Search
- Page Path
- HOME > Search
Case Study
- Inconspicuous longitudinal tears of the intracranial vertebral artery in traumatic basal subarachnoid hemorrhage
- Seongho Kim
- J Pathol Transl Med. 2020;54(2):179-183. Published online November 8, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.15
- 10,438 View
- 208 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
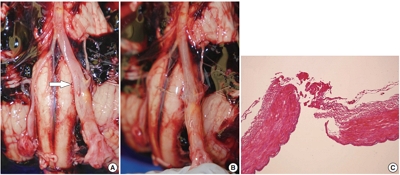
PDF - Blunt force trauma to the head or neck region can cause traumatic basal subarachnoid hemorrhage (TBSAH), which can result in rapid loss of consciousness and death; however, detecting such a vascular injury is difficult. Posterior neck dissection was performed to investigate the bleeding focus in TBSAH cases 2018 and 2019. In all four cases, autopsies revealed a longitudinal tear in the midsection of the vertebral artery’s intracranial portion. The midportion of the intracranial vertebral artery appears to be most vulnerable to TBSAH. Interestingly, three of the cases showed only a vaguely visible longitudinal fissure in the artery without a grossly apparent tear; rupture was confirmed by microscopic examination. Longitudinal fissures of the intracranial vertebral artery, which are difficult to identify without detailed examination, may be overlooked in some cases of TBSAH. Thus, careful gross and microscopic examination of the vertebral artery is recommended in cases of TBSAH.
-
Citations
Citations to this article as recorded by- Traumatic vertebrobasilar pseudoaneurysms: diagnostic pitfalls on CT angiography with forensic implications — two case reports
Numfon Tweeatsani, Kana Unuma, Yukiko Uemura, Hirotaro Iwase, Yohsuke Makino
Emergency Radiology.2025; 33(1): 189. CrossRef - Effect of Ginseng Extract Ginsenoside Rg1 on Mice with Intracerebral Injury
Zixin Zhuang, Jinman Chen, Hao Xu, Yongjun Wang, Qianqian Liang
Chinese Medicine and Culture.2023;[Epub] CrossRef
- Traumatic vertebrobasilar pseudoaneurysms: diagnostic pitfalls on CT angiography with forensic implications — two case reports
Case Reports
- Iris Cyst: A case report.
- Sang Yong Song, Je G Chi, Jin Hak Lee
- Korean J Pathol. 1993;27(4):427-429.
- 2,488 View
- 32 Download
-
 Abstract
Abstract
 PDF
PDF - Cysts of the iris may be primary lesions of either epithelial or stromal in origin, or secondary lesions after trauma or surgery. The stromal cyst is usually of primary lesion, although it could be secondary as shown in our case. We report a case of recurrent iris cyst after trauma. The patient was an 8-year-old girl. She had a penetrating injury of the involved eye three years ago. She had a similar iris cyst removed two years before this surgery. Histologically, the cyst was lined by non-keratinizing stratified squamous epithelia and subjacent fibrovascular tissue. Islands of melanin-containing epithelial cells and acellular basophilic degenerating materials were also seen in the lesion. This case represents a stromal epithelial cyst that by history appears to be of post-traumatic etiology.
- Traumatic Neuroma in the Pancreas Head Following Excision of Pseudocyst: A Brief Case Report.
- Jeong Won Kim, Gawon Choi, Jeong Eun Hwang, Shin Kwang Kang, Duck Jong Han, Se J Jang
- Korean J Pathol. 2006;40(5):385-388.
- 2,338 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - We describe here a case of traumatic neuroma that developed in the pancreas head as a rare complication of pancreatic surgery for pseudocyst. A 50-year-old man presented with septic shock. The patient was a heavy drinker with history of operation for pancreatic pseudocyst 28 years ago. On the radiologic examinations, a poorly defined mass-like lesion was found in the uncinate process of pancreas, and it had features of chronic pancreatitis and a stricture of the distal common bile duct. Whipple's operation was performed due to the diagnosis of suspected pancreas head cancer. The pancreas revealed an ill-demarcated 4 cm sized firm mass with grayish white fibrotic cut surface in the head portion. On the microscopic examination, the mass was composed of haphazard proliferations of nerve fascicles in a fibrocollagenous matrix and this case was diagnosed as traumatic neuroma. Although traumatic neruoma is a rare cause of a pancreatic mass, it should be included as a differential diagnosis of pancreatic mass in patients with a history of pancreatic surgery.

 E-submission
E-submission

 First
First Prev
Prev



