Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 54(5); 2020 > Article
-
Brief Case Report
Breast implant–associated anaplastic large cell lymphoma: the first South Korean case -
Jongwon Lee1
 , Hyungwoo Cho2
, Hyungwoo Cho2 , Dok Hyun Yoon2
, Dok Hyun Yoon2 , Eun Key Kim3
, Eun Key Kim3 , Gyungyub Gong1
, Gyungyub Gong1 , Cheolwon Suh2
, Cheolwon Suh2 , Joo-ryung Huh1
, Joo-ryung Huh1
-
Journal of Pathology and Translational Medicine 2020;54(5):432-434.
DOI: https://doi.org/10.4132/jptm.2020.07.01
Published online: August 18, 2020
1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
2Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
3Department of Plastic Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- Corresponding Author: Joo-ryung Huh, MD Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Korea Tel: +82-2-3010-4553, Fax: +82-2-472-7898, E-mail: jrhuh@amc.seoul.kr
© 2020 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
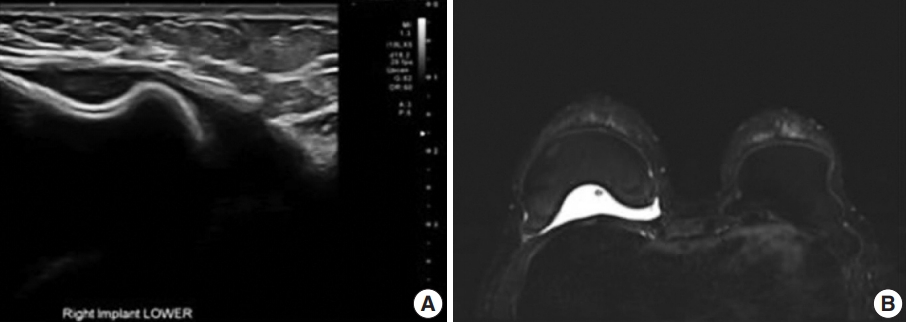
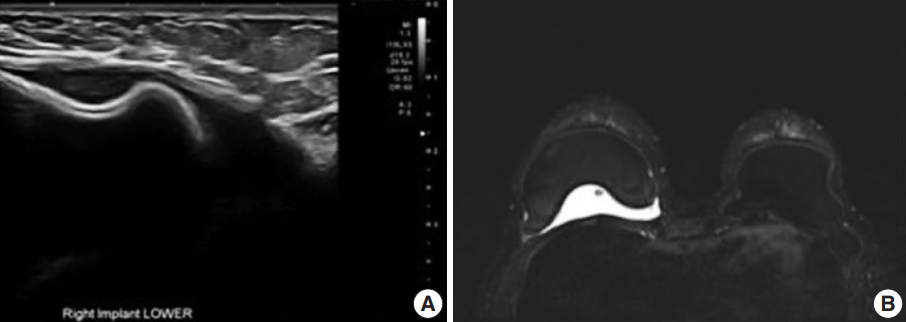
- A 47-year-old woman presented to a local clinic who had previously undergone bilateral breast augmentation via transaxillary subpectoral augmentation (TSA) in 2013 for cosmetic reasons. The implanted device was a Natrelle silicone-filled textured breast implant (style 115, BIOCELL Textured Round Midrange Projection Gel-filled Breast Implant, 253 mL, Allergan, Dublin, Ireland). Six years postoperatively, in 2019, she noticed swelling of her right breast. An ultrasonographic examination revealed fluid collection and capsule discontinuity, suggesting a ruptured implant (Fig. 1A). On magnetic resonance imaging, however, implants were found intact, though fluid collection was prominent in the inner posterior side of the right breast (Fig. 1B).
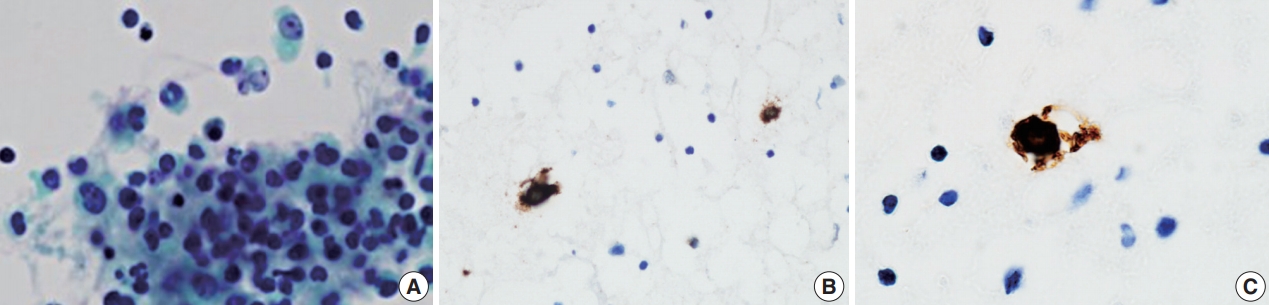
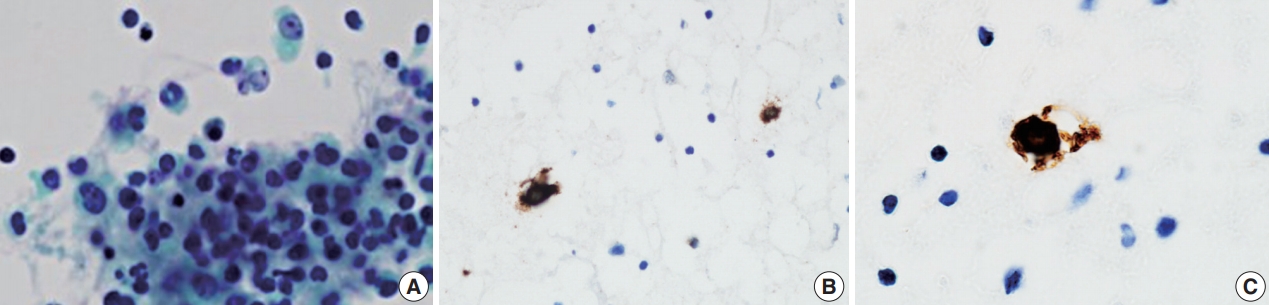
- Under the impression of implant rupture with seroma, aspiration was performed revealing large, atypical lymphocytes with irregular kidney-shaped nuclei, with occasional binucleation (Fig. 2A). These cells were confirmed as atypical T-cells positive for CD30 and CD3 and negative for anaplastic lymphoma kinase 1 per immunostaining, a typical phenotype of anaplastic lymphoma kinase (ALK)–negative BIA-ALCL (Fig. 2B, C) [1].
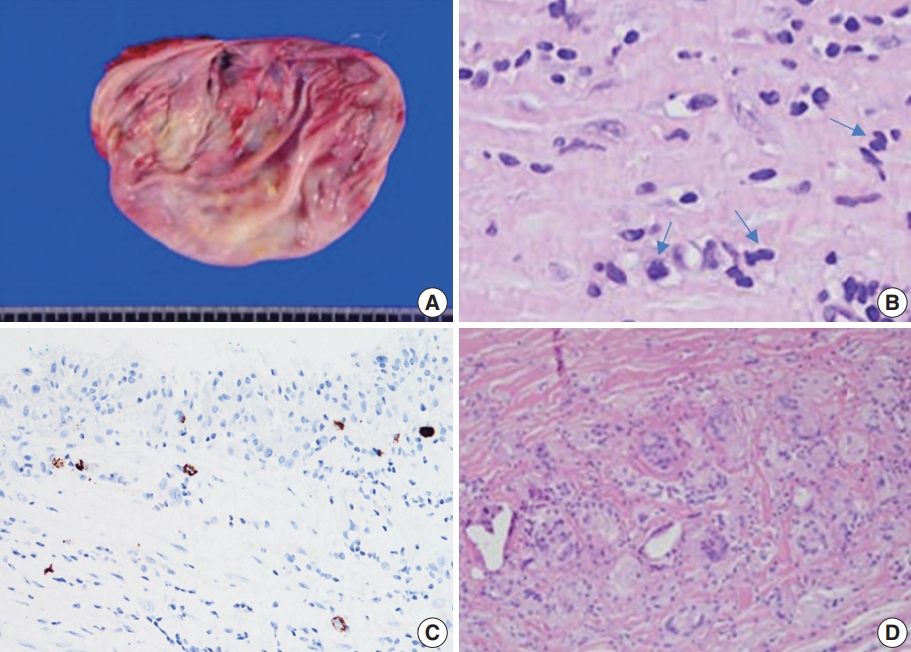
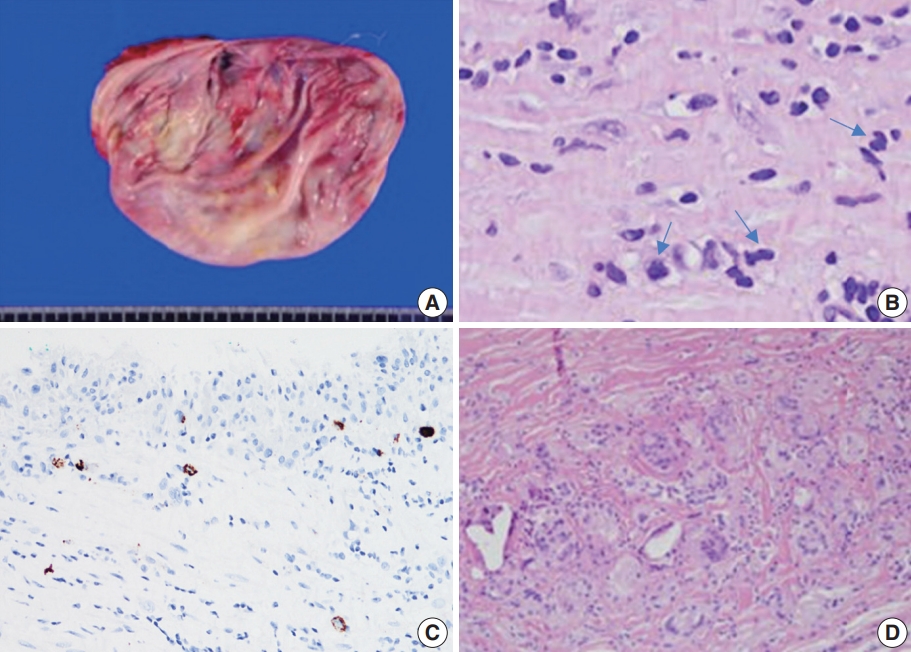
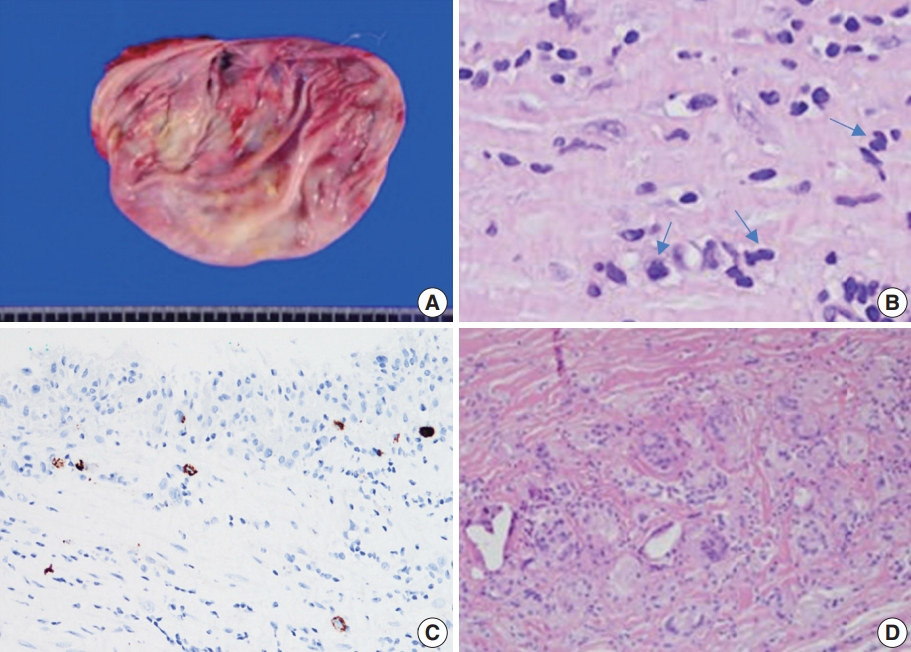
- Whole-body positron-emission tomography (PET) showed hypermetabolic capsule and fluid collection confined to the right breast. Blood test results were normal and bone marrow biopsy findings were negative for lymphoma involvement. With curative intent, the bilateral implants were removed with capsulectomy, which revealed irregular thickening of the capsule taken from the right breast with multiple focal areas of fibrinous deposits in the lining without distinct tumor masses (Fig. 3A). The implant did not show grossly identifiable foci of rupture. The capsule and implant from the left breast were unremarkable.
- According to histologic sectioning, large atypical lymphocytes positive for CD30 but negative for ALK immunostaining that had infiltrated the luminal surface of the capsule from the right breast (Fig. 3B, C) were consistent with pathologic stage T2. Focal foreign body-type macrophages were identified throughout the specimen, denoting microscopic leakage (Fig. 3D). T-cell clonality was detected on gene rearrangement study for beta T-cell and gamma T-cell receptor genes. The contralateral breast was unremarkable, with a thin capsule and the absence of atypical lymphocytes.
CASE REPORT
- BIA-ALCL is a rare type of T-cell lymphoma, occurring in recipients of either saline or silicone-filled textured type breast implants. BIA-ALCL is usually localized and the prognosis is excellent. Complete surgical removal of the capsule and implant with negative resection margins is curative in almost all patients. However, advanced-stage disease with metastasis has also been reported [2], which emphasizes the importance of the awareness of the entity and the making of an early diagnosis.
- BIA-ALCL most commonly presents as effusion around the implant simulating rupture of the implant, while tumor mass formation is less frequent. The present case to our knowledge is the first report of BIA-ALCL in a South Korean patient, with the typical presentation being similar to that in Western countries both clinically and pathologically. With 27,393 annual Allergan breast prostheses implanted in South Korea alone, one would expect a higher number of cases, so the apparent rarity of BIA-ALCL may be due to a trend of underdiagnosis. Due to the low index of suspicion, aspiration cytology is rarely performed in Korea for implant-associated effusions (personal observation, E.K.K.). The present case should raise a clinical awareness that BIA-ALCL does arise in Korean women and investigation to rule out BIA-ALCL should be performed in appropriate cases.
DISCUSSION
Ethics Statement
This case was deemed exempt by the Asan Medical Center Institutional Review Board (IRB #2020-0433). Informed consent was obtained from individual participant included in this study.
Author contributions
Conceptualization: JRH, JL, CS. Data curation: EKK, HC, DHY, JRH, JL. Methodology: JRH, JL, GG. Writing—original draft: JRH, JL. Writing—review & editing: JRH, JL. Approval of final manuscript: all authors.
Conflicts of Interest
G.G., a contributing editor of the Journal of Pathology and Translational Medicine, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding Statement
No funding to declare.
- 1. Di Napoli A, Pepe G, Giarnieri E, et al. Cytological diagnostic features of late breast implant seromas: from reactive to anaplastic large cell lymphoma. PLoS One 2017; 12: e0181097.ArticlePubMedPMC
- 2. Quesada AE, Medeiros LJ, Clemens MW, Ferrufino-Schmidt MC, Pina-Oviedo S, Miranda RN. Breast implant-associated anaplastic large cell lymphoma: a review. Mod Pathol 2019; 32: 166-88. ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

- Breast Reconstruction after Breast Implant-Associated Anaplastic Large Cell Lymphoma Treatment: A Case Report and Literature Review
Won-Seob Lee, Tae-Gon Kim, Jun-Ho Lee, Il-Kug Kim
Journal of Clinical Medicine.2023; 12(5): 1885. CrossRef - Breast filler granuloma mistaken for implant rupture: A case report
Yong Seon Hwang, Je Yeon Byeon, Jun Hyuk Kim, Hwan Jun Choi, Mee Hye Oh, Da Woon Lee
Medicine.2023; 102(22): e33785. CrossRef - Implant replacement and anaplastic large cell lymphoma associated with breast implants: a quantitative analysis
Martina Vittorietti, Sergio Mazzola, Claudio Costantino, Daniele Domenico De Bella, Santo Fruscione, Nicole Bonaccorso, Martina Sciortino, Davide Costanza, Miriam Belluzzo, Alessandra Savatteri, Fabio Tramuto, Paolo Contiero, Giovanna Tagliabue, Palmira I
Frontiers in Oncology.2023;[Epub] CrossRef - Breast implant-associated anaplastic large cell lymphoma: a case report with a history of spontaneously resolved late seroma
Do Yeon Kim, Joon Hur, Woo Yeon Han, Kyunghyun Min, Jong Won Lee, Jin Sup Eom, Hyun Ho Han, Eun Key Kim
Archives of Aesthetic Plastic Surgery.2021; 27(4): 143. CrossRef - Comment on “Breast implant-associated anaplastic large cell lymphoma: the first South Korean case”
Il-Kug Kim, Tae Gon Kim
Journal of Pathology and Translational Medicine.2021; 55(6): 419. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure



 E-submission
E-submission