View
- 72 Download
- 14 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Recent studies have revealed that the splicing factor neuro-oncological ventral antigen 1 (NOVA1) is enriched in fibroblasts and accumulated T cells of tertiary lymphoid structures. In the present study, we investigated NOVA1 expression in various subtypes of mature and immature T- and natural killer (NK)-cell lymphomas as well as in various B-cell lymphoma subtypes. Methods: NOVA1 immunoexpression was evaluated in hyperplastic palatine tonsils (n = 20), T- and NK-cell lymphomas (n = 177), diffuse large B-cell lymphomas (n = 151), and other types of B cell lymphomas (n = 31). Nuclear staining intensity and percentage of positive tumor cells were graded. NOVA1 mRNA expression was analyzed in various lymphoma cell lines. Results: Tumor cells of T- and NK-cell lymphomas showed higher expression levels of NOVA1 than did normal paracortical T cells, and 56.5% of T- and NK-cell lymphoma cases showed diffuse and strong expression. The NOVA1 expression level varied according to the subtype; it was higher in angioimmunoblastic T-cell lymphoma, anaplastic lymphoma kinase (ALK)-negative anaplastic large cell lymphoma (ALCL), and T lymphoblastic leukemia/lymphoma (T-LBL), but it was lower in ALK-positive ALCL. In almost all B-cell lymphomas, NOVA1 expression was very low or negative. NOVA1 mRNA was also expressed in Jurkat, a T-LBL cell line. Conclusions: The present findings suggest that NOVA1 upregulation may be involved in certain subtypes of T- and NK-cell lymphomas, but not in B-cell lymphomas. Upregulated NOVA1 expression seems to be a specific biological feature of activated T cells such as T- and NK-cell lymphomas. -
Citations
Citations to this article as recorded by- Intraoperative pathologic diagnosis of central nervous system lymphomas: A comparison of frozen and permanent section diagnoses, and the significance of preoperative imaging
Aslı Kahraman, Fikret Dirilenoğlu, İsmail Güzeliş, Kenan Çetinoğlu
Annals of Diagnostic Pathology.2024; 69: 152246. CrossRef - NOVA1 acts on Impact to regulate hypothalamic function and translation in inhibitory neurons
Yoko Tajima, Keiichi Ito, Yuan Yuan, Mayu O. Frank, Yuhki Saito, Robert B. Darnell
Cell Reports.2023; 42(2): 112050. CrossRef - MicroRNA miR-27a-3p accelerates cardiac hypertrophy by targeting neuro-oncological ventral antigen 1
Dongyun Li, Mingzhi Shen, Xinxin Deng, Yongyi Bai
Bioengineered.2022; 13(4): 8982. CrossRef - NOVA1 promotes NSCLC proliferation and invasion by activating Wnt/β-catenin signaling
Lianyue Qu, Yulong Tian, Fan Wang, Zixuan Li
BMC Cancer.2022;[Epub] CrossRef - Identification of the Functions and Prognostic Values of RNA Binding Proteins in Bladder Cancer
Yue Wu, Zheng Liu, Xian Wei, Huan Feng, Bintao Hu, Bo Liu, Yang Luan, Yajun Ruan, Xiaming Liu, Zhuo Liu, Shaogang Wang, Jihong Liu, Tao Wang
Frontiers in Genetics.2021;[Epub] CrossRef - Nervous system and gastric cancer
Ke Wang, Xin-hui Zhao, Jun Liu, Rui Zhang, Ji-peng Li
Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.2020; 1873(1): 188313. CrossRef - The RNA-binding protein RBM47 inhibits non-small cell lung carcinoma metastasis through modulation of AXIN1 mRNA stability and Wnt/β-catentin signaling
Di-jian Shen, You-hua Jiang, Jian-qiang Li, Li-wei Xu, Kai-yi Tao
Surgical Oncology.2020; 34: 31. CrossRef - Genome-Wide Profiling of Cervical RNA-Binding Proteins Identifies Human Papillomavirus Regulation of RNASEH2A Expression by Viral E7 and E2F1
Junfen Xu, Habin Liu, Yanqin Yang, Xiaohong Wang, Poching Liu, Yang Li, Craig Meyers, Nilam Sanjib Banerjee, Hsu-Kun Wang, Maggie Cam, Weiguo Lu, Louise T. Chow, Xing Xie, Jun Zhu, Zhi-Ming Zheng, Xiang-Jin Meng, James Pipas, Xuefeng Liu, Lucia Pirisi-cre
mBio.2019;[Epub] CrossRef - NOVA1 induction by inflammation and NOVA1 suppression by epigenetic regulation in head and neck squamous cell carcinoma
Eun Kyung Kim, Yoon Ah Cho, Mi-kyoung Seo, Hyunmi Ryu, Byoung Chul Cho, Yoon Woo Koh, Sun Och Yoon
Scientific Reports.2019;[Epub] CrossRef - The RNA binding protein neuro‐oncological ventral antigen 1 (NOVA1) regulates IL-6 mRNA stability to enhance JAK2-STAT3 signaling in CRC
Yong-gang Hong, Guo-shu Xu, Guan-yu Yu, Ji-dian Zhou, Qi-zhi Liu, Jun-sheng Ni, Hong-li Yan, Wei Zhang, Li-qiang Hao
Surgical Oncology.2019; 31: 67. CrossRef - NOVA1 acts as an oncogene in melanoma via regulating FOXO3a expression
Xin Yu, Heyi Zheng, Matthew T.V. Chan, William K.K. Wu
Journal of Cellular and Molecular Medicine.2018; 22(5): 2622. CrossRef - Neuro‐oncological ventral antigen 1 (NOVA1): Implications in neurological diseases and cancers
Yu Xin, Zheng Li, Heyi Zheng, Jeffery Ho, Matthew T. V. Chan, William K. K. Wu
Cell Proliferation.2017;[Epub] CrossRef - New developments in the pathology of malignant lymphoma. A review of the literature published from January–April 2016
J. Han van Krieken
Journal of Hematopathology.2016; 9(2): 73. CrossRef
- Intraoperative pathologic diagnosis of central nervous system lymphomas: A comparison of frozen and permanent section diagnoses, and the significance of preoperative imaging
- Proposal of an Appropriate Decalcification Method of Bone Marrow Biopsy Specimens in the Era of Expanding Genetic Molecular Study
- Sung-Eun Choi, Soon Won Hong, Sun Och Yoon
- J Pathol Transl Med. 2015;49(3):236-242. Published online May 15, 2015
- DOI: https://doi.org/10.4132/jptm.2015.03.16
- 19,588 View
- 354 Download
- 56 Web of Science
- 58 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The conventional method for decalcification of bone specimens uses hydrochloric acid (HCl) and is notorious for damaging cellular RNA, DNA, and proteins, thus complicating molecular and immunohistochemical analyses. A method that can effectively decalcify while preserving genetic material is necessary. Methods: Pairs of bilateral bone marrow biopsies sampled from 53 patients were decalcified according to protocols of two comparison groups: EDTA versus HCl and RDO GOLD (RDO) versus HCl. Pairs of right and left bone marrow biopsy samples harvested from 28 cases were allocated into the EDTA versus HCl comparison group, and 25 cases to the RDO versus HCl comparison group. The decalcification protocols were compared with regards to histomorphology, immunohistochemistry, and molecular analysis. For molecular analysis, we randomly selected 5 cases from the EDTA versus HCl and RDO versus HCl groups. Results: The decalcification time for appropriate histomorphologic analysis was the longest in the EDTA method and the shortest in the RDO method. EDTA was superior to RDO or HCl in DNA yield and integrity, assessed via DNA extraction, polymerase chain reaction, and silver in situ hybridization using DNA probes. The EDTA method maintained intact nuclear protein staining on immunohistochemistry, while the HCl method produced poor quality images. Staining after the RDO method had equivocal results. RNA in situ hybridization using kappa and lambda RNA probes measured RNA integrity; the EDTA and RDO method had the best quality, followed by HCl. Conclusions: The EDTA protocol would be the best in preserving genetic material. RDO may be an acceptable alternative when rapid decalcification is necessary. -
Citations
Citations to this article as recorded by- Seeing beyond the surface: bone histomorphometry re-visited—implications for diagnostic pathology
Terrence Diamond, Cherie Chiang, Grahame J. Elder
Pathology.2026; 58(2): 230. CrossRef - Evaluation of the protective effect of the Echinacea Purpurea against apoptosis and inflammation induced by overdose of iron dextran on the hematopoietic system
Doaa Kahim Abdul Ridha, Ali Faris Hassan
Journal of Complementary and Integrative Medicine.2026;[Epub] CrossRef - Germline and somatic testing for homologous repair deficiency in patients with prostate cancer (part 1 of 2)
Andrew J. Armstrong, Amy Taylor, Michael C. Haffner, Wassim Abida, Alan H. Bryce, Lawrence I. Karsh, Scott T. Tagawa, Przemyslaw Twardowski, Anthony V. Serritella, Joshua M. Lang
Prostate Cancer and Prostatic Diseases.2025; 28(3): 652. CrossRef - Spatial transcriptomic approaches for characterising the bone marrow landscape: pitfalls and potential
Rosalin A. Cooper, Emily Thomas, Anna M. Sozanska, Carlo Pescia, Daniel J. Royston
Leukemia.2025; 39(2): 291. CrossRef - Qualitative comparison of decalcifiers for mouse bone cryosections for subsequent biophotonic analysis
Shibarjun Mandal, Ramya Motganhalli Ravikumar, Astrid Tannert, Annett Urbanek, Rustam R. Guliev, Max Naumann, Sina M. Coldewey, Uta Dahmen, Lina Carvalho, Luís Bastião Silva, Ute Neugebauer
Scientific Reports.2025;[Epub] CrossRef - Spatial Platform for Periodontal Ligament Angulation and Regeneration: In Vivo Pilot Study
Min Guk Kim, Do-Yeon Kim, Hyoung-Gon Ko, Jin-Seok Byun, Joong-Hyun Kim, Chan Ho Park
Journal of Functional Biomaterials.2025; 16(3): 99. CrossRef - Spatial proteomics and transcriptomics characterization of tissue and multiple cancer types including decalcified marrow
Cecilia CS Yeung, Daniel C Jones, David W. Woolston, Brandon Seaton, Elizabeth Lawless Donato, Minggang Lin, Coral Backman, Vivian Oehler, Kristin L Robinson, Kristen Shimp, Rima Kulikauskas, Annalyssa N Long, David Sowerby, Anna E Elz, Kimberly S Smythe,
Cancer Biomarkers.2025;[Epub] CrossRef - Circulating tumor cell markers for early detection and drug resistance assessment through liquid biopsy
Priya Yadav, Saravanan Rajendrasozhan, Ramzi Hadj Lajimi, Raja Ramadevi Patel, Dominique Heymann, N. Rajendra Prasad
Frontiers in Oncology.2025;[Epub] CrossRef - Morphological Bone Score as a Predictive Tool for Molecular Profiling Success
Kirill Kriukov, Dmitry Ivchenkov, Anna Bejanyan, Aleksandr Sarachakov, Aleksandra Kviatkovskaia, Gleb Khegai, Dominique Knipper-Davis, Amber Berlinski, Tayla Soares, Jochen K. Lennerz, Vladimir Kushnarev
The Journal of Molecular Diagnostics.2025; 27(8): 747. CrossRef - Optimizing cytology and small biopsy specimen processing for ancillary studies: recommendations from the American Society of Cytopathology taskforce
Sinchita Roy-Chowdhuri, Christine N. Booth, Jonas J. Heymann, Elizabeth Jenkins, Joshua R. Menke, Sara E. Monaco, Ritu Nayar, Michiya Nishino, Roberto Ruiz-Cordero, Donna K. Russell, Anjali Saqi, Kaitlin E. Sundling, Michael J. Thrall, Vanda F. Torous, Ch
Journal of the American Society of Cytopathology.2025; 14(5): 285. CrossRef - Ethylenediaminetetraacetic Acid (EDTA)-Decalcified, Formalin-Fixed Paraffin-Embedded (FFPE) Tumor Tissue Shows Comparable Quality and Quantity of DNA to Non-Decalcified Tissue in Next-Generation Sequencing (NGS)
Francis Hong Xin Yap, Jen-Hwei Sng, Jeremy Wee Kiat Ng, Hanis Abdul Kadir, Pei Yi Chan, Timothy Kwang Yong Tay
Journal of Molecular Pathology.2025; 6(3): 21. CrossRef - Case Report: Pitfalls in bone marrow evaluation: importance of adequate bone marrow sampling
Alireza Ghezavati, Elham Vali Betts, Ananya Datta Mitra
Frontiers in Oncology.2025;[Epub] CrossRef - Optimization of Formic Acid-Formalin-Based Decalcification Protocol for Rat Calvarial Bone Histology
S. Amitha Banu, Khan Sharun, Merlin Mamachan, Athira Subash, Vadapalli Deekshita, Kirtika Sharma, Karikalan Mathesh, Obli Rajendran Vinodh kumar, Swapan Kumar Maiti, Abhijit M. Pawde, Laith Abualigah, Kuldeep Dhama, Amarpal
Journal of Experimental Biology and Agricultural Sciences.2024; 12(2): 218. CrossRef - Effects of fixation and demineralization on histomorphology and DNA amplification of canine bone marrow
Gabriella M. L. Diamantino, Janet Beeler-Marfisi, Robert A. Foster, William Sears, Alice Defarges, William Vernau, Dorothee Bienzle
Veterinary Pathology.2024; 61(6): 943. CrossRef - In situ metabolomic analysis of osteonecrosis of the femoral head (ONFH) using MALDI MSI
Chen Li, Jikun Liu, Yiqi Sheng, Yinghao Wang, Lan Jia, Yinguang Zhang, Jiantao Li, Shuangshuang Di, Honggang Nie, Yehua Han
Analytical and Bioanalytical Chemistry.2024; 416(23): 5155. CrossRef - A set of pretreatment reagents including improved formula fixation and decalcification facilitating immunohistochemistry and DNA analyses of formalin-fixed paraffin-embedded bone marrow trephine biopsy
Ting Sun, Liming Xu, Hongtian Yao, Jing Zhao, Zhen Chen, Zexin Chen, Bo Wang, Wei Ding
Acta Histochemica.2024; 126(8): 152188. CrossRef - To Freeze or Not to Freeze? Recommendations for Intraoperative Examination and Gross Prosection of Thyroid Glands
Fouad R. Zakka, Nicole A. Cipriani
Surgical Pathology Clinics.2023; 16(1): 15. CrossRef - Effect of Surface Decalcification With Hydrochloric Acid on the Determination of Estrogen Receptor, Progesterone Receptor, Ki67, and Human Epidermal Growth Factor Receptor 2 Expressions in Invasive Breast Carcinoma Based on Immunohistochemistry and Fluore
Wu Ping, Rao Xin, Zhang Li, Chen Yupeng, Song Fangling, Ren Caihong, Hu Shun, Zhang Sheng
Applied Immunohistochemistry & Molecular Morphology.2023; 31(4): 232. CrossRef - Diagnostic value of MDM2 RNA in situ hybridization for low-grade osteosarcoma: Consistency comparison of RNA in situ hybridization, fluorescence in situ hybridization, and immunohistochemistry
Chen Chen, Xin He, Min Chen, Tianhai Du, Weiji Qin, Wenyi Jing, Hongying Zhang
Virchows Archiv.2023; 482(6): 999. CrossRef - Bone marrow fibrosis is associated with non‐response to CD19 CAR T‐cell therapy in B‐acute lymphoblastic leukemia
Joshua Anil, Ahab Alnemri, Andrew Lytle, Brian Lockhart, Ashley E. Anil, Michael Baumgartner, Kirubel Gebre, Jared McFerran, Stephan A. Grupp, Susan R. Rheingold, Vinodh Pillai
American Journal of Hematology.2023; 98(12): 1888. CrossRef - Epithelioid haemangioendothelioma of the mandible – A case report and review of the literature
Ali Rizvi, Tim K. Blackburn, Guy N. J. Betts
Oral Surgery.2022; 15(3): 387. CrossRef - Evaluation of EDTA and nitric acid solutions for decalcification of joints in AG/WT, BALB/c, C57, DBA1/J mice, and in Wistar rats
Eduarda Correa Freitas, Suelen Pizzolatto Dalmolin, Mateus Müller da Silva, Francine Hehn de Oliveira, Emily Ferreira Salles Pilar
Biotechnic & Histochemistry.2022; 97(5): 372. CrossRef - Coupling Lipid Labeling and Click Chemistry Enables Isolation of Extracellular Vesicles for Noninvasive Detection of Oncogenic Gene Alterations
Na Sun, Benjamin V. Tran, Zishan Peng, Jing Wang, Ceng Zhang, Peng Yang, Tiffany X. Zhang, Josephine Widjaja, Ryan Y. Zhang, Wenxi Xia, Alexandra Keir, Jia‐Wei She, Hsiao‐hua Yu, Jing‐Jong Shyue, Hongguang Zhu, Vatche G. Agopian, Renjun Pei, James S. Toml
Advanced Science.2022;[Epub] CrossRef - The Expressions of CD30 and CD123 of Mastocytosis in Taiwan
Ching-Fen Yang, Chih-Yi Hsu
Applied Immunohistochemistry & Molecular Morphology.2022; 30(4): 278. CrossRef - Unusual Patterns of HER2 Expression in Breast Cancer: Insights and Perspectives
Dora Grassini, Eliano Cascardi, Ivana Sarotto, Laura Annaratone, Anna Sapino, Enrico Berrino, Caterina Marchiò
Pathobiology.2022; 89(5): 278. CrossRef - Expert opinion on NSCLC small specimen biomarker testing — Part 1: Tissue collection and management
Frédérique Penault-Llorca, Keith M. Kerr, Pilar Garrido, Erik Thunnissen, Elisabeth Dequeker, Nicola Normanno, Simon J. Patton, Jenni Fairley, Joshua Kapp, Daniëlle de Ridder, Aleš Ryška, Holger Moch
Virchows Archiv.2022; 481(3): 335. CrossRef - Comparison of bone demineralisation procedures for DNA recovery from burned remains
Meghan Mckinnon, Denice Higgins
Forensic Science International: Genetics.2021; 51: 102448. CrossRef - A review of the current understanding of burned bone as a source of DNA for human identification
Meghan Mckinnon, Maciej Henneberg, Denice Higgins
Science & Justice.2021; 61(4): 332. CrossRef - Time is bone — Quantitative comparison of decalcification solvents in human femur samples using dual-X-ray-absorptiometry and computed tomography
Joshua Gawlitza, Jakob Steinhäuser, Arno Bücker, Gabriela Krasteva-Christ, Thomas Tschernig
Annals of Anatomy - Anatomischer Anzeiger.2021; 235: 151696. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Effect of EDTA decalcification on estrogen receptor and progesterone receptor immunohistochemistry and HER2/neu fluorescence in situ hybridization in breast carcinoma
Erik Washburn, Xiaoyu Tang, Carla Caruso, Michelle Walls, Bing Han
Human Pathology.2021; 117: 108. CrossRef - Performances of single tube nested polymerase chain reaction and GeneXpert ultra on Formalin fixed paraffin embedded tissues in the diagnosis of tuberculous spondylodiscitis
Emna Romdhane, Soumaya Rammeh, Chelli Mouna Bouaziz, Hend Riahi, Meriam Rekaya Ben, Meriam Ksentini, Yosra Chebbi, Wafa Achour, Asma Ferjani, Ben Boubaker Ilhem Boutiba, Leila Slim-Saidi, Mohamed Fethi Ladeb
Clinical Rheumatology.2021; 40(10): 4317. CrossRef - Molecular Characterization of Prostate Cancers in the Precision Medicine Era
Emilio Francesco Giunta, Laura Annaratone, Enrico Bollito, Francesco Porpiglia, Matteo Cereda, Giuseppe Luigi Banna, Alessandra Mosca, Caterina Marchiò, Pasquale Rescigno
Cancers.2021; 13(19): 4771. CrossRef - Increased NF-κB Activity in Osteoprogenitor-Lineage Cells Impairs the Balance of Bone Versus Fat in the Marrow of Skeletally Mature Mice
Tzuhua Lin, Jukka Pajarinen, Yusuke Kohno, Akira Nabeshima, Laura Lu, Karthik Nathan, Zhenyu Yao, Joy Y. Wu, Stuart Goodman
Regenerative Engineering and Translational Medicine.2020; 6(1): 69. CrossRef - Percutaneous CT-guided biopsy of lytic bone lesions in patients clinically suspected of lung cancer: Diagnostic performances for pathological diagnosis and molecular testing
Anne-Claire Toffart, Stéphane Asfari, Anne Mc Leer, Emilie Reymond, Adrien Jankowski, Denis Moro-Sibilot, Olivier Stephanov, Julien Ghelfi, Sylvie Lantuejoul, Gilbert R. Ferretti
Lung Cancer.2020; 140: 93. CrossRef - Effect of decalcification protocols on immunohistochemistry and molecular analyses of bone samples
Elodie Miquelestorena-Standley, Marie-Lise Jourdan, Christine Collin, Corinne Bouvier, Frédérique Larousserie, Sébastien Aubert, Anne Gomez-Brouchet, Jean-Marc Guinebretière, Matthias Tallegas, Bénédicte Brulin, Louis-Romée Le Nail, Anne Tallet, François
Modern Pathology.2020; 33(8): 1505. CrossRef - Identifying Opportunities and Challenges for Patients With Sarcoma as a Result of Comprehensive Genomic Profiling of Sarcoma Specimens
Margaret A. Hay, Eric A. Severson, Vincent A. Miller, David A. Liebner, Jo-Anne Vergilio, Sherri Z. Millis, James L. Chen
JCO Precision Oncology.2020; (4): 176. CrossRef - Comparison of Methods for the Histological Evaluation of Odontocete Spiral Ganglion Cells
Tania Ramírez, Simona Sacchini, Yania Paz, Rubén S. Rosales, Nakita Câmara, Marisa Andrada, Manuel Arbelo, Antonio Fernández
Animals.2020; 10(4): 683. CrossRef - Molecular Pathology of Primary Non-small Cell Lung Cancer
David Ilan Suster, Mari Mino-Kenudson
Archives of Medical Research.2020; 51(8): 784. CrossRef - Comparison of ethylenediaminetetraacetic acid and rapid decalcificier solution for studying human temporal bones by immunofluorescence
Sumana Ghosh, Mark B. Lewis, Bradley J. Walters
Laryngoscope Investigative Otolaryngology.2020; 5(5): 919. CrossRef - A novel cryo-embedding method for in-depth analysis of craniofacial mini pig bone specimens
Pavla Ticha, Igor Pilawski, Xue Yuan, Jie Pan, Ustun S. Tulu, Benjamin R. Coyac, Waldemar Hoffmann, Jill A. Helms
Scientific Reports.2020;[Epub] CrossRef - Accelerating precision medicine in metastatic prostate cancer
Joaquin Mateo, Rana McKay, Wassim Abida, Rahul Aggarwal, Joshi Alumkal, Ajjai Alva, Felix Feng, Xin Gao, Julie Graff, Maha Hussain, Fatima Karzai, Bruce Montgomery, William Oh, Vaibhav Patel, Dana Rathkopf, Matthew Rettig, Nikolaus Schultz, Matthew Smith,
Nature Cancer.2020; 1(11): 1041. CrossRef - Tissue Morphology and Antigenicity in Mouse and Rat Tibia: Comparing 12 Different Decalcification Conditions
Kristofor Bogoevski, Anna Woloszyk, Keith Blackwood, Maria A. Woodruff, Vaida Glatt
Journal of Histochemistry & Cytochemistry.2019; 67(8): 545. CrossRef - Cellular and collagen reference values of gingival and periodontal ligament tissues in rats: a pilot study
Antoine Alves, Nina Attik, Carine Wirth, Yves Bayon, Alexis Piat, Brigitte Grosgogeat, Kerstin Gritsch
Histochemistry and Cell Biology.2019; 152(2): 145. CrossRef - Implementing Precision Medicine Programs and Clinical Trials in the Community-Based Oncology Practice: Barriers and Best Practices
Jennifer L. Ersek, Lora J. Black, Michael A. Thompson, Edward S. Kim
American Society of Clinical Oncology Educational Book.2018; (38): 188. CrossRef - Integration of next-generation sequencing in clinical diagnostic molecular pathology laboratories for analysis of solid tumours; an expert opinion on behalf of IQN Path ASBL
Zandra C Deans, Jose Luis Costa, Ian Cree, Els Dequeker, Anders Edsjö, Shirley Henderson, Michael Hummel, Marjolijn JL Ligtenberg, Marco Loddo, Jose Carlos Machado, Antonio Marchetti, Katherine Marquis, Joanne Mason, Nicola Normanno, Etienne Rouleau, Ed S
Virchows Archiv.2017; 470(1): 5. CrossRef - Protocolo para el estudio de muestras y estandarización del informe patológico de tumores óseos
Isidro Machado, José Juan Pozo, David Marcilla, Julia Cruz, Juan C. Tardío, Aurora Astudillo, Sílvia Bagué
Revista Española de Patología.2017; 50(1): 34. CrossRef - Extremely Well-Differentiated Papillary Thyroid Carcinoma Resembling Adenomatous Hyperplasia Can Metastasize to the Skull: A Case Report
Ju Yeon Pyo, Jisup Kim, Sung-eun Choi, Eunah Shin, Seok-Woo Yang, Cheong Soo Park, Seok-Mo Kim, SoonWon Hong
Yonsei Medical Journal.2017; 58(1): 255. CrossRef - Treatment of steroid-induced osteonecrosis of the femoral head using porous Se@SiO2 nanocomposites to suppress reactive oxygen species
Guoying Deng, Kerun Niu, Feng Zhou, Buxiao Li, Yingjie Kang, Xijian Liu, Junqing Hu, Bo Li, Qiugen Wang, Chengqing Yi, Qian Wang
Scientific Reports.2017;[Epub] CrossRef - Precision Medicine Starts With Preanalytics: Real-Time Assessment of Tissue Fixation Quality by Ultrasound Time-of-Flight Analysis
Melissa L. Lerch, Daniel R. Bauer, David Chafin, Abbey Theiss, Michael Otter, Geoffrey S. Baird
Applied Immunohistochemistry & Molecular Morphology.2017; 25(3): 160. CrossRef - Good Laboratory Standards for Clinical Next-Generation Sequencing Cancer Panel Tests
Jihun Kim, Woong-Yang Park, Nayoung K. D. Kim, Se Jin Jang, Sung-Min Chun, Chang-Ohk Sung, Jene Choi, Young-Hyeh Ko, Yoon-La Choi, Hyo Sup Shim, Jae-Kyung Won
Journal of Pathology and Translational Medicine.2017; 51(3): 191. CrossRef - An international survey about nail histology processing techniques
Christina Wlodek, Pauline Lecerf, Josette Andre, Beth S. Ruben, David de Berker
Journal of Cutaneous Pathology.2017; 44(9): 749. CrossRef - pSTAT5 and ERK exhibit different expression in myeloproliferative neoplasms
Ewa Wiśniewska-Chudy, Łukasz Szylberg, Grzegorz Dworacki, Ewa Mizera-Nyczak, Andrzej Marszałek
Oncology Reports.2017; 37(4): 2295. CrossRef - How we do: optimizing bone marrow biopsy logistics for sign-out within 2 days
I. de Laak–de Vries, A. G. Siebers, L. Burgers, C. Diepenbroek, M. Link, P. Groenen, J. H. J. M. van Krieken, K. M. Hebeda
Journal of Hematopathology.2016; 9(2): 67. CrossRef - Do More With Less: Tips and Techniques for Maximizing Small Biopsy and Cytology Specimens for Molecular and Ancillary Testing: The University of Colorado Experience
Dara L. Aisner, Mathew D. Rumery, Daniel T. Merrick, Kimi L. Kondo, Hala Nijmeh, Derek J. Linderman, Robert C. Doebele, Natalie Thomas, Patrick C. Chesnut, Marileila Varella-Garcia, Wilbur A. Franklin, D. Ross Camidge
Archives of Pathology & Laboratory Medicine.2016; 140(11): 1206. CrossRef - Analysis of the Effects of Bone Marrow Biopsy Decalcification Methods on Histopathological Examination
Ji Young Park, Kyung Hee Han
The Korean Journal of Clinical Laboratory Science.2016; 48(4): 371. CrossRef - Distinguishing between Microbial Habitats Unravels Ecological Complexity in Coral Microbiomes
Amy Apprill, Laura G. Weber, Alyson E. Santoro, Nicole S. Webster
mSystems.2016;[Epub] CrossRef - Optimal Fixation and Decalcification Methods for Bone Marrow Biopsy
Myung-Sub Choi, Hyunsup Lee, Hyuk-Chul Kwon, Moon-Hwan Bae, Young-Hye Ko, Hee-Jin Kim, Beom-Se Lee, Bon-Kyung Koo
Korean Journal of Clinical Laboratory Science.2015; 47(4): 243. CrossRef
- Seeing beyond the surface: bone histomorphometry re-visited—implications for diagnostic pathology
- The Limitations of Endoscopic Ultrasound-Guided Fine Needle Aspiration Cytology in the Diagnosis of Pancreatic Serous Cystadenoma: A Brief Case Report
- Heae Surng Park, Sun Och Yoon, Beom Jin Lim, Joo Hee Kim, Soon Won Hong
- Korean J Pathol. 2014;48(5):405-408. Published online October 27, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.5.405
- 8,487 View
- 63 Download
- Usefulness of Nuclear Protein in Testis (NUT) Immunohistochemistry in the Cytodiagnosis of NUT Midline Carcinoma: A Brief Case Report
- Heae Surng Park, Yoon Sung Bae, Sun Och Yoon, Beom Jin Lim, Hyun Jun Hong, Jae Y Ro, Soon Won Hong
- Korean J Pathol. 2014;48(4):335-338. Published online August 26, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.4.335
- 11,936 View
- 96 Download
- 17 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Exploring cytologic features and potential diagnostic challenges of metastatic NUT carcinoma to the parotid gland: A case report and a comprehensive literature review
Crystal Y. Li, Salih Salihoglu, Francisco J. Civantos, Jaylou M. Velez Torres
Diagnostic Cytopathology.2024;[Epub] CrossRef - NUT carcinoma of the submandibular gland: A case report
Simone Rota, Pasquale Quattrone, Giovanni Centonze, Gianpaolo Dagrada, Arianna Ottini, Elena Colombo, Imperia Nuzzolese, Giuseppina Calareso, Marzia Franceschini, Nicola Alessandro Iacovelli, Federica Perrone, Elena Tamborini, Stefano Cavalieri
Cancer Reports.2023;[Epub] CrossRef - NUT carcinoma of the parotid gland: report of two cases, one with a rare ZNF532-NUTM1 fusion
Min Chen, Sha Zhao, Zuoyu Liang, Weiya Wang, Ping Zhou, Lili Jiang
Virchows Archiv.2022; 480(4): 887. CrossRef - NUT Carcinoma: Clinicopathologic Features, Molecular Genetics and Epigenetics
Vanessa Moreno, Karan Saluja, Sergio Pina-Oviedo
Frontiers in Oncology.2022;[Epub] CrossRef - Salivary Gland NUT Carcinoma with Prolonged Survival in Children: Case Illustration and Systematic Review of Literature
Huiying Wang, Vivian L. Weiss, Robert D. Hoffman, Ty Abel, Richard H. Ho, Scott C. Borinstein, Kyle Mannion, Julia A. Bridge, Jennifer Black, Jiancong Liang
Head and Neck Pathology.2021; 15(1): 236. CrossRef - NUT Carcinoma of the Submandibular Gland: A Case at This Uncommon Site with Review of the Literature
Vanessa Moreno, Christopher A. French, Tianhua Guo, Hui Zhu, Songling Zhang, Darryl Duncan, Ron J. Karni, Angel I. Blanco, Syed H. Jafri, Karan Saluja
Head and Neck Pathology.2021; 16(3): 881. CrossRef - Prevalence of NUT carcinoma in head and neck: Analysis of 362 cases with literature review
Taebum Lee, Junhun Cho, Chung‐Hwan Baek, Young‐Ik Son, Han‐Sin Jeong, Man Ki Chung, Sang Duk Hong, Yong Chan Ahn, Dong Ryul Oh, Jae Myoung Noh, Keunchil Park, Myung‐Ju Ahn, Hyung‐Jin Kim, Yi Kyung Kim, Young Hyeh Ko
Head & Neck.2020; 42(5): 924. CrossRef - HDAC Overexpression in a NUT Midline Carcinoma of the Parotid Gland with Exceptional Survival: A Case Report
Gonçalo Esteves, Joana Ferreira, Rita Afonso, Carmo Martins, Carlos Zagalo, Ana Félix
Head and Neck Pathology.2020; 14(4): 1117. CrossRef - Lung nuclear protein in testis carcinoma in an elderly Korean woman: A case report with cytohistological analysis
Hwa Jin Cho, Hyun‐Kyung Lee
Thoracic Cancer.2020; 11(6): 1724. CrossRef - Clinicopathological and Preclinical Findings of NUT Carcinoma: A Multicenter Study
Minsun Jung, Soyeon Kim, June-Koo Lee, Sun Och Yoon, Heae Surng Park, Soon Won Hong, Weon-Seo Park, Ji Eun Kim, Joon Kim, Bhumsuk Keam, Hyun Jik Kim, Hyoung Jin Kang, Dong-Wan Kim, Kyeong Cheon Jung, Young Tae Kim, Dae Seog Heo, Tae Min Kim, Yoon Kyung Je
The Oncologist.2019; 24(8): e740. CrossRef - NUT Carcinoma of the Salivary Glands
Abbas Agaimy, Isabel Fonseca, Carmo Martins, Khin Thway, Ryan Barrette, Kevin J. Harrington, Arndt Hartmann, Christopher A. French, Cyril Fisher
American Journal of Surgical Pathology.2018; 42(7): 877. CrossRef - Abrupt Dyskeratotic and Squamoid Cells in Poorly Differentiated Carcinoma: Case Study of Two Thoracic NUT Midline Carcinomas with Cytohistologic Correlation
Taebum Lee, Sangjoon Choi, Joungho Han, Yoon-La Choi, Kyungjong Lee
Journal of Pathology and Translational Medicine.2018; 52(5): 349. CrossRef - A Case of Nuclear Protein in Testis Midline Carcinoma Arising From the Submandibular Gland Duct in a Pregnant Patient
Younghoon Cho, Bhum Suk Keam, Kyeong Cheon Jung, Bo Hae Kim
Journal of Oral and Maxillofacial Surgery.2017; 75(9): 2020. CrossRef - Pediatric NUT-midline carcinoma: Therapeutic success employing a sarcoma based multimodal approach
Simone Storck, Alyssa L. Kennedy, Karen J. Marcus, Lisa Teot, Jennifer Vaughn, Astrid K. Gnekow, Bruno Märkl, Ivo Leuschner, Steven G. DuBois, Christopher A. French, Michael C. Frühwald
Pediatric Hematology and Oncology.2017; 34(4): 231. CrossRef - Two Cases of Nuclear Protein in Testis Midline Carcinomas of Sinonasal Tract
Minhyung Lee, Yong Seok Kang, Tae-Bin Won, Hyun Jik Kim
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2017; 60(12): 673. CrossRef - Cytological features of NUT midline carcinoma arising in sino‐nasal tract and parotid gland: Report of two new cases and review of the literature
Jerzy Klijanienko, Christophe Le Tourneau, José Rodriguez, Martial Caly, Stamatios Theocharis
Diagnostic Cytopathology.2016; 44(9): 753. CrossRef - Cytological Features of a Variant NUT Midline Carcinoma of the Lung Harboring theNSD3-NUTFusion Gene: A Case Report and Literature Review
Shiho Kuroda, Shioto Suzuki, Akira Kurita, Mari Muraki, Yoichiro Aoshima, Fumihiko Tanioka, Haruhiko Sugimura
Case Reports in Pathology.2015; 2015: 1. CrossRef
- Exploring cytologic features and potential diagnostic challenges of metastatic NUT carcinoma to the parotid gland: A case report and a comprehensive literature review
- Incidence and Malignancy Rates of Diagnoses in the Bethesda System for Reporting Thyroid Aspiration Cytology: An Institutional Experience
- Ji Hye Park, Sun Och Yoon, Eun Ju Son, Hye Min Kim, Ji Hae Nahm, SoonWon Hong
- Korean J Pathol. 2014;48(2):133-139. Published online April 28, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.2.133
- 14,423 View
- 91 Download
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The Bethesda System for Reporting Thyroid Cytopathology (BSRTC) uses six diagnostic categories to standardize communication of thyroid fine-needle aspiration (FNA) interpretations between clinicians and cytopathologists. Since several studies have questioned the diagnostic accuracy of this system, we examined its accuracy in our hospital.
Methods We calculated the incidences and malignancy rates of each diagnostic category in the BSRTC for 1,730 FNAs that were interpreted by four cytopathologists in Gangnam Severance Hospital between October 1, 2011, and December 31, 2011.
Results The diagnostic incidences of categories I-VI were as follows: 13.3%, 40.6%, 9.1%, 0.4%, 19.3%, and 17.3%, respectively. Similarly, the malignancy rates of these categories were as follows: 35.3%, 5.6%, 69.0%, 50.0%, 98.7%, and 98.9%, respectively. In categories II, V, and VI, there were no statistically significant differences in the ranges of the malignancy rates among the four cytopathologists. However, there were significant differences in the ranges for categories I and III.
Conclusions Our findings suggest that institutions that use the BSRTC should regularly update their diagnostic criteria. We also propose that institutions issue an annual report of incidences and malignancy rates to help other clinicians improve the case management of patients with thyroid nodules.
-
Citations
Citations to this article as recorded by- Assessment of an innovative synthetic matrix for enhanced cell preservation: evaluating its clinical utility and impact on diagnostic precision in thyroid fine-needle aspiration cytology
Diana-Raluca Streinu, Octavian Constantin Neagoe, Andreea Bena, Dana-Liana Stoian
BMC Endocrine Disorders.2026;[Epub] CrossRef - The Malignancy Rates of the Bethesda System for Reporting Thyroid Cytopathology: A 10-year Experience in a Single Asian Institute
Sarah I Liew, Nor S Ahmad, Navarasi R Gopal
World Journal of Endocrine Surgery.2025; 16(2): 42. CrossRef - Assessment of Thyroid Fine-Needle Aspirates Using 2023 Bethesda System
Niti Sureka, Charanjeet Ahluwalia, Sana Ahuja, Neha Kawatra Madan, Meetu Agrawal, Sunil Ranga
Acta Cytologica.2025; 69(3): 280. CrossRef - A Comprehensive Approach to the Thyroid Bethesda Category III (AUS) in the Transition Zone Between 2nd Edition and 3rd Edition of The Bethesda System for Reporting Thyroid Cytopathology: Subcategorization, Nuclear Scoring, and More
Merve Bagıs, Nuray Can, Necdet Sut, Ebru Tastekin, Ezgi Genc Erdogan, Buket Yilmaz Bulbul, Yavuz Atakan Sezer, Osman Kula, Elif Mercan Demirtas, Inci Usta
Endocrine Pathology.2024; 35(1): 51. CrossRef - Evaluation of the Efficacy of Thyroid Imaging Reporting and Data Systems Classification in Risk Stratification and in the Management of Thyroid Swelling by Comparing It With Fine-Needle Aspiration Cytology and Histopathological Examination
Abhishek K Saw, Zenith H Kerketta, Khushboo Rani, Krishna Murari, Kritika Srivastava, Ajay Kumar, Sunny LNU, Anish Baxla, Nabu Kumar, Nusrat Noor
Cureus.2024;[Epub] CrossRef - A COMPARATIVE STUDY BETWEEN CONVENTIONAL METHOD AND THE BETHESDA SYSTEM FOR REPORTING THYROID CYTOPATHOLOGY
Pooja Mangal, Arti Gupta
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2023; : 67. CrossRef - Study of Fine Needle Aspiration Cytology (FNAC) of Thyroid Gland According to the Bethesda System
Keval A Patel, Garima Anandani, Bhawana S Sharma, Riddhi A Parmar
Cureus.2023;[Epub] CrossRef - Correlation of Thyroid Fine Needle Aspiration Biopsy With Histopathological Results
Cemalettin Durgun
Cureus.2023;[Epub] CrossRef - The Bethesda System for Reporting Thyroid Cytopathology: Validating at Tribhuvan University Teaching Hospital
Kunjan Acharya, Shreya Shrivastav, Prashant Triipathi, Bigyan Raj Gyawali, Bijaya Kharel, Dharma Kanta Baskota, Pallavi Sinha
International Archives of Otorhinolaryngology.2022; 26(01): e097. CrossRef - Validating the ‘CUT score’ risk stratification tool for indeterminate thyroid nodules using the Bethesda system for reporting thyroid cytopathology
Sapir Pinhas, Idit Tessler, Luba Pasherstnik Bizer, Khaled khalilia, Meir Warman, Meital Adi, Doron Halperin, Oded Cohen
European Archives of Oto-Rhino-Laryngology.2022; 279(1): 383. CrossRef - ANALYSIS OF FINE NEEDLE ASPIRATIONS OF THE THYROID: CYTOLOGICAL-HISTOPATHOLOGICAL CORRELATION AND OUTCOMES OF THE BETHESDA SYSTEM
Ayca TAN
SDÜ Tıp Fakültesi Dergisi.2022; 29(2): 213. CrossRef - Reproducibility of Cytomorphological Diagnosis and Assessment of Risk of Malignancy of Thyroid Nodules Based on the Bethesda System for Reporting Thyroid Cytopathology
Sasmita Panda, Mamita Nayak, Lucy Pattanayak, Paresh Kumar Behera, Sagarika Samantaray, Sashibhusan Dash
Journal of Microscopy and Ultrastructure.2022; 10(4): 174. CrossRef - Comparative analysis of cytomorphology of thyroid lesion on conventional cytology versus liquid-based cytology and categorize the lesions according to The Bethesda System for Reporting Thyroid Cytopathology
M Qamar Alam, Pinki Pandey, Megha Ralli, Jitendra Pratap Singh Chauhan, Roopak Aggarwal, Vineet Chaturvedi, Asttha Kapoor, Kapil Trivedi, Savita Agarwal
Journal of Cancer Research and Therapeutics.2022; 18(Suppl 2): S259. CrossRef - Thyroid cytology in Pakistan: An institutional audit of the atypia of undetermined significance/follicular lesion of undetermined significance category
Saira Fatima, Rabia Qureshi, Sumbul Imran, Romana Idrees, Zubair Ahmad, Naila Kayani, Arsalan Ahmed
Cytopathology.2021; 32(2): 205. CrossRef - Outcomes of the Bethesda system for reporting thyroid cytopathology: Real‐life experience
Galit Avior, Or Dagan, Isaac Shochat, Yulia Frenkel, Idit Tessler, Alona Meir, Anat Jaffe, Oded Cohen
Clinical Endocrinology.2021; 94(3): 521. CrossRef - National differences in cost analysis of Afirma Genomic sequencing classifier
Ohad Ronen, Maya Oichman
Clinical Endocrinology.2021; 94(4): 717. CrossRef - Thyroid malignancy rates according to the Bethesda reporting system in Israel - A multicenter study
Ory Madgar, Galit Avior, Isaac Shochat, Ben-Zion Joshua, Lior Baraf, Yuval Avidor, Avi khafif, Niddal Assadi, Eran E. Alon
European Journal of Surgical Oncology.2021; 47(6): 1370. CrossRef - Application of the Bethesda system for reporting thyroid cytopathology for classification of thyroid nodules: A clinical and cytopathological characteristics in Bhutanese population
Sonam Choden, Chimi Wangmo, Sushna Maharjan
Diagnostic Cytopathology.2021; 49(11): 1179. CrossRef - Malignancy rates in thyroid nodules classified as Bethesda categories III and IV; a subcontinent perspective
Adnan Zahid, Waqas Shafiq, Khawaja Shehryar Nasir, Asif Loya, Syed Abbas Raza, Sara Sohail, Umal Azmat
Journal of Clinical & Translational Endocrinology.2021; 23: 100250. CrossRef - The combination of ACR‐Thyroid Imaging Reporting and Data system and The Bethesda System for Reporting Thyroid Cytopathology in the evaluation of thyroid nodules—An institutional experience
Shanmugasundaram Sakthisankari, Sreenivasan Vidhyalakshmi, Sivanandam Shanthakumari, Balalakshmoji Devanand, Udayasankar Nagul
Cytopathology.2021; 32(4): 472. CrossRef - Ultrasound-guided fine needle aspiration cytology and ultrasound examination of thyroid nodules in the UAE: A comparison
Suhail Al-Salam, Charu Sharma, Maysam T. Abu Sa’a, Bachar Afandi, Khaled M. Aldahmani, Alia Al Dhaheri, Hayat Yahya, Duha Al Naqbi, Esraa Al Zuraiqi, Baraa Kamal Mohamed, Shamsa Ahmed Almansoori, Meera Al Zaabi, Aysha Al Derei, Amal Al Shamsi, Juma Al Kaa
PLOS ONE.2021; 16(4): e0247807. CrossRef - Incidence, Clinical Characteristics, and Histopathological Results of Atypia of Undermined Significance in a Tertiary Center in UAE
Maha Osman Shangab, Azza Abdulaziz Khalifa, Fatheya Al Awadi, Mouza Alsharhan, Alaaeldin Bashier
Dubai Diabetes and Endocrinology Journal.2021; 27(1): 1. CrossRef - McGill Thyroid Nodule Score in Differentiating Thyroid Nodules in Total Thyroidectomy Cases of Indeterminate Nodules
Hadi A Al-Hakami, Reem Al-Mohammadi, Rami Al-Mutairi, Haya Al-Subaie, Mohammed A Al Garni
Indian Journal of Surgical Oncology.2020; 11(2): 268. CrossRef - The Bethesda System for Reporting Thyroid Cytopathology: A Cytohistological Study
Bakiarathana Anand, Anita Ramdas, Marie Moses Ambroise, Nirmal P. Kumar
Journal of Thyroid Research.2020; 2020: 1. CrossRef - Differences in cytopathologist thyroid nodule malignancy rate
Ohad Ronen, Hector Cohen, Eyal Sela, Mor Abu
Cytopathology.2020; 31(4): 315. CrossRef - Thyroid Multimodal Ultrasound Evaluation—Impact on Presurgical Diagnosis of Intermediate Cytology Cases
Andreea Borlea, Dana Stoian, Laura Cotoi, Ioan Sporea, Fulger Lazar, Ioana Mozos
Applied Sciences.2020; 10(10): 3439. CrossRef - Fine-needle aspiration cytology of nodular thyroid lesions: A 1-year experience of the thyroid cytopathology in a large regional and a University Hospital, with histological correlation
Kaumudi Konkay, Radhika Kottu, Mutheeswaraiah Yootla, Narendra Hulikal
Thyroid Research and Practice.2019; 16(2): 60. CrossRef - Review of a single institution's fine needle aspiration results for thyroid nodules: Initial observations and lessons for the future
Ohad Ronen, Hector Cohen, Mor Abu
Cytopathology.2019; 30(5): 468. CrossRef - Strain Elastography as a Valuable Diagnosis Tool in Intermediate Cytology (Bethesda III) Thyroid Nodules
Dana Stoian, Florin Borcan, Izabella Petre, Ioana Mozos, Flore Varcus, Viviana Ivan, Andreea Cioca, Adrian Apostol, Cristina Adriana Dehelean
Diagnostics.2019; 9(3): 119. CrossRef - Improvement of diagnostic performance of pathologists by reducing the number of pathologists responsible for thyroid fine needle aspiration cytology: An institutional experience
Jae Yeon Seok, Jungsuk An, Hyun Yee Cho
Diagnostic Cytopathology.2018; 46(7): 561. CrossRef - Bethesda Classification and Cytohistological Correlation of Thyroid Nodules in a Brazilian Thyroid Disease Center
Kassia B. Reuters, Maria C.O.C. Mamone, Elsa S. Ikejiri, Cleber P. Camacho, Claudia C.D. Nakabashi, Carolina C.P.S. Janovsky, Ji H. Yang, Danielle M. Andreoni, Rosalia Padovani, Rui M.B. Maciel, Felipe A.B. Vanderlei, Rosa P.M. Biscolla
European Thyroid Journal.2018; 7(3): 133. CrossRef - The impact of rapid on‐site evaluation on thyroid fine‐needle aspiration biopsy: A 2‐year cancer center institutional experience
Ricardo G. Pastorello, Camila Destefani, Pedro H. Pinto, Caroline H. Credidio, Rafael X. Reis, Thiago de A. Rodrigues, Maryane C. de Toledo, Louise De Brot, Felipe de A. Costa, Antonio G. do Nascimento, Clóvis A. L. Pinto, Mauro A. Saieg
Cancer Cytopathology.2018; 126(10): 846. CrossRef - The Use of the Bethesda System for Reporting Thyroid Cytopathology in Korea: A Nationwide Multicenter Survey by the Korean Society of Endocrine Pathologists
Mimi Kim, Hyo Jin Park, Hye Sook Min, Hyeong Ju Kwon, Chan Kwon Jung, Seoung Wan Chae, Hyun Ju Yoo, Yoo Duk Choi, Mi Ja Lee, Jeong Ja Kwak, Dong Eun Song, Dong Hoon Kim, Hye Kyung Lee, Ji Yeon Kim, Sook Hee Hong, Jang Sihn Sohn, Hyun Seung Lee, So Yeon Pa
Journal of Pathology and Translational Medicine.2017; 51(4): 410. CrossRef - Thyroid FNA cytology in Asian practice—Active surveillance for indeterminate thyroid nodules reduces overtreatment of thyroid carcinomas
K. Kakudo, M. Higuchi, M. Hirokawa, S. Satoh, C. K. Jung, A. Bychkov
Cytopathology.2017; 28(6): 455. CrossRef - Thyroid Fine-Needle Aspiration Cytology Practice in Korea
Yoon Jin Cha, Ju Yeon Pyo, SoonWon Hong, Jae Yeon Seok, Kyung-Ju Kim, Jee-Young Han, Jeong Mo Bae, Hyeong Ju Kwon, Yeejeong Kim, Kyueng-Whan Min, Soonae Oak, Sunhee Chang
Journal of Pathology and Translational Medicine.2017; 51(6): 521. CrossRef - Bethesda System for Reporting Thyroid Cytopathology: A three-year study at a tertiary care referral center in Saudi Arabia
Mohamed Abdulaziz Al Dawish, Asirvatham Alwin Robert, Aljuboury Muna, Alkharashi Eyad, Abdullah Al Ghamdi, Khalid Al Hajeri, Mohammed A Thabet, Rim Braham
World Journal of Clinical Oncology.2017; 8(2): 151. CrossRef - A meta‐analytic review of the Bethesda System for Reporting Thyroid Cytopathology: Has the rate of malignancy in indeterminate lesions been underestimated?
Patrizia Straccia, Esther Diana Rossi, Tommaso Bizzarro, Chiara Brunelli, Federica Cianfrini, Domenico Damiani, Guido Fadda
Cancer Cytopathology.2015; 123(12): 713. CrossRef - Value of TIRADS, BSRTC and FNA-BRAFV600E mutation analysis in differentiating high-risk thyroid nodules
Yu-zhi Zhang, Ting Xu, Dai Cui, Xiao Li, Qing Yao, Hai-yan Gong, Xiao-yun Liu, Huan-huan Chen, Lin Jiang, Xin-hua Ye, Zhi-hong Zhang, Mei-ping Shen, Yu Duan, Tao Yang, Xiao-hong Wu
Scientific Reports.2015;[Epub] CrossRef - A study of malignancy rates in different diagnostic categories of the Bethesda system for reporting thyroid cytopathology: An institutional experience
P. Arul, C. Akshatha, Suresh Masilamani
Biomedical Journal.2015; 38(6): 517. CrossRef - Diagnostic accuracy of Bethesda system for reporting thyroid cytopathology: an institutional perspective
Samreen Naz, Atif Hashmi, Amna khurshid, Naveen Faridi, Muhammad Edhi, Anwar Kamal, Mehmood Khan
International Archives of Medicine.2014; 7(1): 46. CrossRef
- Assessment of an innovative synthetic matrix for enhanced cell preservation: evaluating its clinical utility and impact on diagnostic precision in thyroid fine-needle aspiration cytology
- Cytologic Features of Giant Cell Ependymoma: A Case Report and Review of the Literature
- Myoung Ju Koh, Sun Och Yoon, Hyae Min Jeon, Hyeon Joo Jeong, Soon Won Hong, Se Hoon Kim
- Korean J Pathol. 2012;46(5):507-513. Published online October 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.5.507
- 10,496 View
- 71 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Here, we present a case of anaplastic giant cell ependymoma (GCE) occurring in a 15-year-old woman. Squash smear slides for intraoperative frozen section diagnosis revealed oval to round cell clusters with a papillary structure in a fibrillary background. This was occasionally accompanied by the presence of bizarre pleomorphic giant cells with hyperchromatic nuclei and prominent intranuclear inclusions. These intranuclear inclusions were a key clue to diagnosis of ependymoma. Histologic analysis revealed features of a high-grade tumor with perivascular pseudorosettes and bizarre pleomorphic giant cells, which established the diagnosis of GCE. We performed a review of literatures about the cytologic features of GCE, including our case, thus proposing that intraoperative frozen diagnosis of GCE would be established by squash smear preparations featuring the mitosis and necrosis, as well as the high cellularity, and the presence of giant cells showing hyperchromatic nuclei with eosinophilic cytoplasm and intranuclear inclusions/pseudoinclusions.
-
Citations
Citations to this article as recorded by- A case of myxopapillary ependymoma with predominant giant cell morphology: A rare entity with comprehensive genomic profiling and review of literature
Bryan Morales‐Vargas, Hassan Saad, Daniel Refai, Matthew Schniederjan, Zied Abdullaev, Kenneth Aldape, Malak Abedalthagafi
Neuropathology.2025; 45(1): 13. CrossRef - Report of a case of giant cell ependymoma with unusual clinical and pathological presentation
Mónica B. Mezmezian, Victor Del Caño, Liliana G. Olvi
Neuropathology.2019; 39(4): 313. CrossRef - Giant Cell Ependymoma of Cervicomedullary Junction: A Case Report of a Long-Term Survivor and Literature Review
Martina Cappelletti, Andrea G. Ruggeri, Giorgia Iacopino, Roberto Delfini
World Neurosurgery.2018; 116: 121. CrossRef - Immunohistochemical features of giant cell ependymoma of the filum terminale with unusual clinical and radiological presentation
Fernando Candanedo-Gonzalez, Cindy Sharon Ortiz-Arce, Samuel Rosales-Perez, Ana Lilia Remirez-Castellanos, Candelaria Cordova-Uscanga, Armando Gamboa-Dominguez
Diagnostic Pathology.2017;[Epub] CrossRef - Giant Cell Ependymoma of Lateral Ventricle: Case Report, Literature Review, and Analysis of Prognostic Factors and Genetic Profile
Hirokazu Takami, Christopher S. Graffeo, Avital Perry, Aditya Raghunathan, Robert B. Jenkins, Caterina Giannini, Terry C. Burns
World Neurosurgery.2017; 108: 997.e9. CrossRef
- A case of myxopapillary ependymoma with predominant giant cell morphology: A rare entity with comprehensive genomic profiling and review of literature
- Detection of SV40 Large T Antigen in Malignant Lymphomas.
- Young A Kim, MeeSoo Chang, Jinho Paik, Sun Och Yoon, Yoon Kyung Jeon, Chul Woo Kim, Ji Eun Kim
- Korean J Pathol. 2009;43(4):312-316.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.312
- 5,009 View
- 70 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The association of simian virus 40 (SV40) with certain types of human cancers, including malignant lymphomas, has been a topic of interest for some time. Although the virus is distributed worldwide, its incidences vary according to the specific types of tumors, and the epidemiological areas. The aim of this study was to investigate the frequency of SV40 in malignant lymphomas among Korean patients. METHODS: One hundred seventy three cases of malignant lymphomas were evaluated by immunohistochemical staining for SV40 large T antigen (TAg), using an extremely sensitive, tyramide based, catalyzed signal amplification method. RESULTS: From 158 non-Hodgkin's lymphomas, including 115 diffuse large B-cell lymphomas, and 15 Hodgkin's lymphomas, none of the cases were positive for SV40 TAg. CONCLUSIONS: SV40 does not appear to be related to the pathogenesis of malignant lymphomas among Koreans. -
Citations
Citations to this article as recorded by- No Detection of Simian Virus 40 in Malignant Mesothelioma in Korea
Minseob Eom, Jamshid Abdul-Ghafar, Sun-Mi Park, Joung Ho Han, Soon Won Hong, Kun Young Kwon, Eun Suk Ko, Lucia Kim, Wan Seop Kim, Seung Yeon Ha, Kyo Young Lee, Chang Hun Lee, Hye Kyoung Yoon, Yoo Duk Choi, Myoung Ja Chung, Soon-Hee Jung
Korean Journal of Pathology.2013; 47(2): 124. CrossRef
- No Detection of Simian Virus 40 in Malignant Mesothelioma in Korea
- Epstein-Barr virus-associated Inflammatory Pseudotumor-like Follicular Dendritic Cell Tumor in the Spleen of a Patient with Diffuse Large B Cell Lymphoma: A Case Report and Review of the Literature.
- Sun Och Yoon, Hyoungsuk Ko, Baek hui Kim, Ghee Young Kwon, Yoon Kyung Jeon, Chul Woo Kim
- Korean J Pathol. 2007;41(3):198-202.
- 2,497 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF - We report a case of an Epstein-Barr virus (EBV)-associated inflammatory pseudotumor-like follicular dendritic cell tumor (IPT-like FDC tumor). The tumor occurred in the spleen of a 64-year-old woman with a history of a diffuse large B-cell lymphoma (DLBCL) of neck nodes that presented four years ago. The splenectomy specimen revealed a 5 cm-sized, tan-colored and well-circumscribed mass. Histologically, spindle or ovoid cells with large vesicular nuclei were admixed with abundant inflammatory cells. Immunohistochemically, spindle cells were positive for FDC marker CD35, but negative for CD20, CD30 and ALK. EBV was detected almost exclusively in spindle cells by EBER in situ hybridization. IPT-like FDC tumors are rare, and are recognized as a distinctive clinicopathologic variant of FDC tumors. Among only 18 similar cases reported in the English language literature, the present case is the first case of a patient with a history of DLBCL.
- Twist Expression in Upper Urinary Tract Urothelial Carcinoma Affects Patients Disease Free Survival and is Associated with Tumor Grade.
- Dong Il Kim, Sun Och Yoon, Seog Yun Park, Bomi Kim, Gyeong Hoon Kang, Kyung Chul Moon
- Korean J Pathol. 2007;41(5):324-328.
- 2,120 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Epithelial-mesenchymal transition (EMT) is critical for morphogenesis during embryonic development and is also implicated in the conversion of early-stage tumors into invasive malignancies. Recently, Twist has been identified to play an important role in EMTmediated metastatic progression of several types of human cancer. The present study examined the expression of Twist and evaluated its clinicopathologic significance in urothelial carcinoma of upper urinary tract.
METHODS
Immunohistochemical staining for Twist expression was performed on 70 upper urinary tract urothelial carcinomas (UUT-UCs) using tissue microarray.
RESULTS
Immunohistochemical staining for Twist was positive in 31/70 cases (44.3%) of UUT-UCs. Twist expression was associated with high-grade and advanced-stage (ISUP grade, p<0.01; stage, p=0.045). The patients with Twist positive-tumors revealed lower disease free survival rate than those with Twist negative-tumors (p<0.01). The overall survival for patients with Twist positive-tumors was slightly worse than the patients with Twist negative- tumors, but the difference was not statistically significant (p=0.12).
CONCLUSION
Our results suggest that Twist is a novel marker for advanced UUT-UC.
- Adrenocortical Carcinoma, Myxoid Variant: A Case Report.
- Bomi Kim, Sun Och Yoon, Dong Il Kim, Myung Cherl Kook, Eun Kyung Hong
- Korean J Pathol. 2007;41(6):430-435.
- 2,134 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - Myxoid variant of adrenal cortical carcinoma is extremely rare and there have been only 16 such cases reported in the medical literature. Here we report on a case of 43-year-old woman with a left adrenal mass that was detected during the evaluation for Cushing's syndrome. Left adrenalectomy was performed and the tumor weighed 347 g. The cut surface was predominantly myxoid and gelatinous with central hemorrhage and necrosis. Histologically, the tumor cells were rather small, uniform and polygonal with mild pleomorphism. It showed diverse morphologic patterns according to the amount of the myxoid stromal component. Making the diagnosis was not easy because the tumor was without areas of conventional adrenocortical carcinoma. Immunohistochemically, the tumor cells were positive for alpha-inhibin, synaptophysin and vimentin, but the tumor cells were negative for pan-cytokeratin and CAM 5.2. The immunophenotypes were identical to those of conventional adrenal cortical neoplasms. During the evaluation of a cytokeratin-negative and vimentin-positive retroperitoneal neoplasm with a myxoid component, the possibility of adrenal cortical tumor should be considered in spite that this is a very rare entity.
- Diffuse Large B Cell Lymphoma Shows Distinct Methylation Profiles of the Tumor Suppressor Genes among the Non-Hodgkin's Lymphomas.
- Sun Och Yoon, Young A Kim, Yoon Kyung Jeon, Ji Eun Kim, Gyeong Hoon Kang, Chul Woo Kim
- Korean J Pathol. 2008;42(1):16-20.
- 2,379 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Aberrant methylation of CpG islands in promoter regions is one of the major mechanisms for silencing of tumor suppressor genes in various types of human cancers including non-Hodgkin's lymphomas (NHL). In this study, we investigated the aberrant promoter methylation status of known or suspected tumor suppressor genes in NHLs and compared the methylation profiles between B-cell and T/NK-cell NHLs.
METHODS
54 cases of B-cell NHLs and 16 cases of T/NK-cell NHLs were examined for the methylation status of eight genes using methylation specific PCR.
RESULTS
CpG islands methylation was variously found in eight genes as follows; DAPK (71%), MT1G (70%), p16 (53%), CDH1 (53%), THBS1 (56%), MGMT (27.1%), COX2 (13%), and RUNX3 (11.4%). In six cases (8 %), methylation was not observed in any of these genes. Overall methylation index of B-cell NHLs (0.48) was significantly higher than that of T/NK-cell NHLs (0.32). Of eight genes tested, THBS1 and CDH1 methylations were much more prominent in diffuse large B-cell lymphomas than in T/NK-cell NHLs or other B-cell NHLs.
CONCLUSION
This study suggests that aberrant CpG island methylation is a frequent event in NHLs, and diffuse large B-cell lymphomas show overlapping but distinct methylation profiles.

 E-submission
E-submission
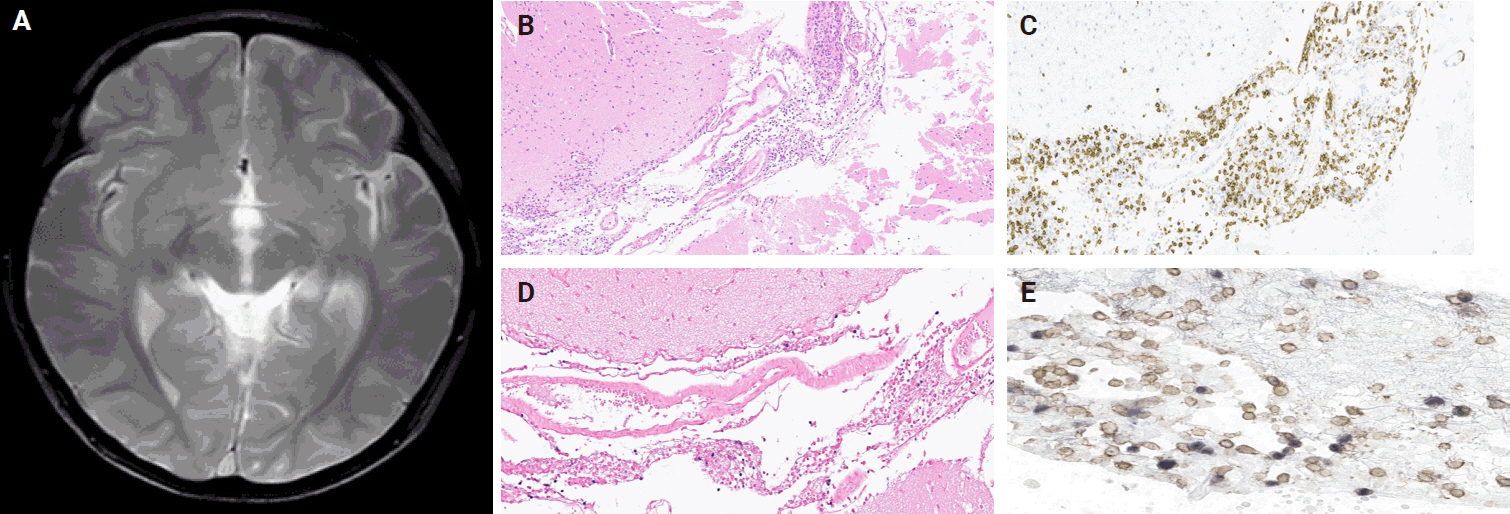



 First
First Prev
Prev



