Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(4); 2012 > Article
-
Case Report
Multifocal Adenocarcinomas Arising within a Gastric Inverted Hyperplastic Polyp - Hyun-Soo Kim, Eun-Jung Hwang1, Jae-Young Jang1, Juhie Lee2, Youn Wha Kim2
-
Korean Journal of Pathology 2012;46(4):387-391.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.4.387
Published online: August 23, 2012
Aerospace Medical Research Center, Aerospace Medical Center, Republic of Korea Air Force, Cheongwon, Korea.
1Department of Internal Medicine, Kyung Hee University School of Medicine, Seoul, Korea.
2Department of Pathology, Kyung Hee University School of Medicine, Seoul, Korea.
- Corresponding Author: Youn Wha Kim, M.D. Department of Pathology, Kyung Hee University School of Medicine, 26 Kyunghee-daero, Dongdaemun-gu, Seoul 130-701, Korea. Tel: +82-2-958-8743, Fax: +82-2-958-8730, kimyw@khu.ac.kr
• Received: May 18, 2011 • Accepted: July 26, 2011
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- We present herein the occurrence of multifocal adenocarcinomas with a minute signet ring cell carcinoma that arose within a gastric inverted hyperplastic polyp (IHP) in a 40-year-old woman. Endoscopic ultrasonography demonstrated a heterogeneous hypoechoic mass in the third layer of the gastric wall. The endoscopic submucosal dissection specimen measuring 3.5×3.2×1.8 cm was a well-circumscribed protruding lesion that had a slit-shaped cavity. Histologically, the lesion consisted mainly of endophytic proliferation of hyperplastic columnar cells resembling normal foveolar epithelium. In addition, six foci of adenocarcinomas and a minute focus of signet ring cell carcinoma were randomly distributed in the superficial and deep regions. The adenocarcinoma was gradually transitioning from dysplasia, while the signet ring cell carcinoma was surrounded by hyperplastic foveolar epithelium. This is the first report of a gastric IHP with multifocal intramucosal adenocarcinomas and a signet ring cell carcinoma, and endoscopic submucosal dissection is used to completely resect it.
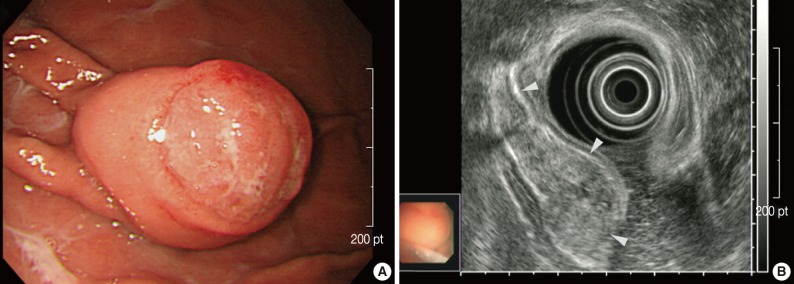
- A 40-year-old woman presented with a one-month history of preprandial epigastric pain. Her medical history included uterine leiomyoma. Physical examination and laboratory data produced no abnormal findings. Endoscopic examination revealed a subepithelial mass in the gastric body that was covered with normal mucosa and showed round superficial nodular changes at the surface. Bridging of surrounding folds was evident (Fig. 1A). Endoscopic ultrasonography demonstrated a heterogeneous hypoechoic tumor in the third layer of the gastric wall (Fig. 1B). With the expectation of a gastric submucosal tumor, endoscopic submucosal dissection was performed to resect the mass completely.
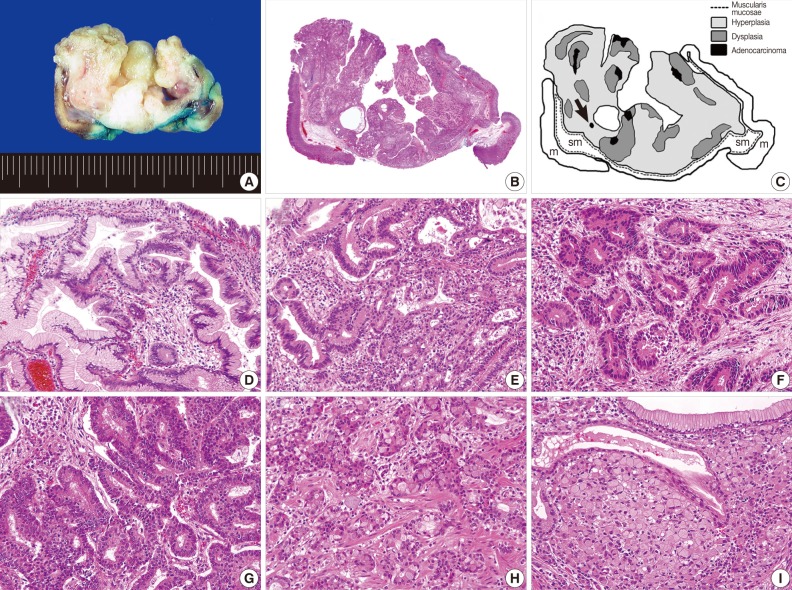
- Grossly, the resected specimen measuring 3.5×3.2×1.8 cm was a well-circumscribed protruding lesion with a slit-shaped cavity in the center (Fig. 2A). Histologically, the lesion consisted mainly of endophytic proliferation of hyperplastic columnar cells that resembled normal foveolar epithelium and were connected with inflamed surface epithelium. Also seen were six foci of adenocarcinomas, which were randomly distributed in the superficial and deep portions of the lesion (Fig. 2B, C). Transitions from hyperplasia to dysplasia (Fig. 2D) and from dysplasia to adenocarcinoma (Fig. 2E) were identified. The cancerous foci displayed distinct morphologic features, including well-formed tubular structures infiltrating the lamina propria (well-differentiated adenocarcinoma) (Fig. 2F), clusters of fused or cribriform glands lined with the tumor cells with obvious piling-up (moderately differentiated adenocarcinoma) (Fig. 2G) and indistinct glandular structures with occasional mucus production due to individual tumor cells (poorly differentiated adenocarcinoma) (Fig. 2H). We also found a minute focus of signet ring cell carcinoma that was surrounded by hyperplastic foveolar epithelium (Fig. 2I). No dysplasia was identified adjacent to the signet ring cell carcinoma. All cancerous foci were confined within the mucosa, and the resection margins were negative for dysplasia or carcinoma.
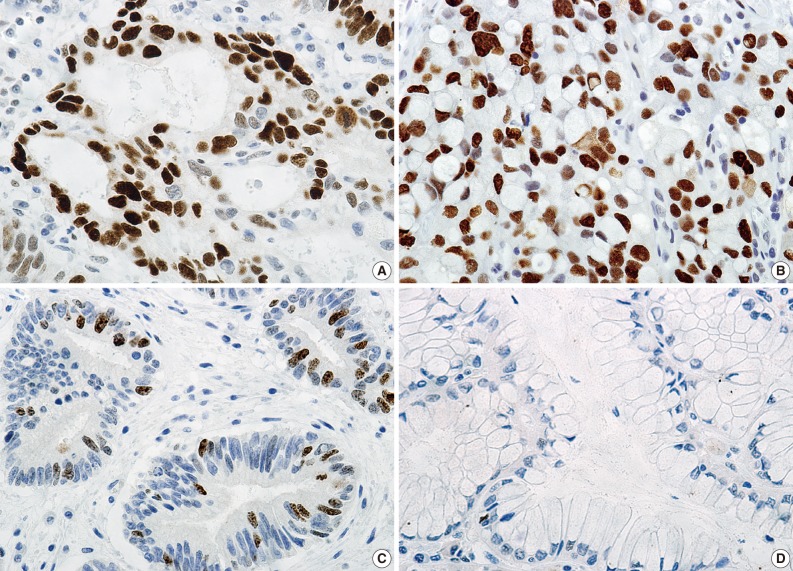
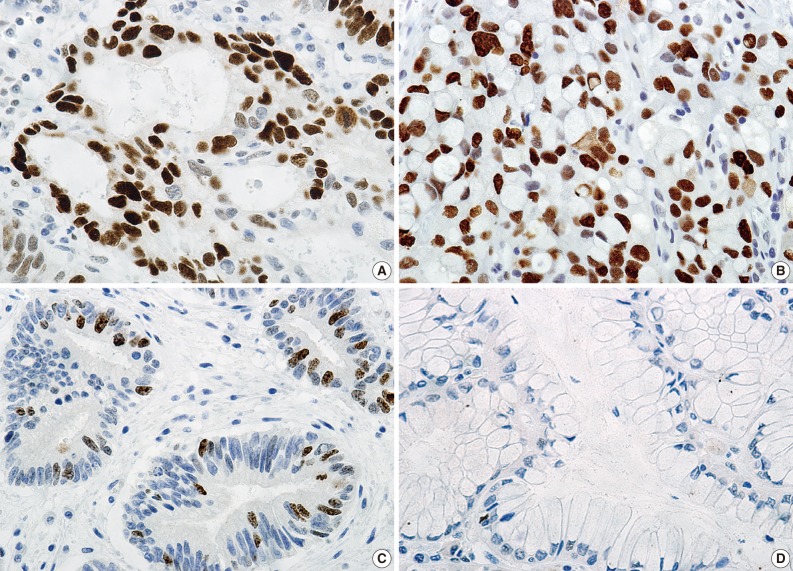
- Immunohistochemically, almost all cancer cells in the adenocarcinoma (Fig. 3A) and signet ring cell carcinoma (Fig. 3B) and approximately 10% of dysplastic cells (Fig. 3C) were positive for p53 protein (1:2,000, clone DO-7, Novacastra, Newcastle upon Dyne, UK), while hyperplastic epithelium was negative (Fig. 3D). In addition, immunoreactivity to Ki-67 protein (1:250, clone MIB-1, Dakocytomation, Glostrup, Denmark) was detected in approximately 80% of cancer cells and in almost the same percentage of dysplastic cells, while no Ki-67 immunoreactivity was observed in hyperplastic epithelium.
- The patient was discharged 3 days after endoscopic submucosal dissection without any complication. She has been followed-up as an outpatient with periodic endoscopy, and is healthy at 22 months without any sign of tumor recurrence.
CASE REPORT
- Histologically, Gastric IHP consists of marked endophytic proliferation of foveolar-, pyloric- or fundic-type glandular epithelium, leading to a polypoid lesion. The main lesion is located in the submucosa or the inside of muscularis mucosae. In 1993, Kamata et al.1 named the lesion IHP, as it resembles IHP of the colon.3 To date, 35 cases of gastric IHP, including the present case, have been described in the English-language literature. Although the pathogenesis of IHP is not understood, studies suggest that inflammation and subsequent healing may promote the epithelial displacement.4,5 In our patient, the connection between the inflamed overlying mucosa and the hyperplastic component, and the presence of the slit-shaped cavity in the center suggested that repeated mucosal inflammation caused a break in the muscularis mucosae, which permitted the downward herniation and submucosal trapping of mucosal glands.
- The occurrence of adenocarcinoma within a gastric IHP was reported for the first time by Kono et al.,2 who observed a single focus of well-differentiated adenocarcinoma emerging from adjacent dysplasia. Six cases of gastric IHP with coexisting adenocarcinoma have been reported.6,7 But in each case, the two lesions developed separately. To our knowledge, therefore, this is the second report of adenocarcinoma that arose within a gastric IHP. The presence of transitions from hyperplasia to dysplasia and from dysplasia to adenocarcinoma may indicate that the cancerous foci might progress through a dysplasia-carcinoma sequence. In the present case, p53 immunoreactivity was absent in hyperplasia, focal in dysplasia, and was diffuse and strong in the adenocarcinoma. These observations, in line with those of Kono et al.,2 suggest that p53 dysregulation may have an important role in the malignant transformation of IHP.
- Also worth noting are the poorly differentiated adenocarcinoma and signet ring cell carcinoma we observed in this IHP. Most gastric HPs that undergo malignant transformation are accompanied by well- to moderately differentiated adenocarcinomas.8,9 In fact, an association of poorly differentiated adenocarcinoma or signet ring cell carcinoma with HP is extremely unusual.10-12 To our knowledge, this is the first report of a signet ring cell carcinoma that arose within a gastric IHP. The relationship between dysplasia and signet ring cell carcinoma is unknown, and the progression from dysplasia to carcinoma as generally understood does not adequately explain how signet ring cell carcinoma might develop within an IHP. However, our observation of diffuse, strong p53 immunoreactivity in the signet ring cell carcinoma may help to clarify the pathogenesis.
- Several points may be relevant to the treatment of IHP. In view of the generally benign cellular characteristics of IHP, similar to those of HP, overtreatment should be avoided. However, given that dysplasia or even adenocarcinoma may develop within the IHP, the lesion should be resected. As we clearly demonstrated, multifocal adenocarcinomas may be present and randomly distributed in the superficial and deep regions of the gastric IHP. Despite a thorough review of endoscopic photographs, we could not precisely locate the cancerous foci. Furthermore, conventional endoscopic biopsy forceps would not be able to reach the deeply seated adenocarcinoma. In a large lesion, a negative biopsy result cannot reliably exclude the presence of dysplasia or adenocarcinoma, and hence a complete resection with a negative margin and thorough histologic examination should be performed. In the present case, the lesion was successfully resected using endoscopic submucosal dissection technique. For gastric mucosal and submucosal tumors, endoscopic resection is comparable to conventional surgery, but is less invasive and more economical.13 The endoscopic submucosal dissection technique is more reliable than the conventional endoscopic mucosal resection for en bloc resection of a lesion measuring larger than 2 cm.14 We recommend that endoscopic submucosal dissection be used to treat a gastric IHP measuring larger than 2 cm. Undoubtedly, this procedure requires endoscopists with specialized skill and experience, and follow-up with periodic endoscopy to check for recurrence.
- We have described the occurrence of multifocal intramucosal adenocarcinomas with a minute signet ring cell carcinoma that arose within a gastric IHP. Our findings reveal that because biopsy cannot exclude the presence of dysplasia or adenocarcinoma, the IHP should be completely resected and analyzed histologically with particular thoroughness.
DISCUSSION
- 1. Kamata Y, Kurotaki H, Onodera T, Nishida N. An unusual heterotopia of pyloric glands of the stomach with inverted downgrowth. Acta Pathol Jpn 1993; 43: 192-197. ArticlePubMed
- 2. Kono T, Imai Y, Ichihara T, et al. Adenocarcinoma arising in gastric inverted hyperplastic polyp: a case report and review of the literature. Pathol Res Pract 2007; 203: 53-56. ArticlePubMed
- 3. Sobin LH. Inverted hyperplastic polyps of the colon. Am J Surg Pathol 1985; 9: 265-272. ArticlePubMed
- 4. Yantiss RK, Goldman H, Odze RD. Hyperplastic polyp with epithelial misplacement (inverted hyperplastic polyp): a clinicopathologic and immunohistochemical study of 19 cases. Mod Pathol 2001; 14: 869-875. ArticlePubMedPDF
- 5. Itoh K, Tsuchigame T, Matsukawa T, Takahashi M, Honma K, Ishimaru Y. Unusual gastric polyp showing submucosal proliferation of glands: case report and literature review. J Gastroenterol 1998; 33: 720-723. ArticlePubMedPDF
- 6. Yamashita M, Hirokawa M, Nakasono M, et al. Gastric inverted hyperplastic polyp: report of four cases and relation to gastritis cystica profunda. APMIS 2002; 110: 717-723. ArticlePubMed
- 7. Choi MS, Jin SY, Kim DW, Lee DW, Park SM. A case of gastric inverted hyperplastic polyp associated with gastritis cystica profunda and early gastric carcinoma. Korean J Pathol 2007; 41: 55-58.
- 8. Shibahara K, Haraguchi Y, Sasaki I, et al. A case of gastric hyperplastic polyp with malignant transformation. Hepatogastroenterology 2005; 52: 319-321. PubMed
- 9. Yao T, Kajiwara M, Kuroiwa S, et al. Malignant transformation of gastric hyperplastic polyps: alteration of phenotypes, proliferative activity, and p53 expression. Hum Pathol 2002; 33: 1016-1022. ArticlePubMed
- 10. Hirasaki S, Suzuki S, Kanzaki H, Fujita K, Matsumura S, Matsumoto E. Minute signet ring cell carcinoma occurring in gastric hyperplastic polyp. World J Gastroenterol 2007; 13: 5779-5780. ArticlePubMedPMC
- 11. Wu CH, Chen MJ, Chang WH, Chan YJ, Wang HY, Shih SC. Signet-ring type adenocarcinoma arising from a tiny gastric polyp. Gastrointest Endosc 2008; 67: 724-725. Article
- 12. Fry LC, Lazenby AJ, Lee DH, Mönkemüller K. Signet-ring-cell adenocarcinoma arising from a hyperplastic polyp in the stomach. Gastrointest Endosc 2005; 61: 493-495. ArticlePubMed
- 13. Gotoda T. Endoscopic resection of early gastric cancer. Gastric Cancer 2007; 10: 1-11. ArticlePubMedPDF
- 14. Gotoda T. A large endoscopic resection by endoscopic submucosal dissection procedure for early gastric cancer. Clin Gastroenterol Hepatol 2005; 3(7 Suppl 1):S71-S73. ArticlePubMed
REFERENCES
Fig. 1Endoscopic findings. (A) A subepithelial mass in the gastric body shows round superficial nodular change at the surface, with bridging of surrounding folds (right upper corner). (B) Endoscopic ultrasonography shows a heterogeneous hypoechoic tumor in the third layer of the gastric wall (arrowheads).
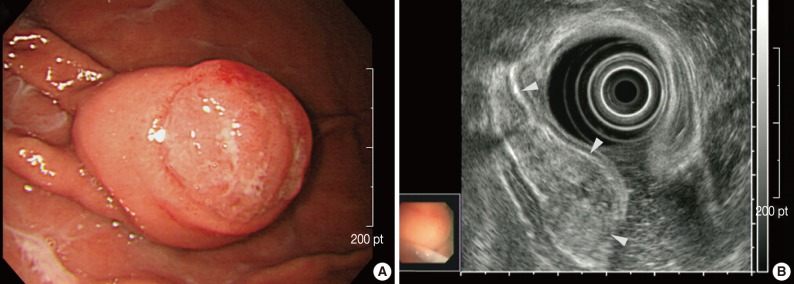
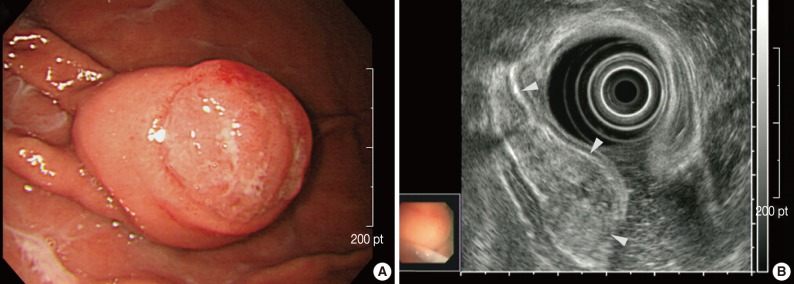
Fig. 2Gross and histologic findings. (A) The mass is a well-circumscribed downward-growing lesion with a slit-shaped cavity in the center. Scanning view (B) and schematic representation (C) of the lesion, which includes regions of hyperplasia and multifocal dysplasia and adenocarcinoma. A black arrow indicates a minute focus of signet ring cell carcinoma. m, mucosa; sm, submucosa. Transitions from hyperplasia (left half) to dysplasia (right half; D) and dysplasia (periphery) to adenocarcinoma (center; E) are apparent. Each cancerous focus displays a distinctive morphology and degree of differentiation, corresponding to well (F), moderately (G) and poorly differentiated adenocarcinoma (H). (I) In contrast with other cancerous foci, the signet ring cell carcinoma is surrounded by hyperplastic epithelium, without a transitional dysplastic component.
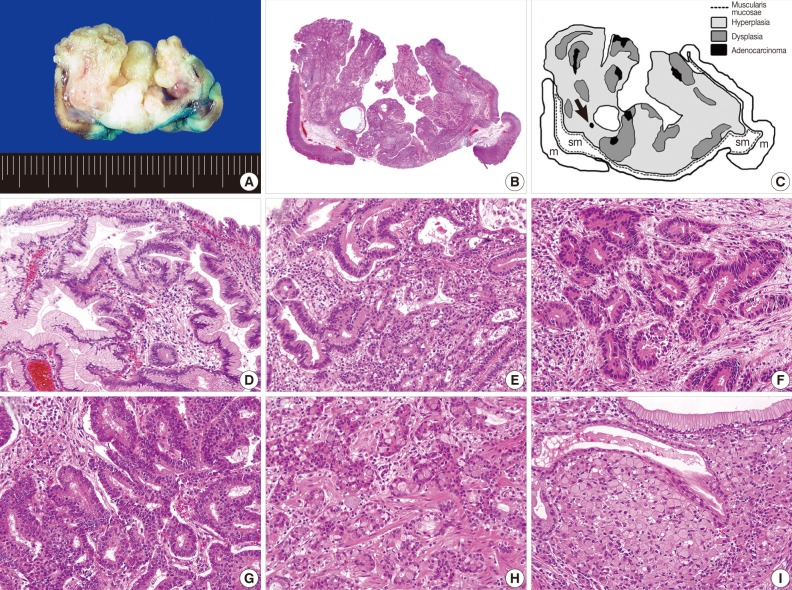
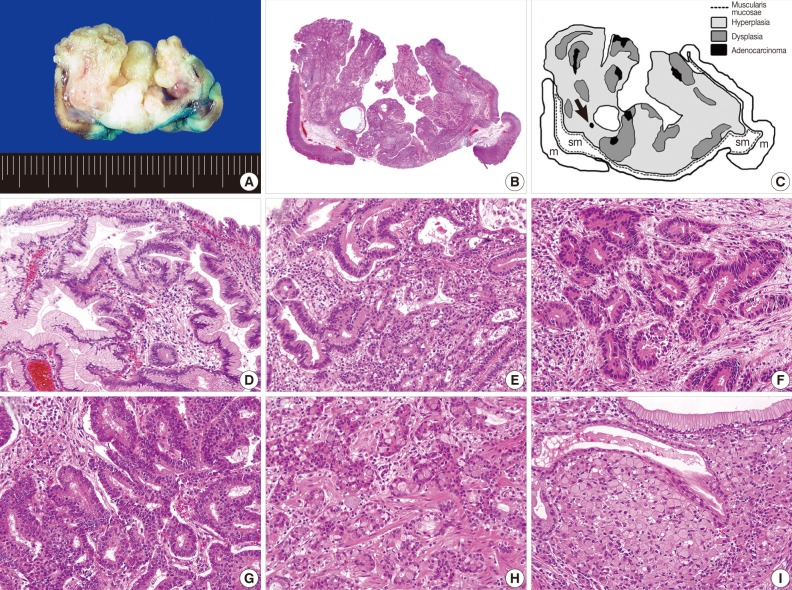
Figure & Data
References
Citations
Citations to this article as recorded by 

- Case report and literature analysis of ectopic gastric glands combined with intestinal-type gastric cancer in an HP-negative background
Shiyu Peng, Shuxin Tian
Frontiers in Oncology.2025;[Epub] CrossRef - Clinicopathologic and endoscopic characteristics of ten patients with gastric hamartomatous inverted polyp: a single center case series
Ningning Dong, Fandong Meng, Bing Yue, Junzhen Hou
BMC Gastroenterology.2024;[Epub] CrossRef - Gastric hamartomatous inverted polyp: Report of three cases with a review of the endoscopic and clinicopathological features
Takuya Ohtsu, Yu Takahashi, Mitsuo Tokuhara, Tomomitsu Tahara, Mitsuaki Ishida, Chika Miyasaka, Koji Tsuta, Makoto Naganuma
DEN Open.2023;[Epub] CrossRef - Gastric Inverted Hyperplastic Polyp Removed Using Endoscopic Submucosal Dissection
Jee Won Boo, Joon Sung Kim, Byung-Wook Kim
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2023; 23(1): 63. CrossRef - The Many Faces of Gastric Inverted Polyps: a case report
S.I. Kim, M.Y. Agapov, T.F. Savostyanov, A.A. Paratovskaya, I.A. Sokolova
Russian Journal of Evidence-Based Gastroenterology.2023; 12(2): 88. CrossRef - Large gastric hamartomatous inverted polyp accompanied by advanced gastric cancer: A case report
Gyerim Park, Jihye Kim, Sung Hak Lee, Younghoon Kim
World Journal of Clinical Cases.2023; 11(28): 6967. CrossRef - Activating KRAS and GNAS mutations in heterotopic submucosal glands of the stomach
Hourin Cho, Taiki Hashimoto, Tomoaki Naka, Yasushi Yatabe, Ichiro Oda, Yutaka Saito, Takaki Yoshikawa, Shigeki Sekine
Journal of Gastroenterology.2022; 57(5): 333. CrossRef - Gastric Inverted Polyps—Distinctive Subepithelial Lesions of the Stomach
Ji-Ye Kim, Soomin Ahn, Kyoung-Mee Kim, Sun Hee Chang, Han Seong Kim, Jun Haeng Lee, Jae J. Kim, Tae Sung Sohn, Hye Ju Kang, Mee Joo
American Journal of Surgical Pathology.2021; 45(5): 680. CrossRef - Signet-ring Cell Carcinoma in Hyperplastic Polyp of the Stomach
Kenta Yoshida, Tatsuya Mikami, Takao Oyama, Yuki Sato, Taro Saito, Takafumi Mikami, Chieko Itabashi, Yasushi Soma, Shinsaku Fukuda
Internal Medicine.2019; 58(24): 3531. CrossRef - Inverted Hyperplastic Polyp in Stomach: A Case Report and Literature Review
Yeon Ho Lee, Moon Kyung Joo, Beom Jae Lee, Ji-Ae Lee, Taehyun Kim, Jin Gu Yoon, Jung Min Lee, Jong-Jae Park
The Korean Journal of Gastroenterology.2016; 67(2): 98. CrossRef - Inflammatory myofibroblastic tumor‐like stromal proliferation within gastric inverted hyperplastic polyp
Byeong‐Joo Noh, Ji Won Min, Ji‐Youn Sung, Yong‐Koo Park, Juhie Lee, Youn Wha Kim
Pathology International.2016; 66(3): 180. CrossRef - Gastric inverted hyperplastic polyp: A rare cause of iron deficiency anemia
Jin Tak Yun, Seung Woo Lee, Dong Pil Kim, Seung Hwa Choi, Seok-Hwan Kim, Jun Kyu Park, Sun Hee Jang, Yun Jung Park, Ye Gyu Sung, Hae Jung Sul
World Journal of Gastroenterology.2016; 22(15): 4066. CrossRef - Gastric Inverted Hyperplasic Polyp Composed Only of Pyloric Glands
Minsun Jung, Kyueng-Whan Min, Young-Joon Ryu
International Journal of Surgical Pathology.2015; 23(4): 313. CrossRef - A Pedunculated Submucosal Lesion in the Stomach with Inverted Downgrowth
Yoshihiko Miyamoto, Naoki Muguruma, Seisuke Okamura, Yasuyuki Okada, Shinji Kitamura, Koichi Okamoto, Akiko Yoneda, Noriko Kagawa, Tetsuji Takayama
Internal Medicine.2014; 53(15): 1625. CrossRef
Multifocal Adenocarcinomas Arising within a Gastric Inverted Hyperplastic Polyp



Fig. 1 Endoscopic findings. (A) A subepithelial mass in the gastric body shows round superficial nodular change at the surface, with bridging of surrounding folds (right upper corner). (B) Endoscopic ultrasonography shows a heterogeneous hypoechoic tumor in the third layer of the gastric wall (arrowheads).
Fig. 2 Gross and histologic findings. (A) The mass is a well-circumscribed downward-growing lesion with a slit-shaped cavity in the center. Scanning view (B) and schematic representation (C) of the lesion, which includes regions of hyperplasia and multifocal dysplasia and adenocarcinoma. A black arrow indicates a minute focus of signet ring cell carcinoma. m, mucosa; sm, submucosa. Transitions from hyperplasia (left half) to dysplasia (right half; D) and dysplasia (periphery) to adenocarcinoma (center; E) are apparent. Each cancerous focus displays a distinctive morphology and degree of differentiation, corresponding to well (F), moderately (G) and poorly differentiated adenocarcinoma (H). (I) In contrast with other cancerous foci, the signet ring cell carcinoma is surrounded by hyperplastic epithelium, without a transitional dysplastic component.
Fig. 3 Immunohistochemical findings. Immunoreactivity to p53 protein is detected in almost all cancer cells in the adenocarcinoma (A) and signet ring cell carcinoma (B) and approximately 10% of dysplastic cells (C), but not in the hyperplastic epithelium (D).
Fig. 1
Fig. 2
Fig. 3
Multifocal Adenocarcinomas Arising within a Gastric Inverted Hyperplastic Polyp

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article