Previous issues
- Page Path
- HOME > Articles and issues > Previous issues
Reviews
- Immune landscape and biomarkers for immuno-oncology in colorectal cancers
- Jeong Mo Bae, Seung-Yeon Yoo, Jung Ho Kim, Gyeong Hoon Kang
- J Pathol Transl Med. 2020;54(5):351-360. Published online June 26, 2020
- DOI: https://doi.org/10.4132/jptm.2020.05.15
- 8,174 View
- 319 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF - Recent advances in immuno-oncology have increased understanding of the tumor immune microenvironment (TIME), and clinical trials for immune checkpoint inhibitor treatment have shown remission and/or durable response in certain proportions of patients stratified by predictive biomarkers. The TIME in colorectal cancer (CRC) was initially evaluated several decades ago. The prognostic value of the immune response to tumors, including tumor-infiltrating lymphocytes, peritumoral lymphoid reaction, and Crohn’s-like lymphoid reaction, has been well demonstrated. In this review, we describe the chronology of TIME research and review the up-to-date high-dimensional TIME landscape of CRC. We also summarize the clinical relevance of several biomarkers associated with immunotherapy in CRC, such as microsatellite instability, tumor mutational burden, POLE/POLD mutation, consensus molecular subtype, and programmed death-ligand 1 expression.
-
Citations
Citations to this article as recorded by- Targeting the “tumor microenvironment”: RNA-binding proteins in the spotlight in colorectal cancer therapy
Yiwei Zhang, Yujun Zhang, Jingjing Song, Xifu Cheng, Chulin Zhou, Shuo Huang, Wentao Zhao, Zhen Zong, Lingling Yang
International Immunopharmacology.2024; 131: 111876. CrossRef - Five decades of colorectal cancer pathology: The World and China
Maode Lai
Chinese Science Bulletin.2024;[Epub] CrossRef - T cell receptor clonotype in tumor microenvironment contributes to intratumoral signaling network in patients with colorectal cancer
In Hye Song, Seung-been Lee, Byung-Kwan Jeong, Jungwook Park, Honggeun Kim, GunHee Lee, Su Min Cha, Heejae Lee, Gyungyub Gong, Nak-Jung Kwon, Hee Jin Lee
Immunologic Research.2024; 72(5): 921. CrossRef - Identification of Key Immune and Cell Cycle Modules and Prognostic Genes for Glioma Patients through Transcriptome Analysis
Kaimin Guo, Jinna Yang, Ruonan Jiang, Xiaxia Ren, Peng Liu, Wenjia Wang, Shuiping Zhou, Xiaoguang Wang, Li Ma, Yunhui Hu
Pharmaceuticals.2024; 17(10): 1295. CrossRef - Unraveling the Role of Molecular Profiling in Predicting Treatment Response in Stage III Colorectal Cancer Patients: Insights from the IDEA International Study
Ippokratis Messaritakis, Eleni Psaroudaki, Konstantinos Vogiatzoglou, Maria Sfakianaki, Pantelis Topalis, Ioannis Iliopoulos, Dimitrios Mavroudis, John Tsiaoussis, Nikolaos Gouvas, Maria Tzardi, John Souglakos
Cancers.2023; 15(19): 4819. CrossRef - Biomarkers for Predicting Response to Personalized Immunotherapy in Gastric Cancer
Moonsik Kim, Ji Yun Jeong, An Na Seo
Diagnostics.2023; 13(17): 2782. CrossRef - Evaluation on Braking Stability of Autonomous Vehicles Running along Curved Sections Based on Asphalt Pavement Adhesion Properties
Binshuang Zheng, Xiaoming Huang, Junyao Tang, Jiaying Chen, Runmin Zhao, Zhengqiang Hong, Tao Tang, Meiling Han, Yang Yang
Journal of Advanced Transportation.2022; 2022: 1. CrossRef - Intratumoral spatial heterogeneity of tumor-infiltrating lymphocytes is a significant factor for precisely stratifying prognostic immune subgroups of microsatellite instability-high colorectal carcinomas
Minsun Jung, Ji Ae Lee, Seung-Yeon Yoo, Jeong Mo Bae, Gyeong Hoon Kang, Jung Ho Kim
Modern Pathology.2022; 35(12): 2011. CrossRef - Association of Tumor-Infiltrating Lymphocytes With Survival in Stages II and III Colorectal Cancer
Marina Vitorino, Inês Eiriz, Tiago C Tomás, Rodrigo Vicente, Ana Mendes, Ana Rita Freitas, Sofia Braga, Catarina Alves-Vale, Paula Borralho, André Ferreira, Luisa Leal da Costa
Cureus.2022;[Epub] CrossRef - Tumor Mutational Burden Predicting the Efficacy of Immune Checkpoint Inhibitors in Colorectal Cancer: A Systematic Review and Meta-Analysis
Yan Li, Yiqi Ma, Zijun Wu, Fanxin Zeng, Bin Song, Yanrong Zhang, Jinxing Li, Su Lui, Min Wu
Frontiers in Immunology.2021;[Epub] CrossRef - Genomic and transcriptomic characterization of heterogeneous immune subgroups of microsatellite instability-high colorectal cancers
Jung Ho Kim, Mi-Kyoung Seo, Ji Ae Lee, Seung-Yeon Yoo, Hyeon Jeong Oh, Hyundeok Kang, Nam-Yun Cho, Jeong Mo Bae, Gyeong Hoon Kang, Sangwoo Kim
Journal for ImmunoTherapy of Cancer.2021; 9(12): e003414. CrossRef
- Targeting the “tumor microenvironment”: RNA-binding proteins in the spotlight in colorectal cancer therapy
- Thyroid fine-needle aspiration cytology in Taiwan: a nationwide survey and literature update
- Chien-Chin Chen, Jen-Fan Hang, Chih-Yi Liu, Yeh-Han Wang, Chiung-Ru Lai
- J Pathol Transl Med. 2020;54(5):361-366. Published online August 31, 2020
- DOI: https://doi.org/10.4132/jptm.2020.07.17
- 5,488 View
- 157 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
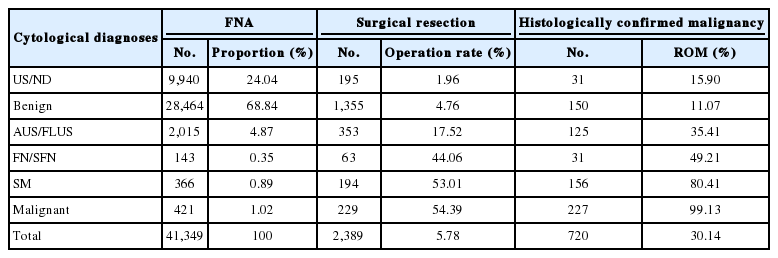
PDF - In Taiwan, thyroid fine-needle aspiration cytology is easily accessible and reliable for evaluating thyroid nodules. The sonographic pattern plays a major role and is the deciding factor for aspiration. We conducted a nationwide survey in 2017 and it revealed that 31% of laboratories had adopted The Bethesda System for Reporting Thyroid Cytopathology. There was a relatively high unsatisfactory rate (24.04%) and low rates of indeterminate diagnoses, including atypia of undetermined significance/follicular lesions of undetermined significance: 4.87%, and follicular neoplasm/suspicious for a follicular neoplasm: 0.35%. Moreover, the risks of malignancy in benign, atypia of undetermined significance, and suspicious for a follicular neoplasm were relatively high. These may reflect strict diagnostic criteria for indeterminate categories and better patient selection for surgery. Improvements in specimen sampling and continuing education programs are crucial. Newly-developed thyroid cytology technologies, such as immunocytochemistry, molecular testing, and computerized cytomorphometry, may further facilitate cytology diagnoses.
-
Citations
Citations to this article as recorded by- Diagnostic values of SurePath liquid‐based cytology versus conventional smear in thyroid aspiration samples: A 13‐year experience at a single institution
Wen‐Ying Lee, Hsiu‐Chu Wang, Lee‐E Huang, Min‐Hui Tseng, Shu‐Hui Chiang, Ching‐Chien Lee
Diagnostic Cytopathology.2024; 52(7): 369. CrossRef - Comparison of fine-needle aspiration with fine-needle capillary cytology in thyroid nodules
H Hatami, M Samsami, S Movahedinia, B Salehi, M Movahedinia, M Ardeshir
The Annals of The Royal College of Surgeons of England.2023; 105(2): 162. CrossRef - Identification of NIFTP-Specific mRNA Markers for Reliable Molecular Diagnosis of Thyroid Tumors
So-Yeon Lee, Jong-Lyul Park, Kwangsoon Kim, Ja Seong Bae, Jae-Yoon Kim, Seon-Young Kim, Chan Kwon Jung
Endocrine Pathology.2023; 34(3): 311. CrossRef - Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: its updated diagnostic criteria, preoperative cytologic diagnoses and impact on the risk of malignancy
Hee Young Na, So Yeon Park
Journal of Pathology and Translational Medicine.2022; 56(6): 319. CrossRef - Thyroid malignancy rates according to the Bethesda reporting system in Israel - A multicenter study
Ory Madgar, Galit Avior, Isaac Shochat, Ben-Zion Joshua, Lior Baraf, Yuval Avidor, Avi khafif, Niddal Assadi, Eran E. Alon
European Journal of Surgical Oncology.2021; 47(6): 1370. CrossRef
- Diagnostic values of SurePath liquid‐based cytology versus conventional smear in thyroid aspiration samples: A 13‐year experience at a single institution
- Pathologic interpretation of endoscopic ultrasound–guided fine needle aspiration cytology/biopsy for pancreatic lesions
- Haeryoung Kim, Kee-Taek Jang
- J Pathol Transl Med. 2020;54(5):367-377. Published online August 31, 2020
- DOI: https://doi.org/10.4132/jptm.2020.07.21
- 6,940 View
- 210 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pathologic interpretation of endoscopic ultrasound–guided fine needle aspiration (EUS-FNA) cytology/biopsy specimens is one of the most challenging tasks in cytology and surgical pathology practice, as the procedure often yields minimal amounts of diagnostic material and contains contaminants, such as blood cells and normal intestinal mucosa. EUS-FNA cytology/biopsy will nevertheless become a more popular procedure for evaluation of various pancreatic lesions because they are difficult to approach with conventional endoscopic procedures. Pathologists should understand the structural differences and limitations of EUS-FNA that make pathologic diagnosis difficult. Ancillary tests are available for differential diagnosis of EUS-FNA for various pancreatic lesions. Immunostains are the most commonly used ancillary tests, and pathologists should able to choose the necessary panel for differential diagnosis. Pathologists should review clinical history and radiologic and/or EUS findings before selecting an immunostain panel and making a pathologic diagnosis. In addition, one’s threshold of malignancy should be adjusted according to the appropriate clinical setting to avoid under-evaluation of pathologic diagnoses. Clinico-pathologic correlation is essential in pathologic evaluation of EUS-FNA for pancreatic lesions. Pathologists can reduce errors by correlating clinical and radiologic findings when evaluating EUS-FNA. Some molecular tests can be applied in differential diagnosis of pancreatic neoplastic and cystic lesions. Molecular data should be used as supportive evidence of a specific disease entity, rather than direct evidence, and should be correlated with clinico-pathologic findings to avoid errors in pathologic diagnosis.
-
Citations
Citations to this article as recorded by- Endoscopic Ultrasound-Guided Pancreatic Tissue Sampling: Lesion Assessment, Needles, and Techniques
Jahnvi Dhar, Jayanta Samanta, Zaheer Nabi, Manik Aggarwal, Maria Cristina Conti Bellocchi, Antonio Facciorusso, Luca Frulloni, Stefano Francesco Crinò
Medicina.2024; 60(12): 2021. CrossRef - A prospective randomized noninferiority trial comparing conventional smears and SurePathTM liquid-based cytology in endoscopic ultrasound-guided sampling of esophageal, gastric, and duodenal lesions
Jae Chang Jun, Sang Hyub Lee, Han Myung Lee, Sang Gyun Kim, Hyunsoo Chung, Joo Seong Kim, Namyoung Park, Jin Ho Choi, Yoonjin Kwak, Soo-Jeong Cho
Medicine.2023; 102(29): e34321. CrossRef - Double Ki-67 and synaptophysin labeling in pancreatic neuroendocrine tumor biopsies
Bokyung Ahn, Jin Kying Jung, HaeSung Jung, Yeon-Mi Ryu, Yeon Wook Kim, Tae Jun Song, Do Hyun Park, Dae wook Hwang, HyungJun Cho, Sang-Yeob Kim, Seung-Mo Hong
Pancreatology.2022; 22(3): 427. CrossRef - Comparison of Endoscopic Ultrasound-Guided Fine Needle Aspiration with 19-Gauge and 22-Gauge Needles for Solid Pancreatic Lesions
Changjuan Li, Jianwei Mi, Fulai Gao, Xinying Zhu, Miao Su, Xiaoli Xie, Dongqiang Zhao
International Journal of General Medicine.2021; Volume 14: 10439. CrossRef
- Endoscopic Ultrasound-Guided Pancreatic Tissue Sampling: Lesion Assessment, Needles, and Techniques
Original Articles
- Prediction of TP53 mutations by p53 immunohistochemistry and their prognostic significance in gastric cancer
- Hye Jung Hwang, Soo Kyung Nam, Hyunjin Park, Yujun Park, Jiwon Koh, Hee Young Na, Yoonjin Kwak, Woo Ho Kim, Hye Seung Lee
- J Pathol Transl Med. 2020;54(5):378-386. Published online July 1, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.01
- 9,071 View
- 269 Download
- 37 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Recently, molecular classifications of gastric cancer (GC) have been proposed that include TP53 mutations and their functional activity. We aimed to demonstrate the correlation between p53 immunohistochemistry (IHC) and TP53 mutations as well as their clinicopathological significance in GC.
Methods
Deep targeted sequencing was performed using surgical or biopsy specimens from 120 patients with GC. IHC for p53 was performed and interpreted as strong, weak, or negative expression. In 18 cases (15.0%) with discrepant TP53 mutation and p53 IHC results, p53 IHC was repeated.
Results
Strong expression of p53 was associated with TP53 missense mutations, negative expression with other types of mutations, and weak expression with wild-type TP53 (p<.001). The sensitivity for each category was 90.9%, 79.0%, and 80.9%, and the specificity was 95.4%, 88.1%, and 92.3%, respectively. The TNM stage at initial diagnosis exhibited a significant correlation with both TP53 mutation type (p=.004) and p53 expression status (p=.029). The Kaplan-Meier survival analysis for 109 stage II and III GC cases showed that patients with TP53 missense mutations had worse overall survival than those in the wild-type and other mutation groups (p=.028). Strong expression of p53 was also associated with worse overall survival in comparison to negative and weak expression (p=.035).
Conclusions
Results of IHC of the p53 protein may be used as a simple surrogate marker of TP53 mutations. However, negative expression of p53 and other types of mutations of TP53 should be carefully interpreted because of its lower sensitivity and different prognostic implications. -
Citations
Citations to this article as recorded by- The future is now: advancing p53 immunohistochemistry in Barrett's oesophagus and its implication for the everyday pathologist
Yevgen Chornenkyy, Monika Vyas, Vikram Deshpande
Histopathology.2025;[Epub] CrossRef - Multiple approaches revealed MGc80‐3 as a somatic hybrid with HeLa cells rather than a gastric cancer cell line
Fang Cao, Hao Sun, Zhenli Yang, Yanhua Bai, Xiao Hu, Yuhong Hou, Xiaocui Bian, Yuqin Liu
International Journal of Cancer.2024; 154(1): 155. CrossRef - In Response to p53 Immunohistochemical Staining and TP53 Gene Mutations in Endometrial Cancer: Does Null Pattern Correlate With Prognosis?
Ikuko Sakamoto, Keiko Kagami, Takahiro Nozaki, Yosuke Hirotsu, Kenji Amemiya, Toshio Oyama, Masao Omata
American Journal of Surgical Pathology.2024; 48(3): 374. CrossRef - CHEK2 germline variants identified in familial nonmedullary thyroid cancer lead to impaired protein structure and function
Carolina Pires, Inês J. Marques, Mariana Valério, Ana Saramago, Paulo E. Santo, Sandra Santos, Margarida Silva, Margarida M. Moura, João Matos, Teresa Pereira, Rafael Cabrera, Diana Lousa, Valeriano Leite, Tiago M. Bandeiras, João B. Vicente, Branca M. Ca
Journal of Biological Chemistry.2024; 300(3): 105767. CrossRef - The spectrum of TP53 mutations in Rwandan patients with gastric cancer
Augustin Nzitakera, Jean Bosco Surwumwe, Ella Larissa Ndoricyimpaye, Schifra Uwamungu, Delphine Uwamariya, Felix Manirakiza, Marie Claire Ndayisaba, Gervais Ntakirutimana, Benoit Seminega, Vincent Dusabejambo, Eric Rutaganda, Placide Kamali, François Ngab
Genes and Environment.2024;[Epub] CrossRef - Gastric cancer molecular classification based on immunohistochemistry and in‐situ hybridisation and mortality
Maarit Eskuri, Eva‐Maria Birkman, Joonas H Kauppila
Histopathology.2024; 85(2): 327. CrossRef - Redefining aberrant P53 expression of gastric cancer and its distinct clinical significance among molecular-histologic subtypes
Shih-Chiang Huang, Ian Yi-Feng Chang, Tse-Ching Chen, Hsiao-Ching Lin, Chun-Yi Tsai, Jun-Te Hsu, Chun-Nan Yeh, Shih-Cheng Chang, Ta-Sen Yeh
Asian Journal of Surgery.2024; 47(11): 4699. CrossRef - Assessment of TP53 and CDKN2A status as predictive markers of malignant transformation of sinonasal inverted papilloma
Soohyeon Kwon, Jeong-Whun Kim, Eun Sun Kim, Jin Ho Paik, Jin-Haeng Chung, Sung-Woo Cho, Tae-Bin Won, Chae-Seo Rhee, Jee Hye Wee, Hyojin Kim
Scientific Reports.2024;[Epub] CrossRef - Implementing an integrated molecular classification for gastric cancer from endoscopic biopsies using on-slide tests
Simona Costache, Adelina Baltan , Sofia Diaz McLinn , Mattia Pegoraro , Rebecca de Havilland , Matthew Porter , Ana Lerga , Teresa Thomas , Alina Elena Chefani
Romanian Journal of Morphology and Embryology.2024; 65(2): 257. CrossRef - Application of NGS molecular classification in the diagnosis of endometrial carcinoma: A supplement to traditional pathological diagnosis
Qunxian Rao, Jianwei Liao, Yangyang Li, Xin Zhang, Guocai Xu, Changbin Zhu, Shengya Tian, Qiuhong Chen, Hui Zhou, Bingzhong Zhang
Cancer Medicine.2023; 12(5): 5409. CrossRef - Predictive value of p53 and AXL immunostaining for the efficacy of immune checkpoint inhibitor-based therapy after osimertinib treatment in patients with epidermal growth factor-mutant non-small cell lung cancer
Kenji Morimoto, Tadaaki Yamada, Ryo Sawada, Koichi Azuma, Yasuhiro Goto, Taishi Harada, Shinsuke Shiotsu, Nobuyo Tamiya, Yusuke Chihara, Takayuki Takeda, Osamu Hiranuma, Isao Hasegawa, Satomi Tanaka, Akihiro Yoshimura, Masahiro Iwasaku, Shinsaku Tokuda, Y
Cancer Immunology, Immunotherapy.2023; 72(6): 1699. CrossRef - Validation of p53 Immunohistochemistry (PAb240 Clone) in Canine Tumors with Next-Generation Sequencing (NGS) Analysis
Barbara Brunetti, Dario de Biase, Giulia Dellapina, Luisa Vera Muscatello, Francesco Ingravalle, Giorgia Tura, Barbara Bacci
Animals.2023; 13(5): 899. CrossRef - Mesonephric‐like adenocarcinoma of the female genital tract: novel observations and detailed molecular characterisation of mixed tumours and mesonephric‐like carcinosarcomas
Jelena Mirkovic, Ekaterina Olkhov‐Mitsel, Yutaka Amemiya, Maysa Al‐Hussaini, Sharon Nofech‐Mozes, Bojana Djordjevic, Rachel Kupets, Arun Seth, W Glenn McCluggage
Histopathology.2023; 82(7): 978. CrossRef - Clinicopathologic characterization of cervical metastasis from an unknown primary tumor: a multicenter study in Korea
Miseon Lee, Uiree Jo, Joon Seon Song, Youn Soo Lee, Chang Gok Woo, Dong-Hoon Kim, Jung Yeon Kim, Sun Och Yoon, Kyung-Ja Cho
Journal of Pathology and Translational Medicine.2023; 57(3): 166. CrossRef - P53 in Penile Squamous Cell Carcinoma: A Pattern-Based Immunohistochemical Framework with Molecular Correlation
Isabel Trias, Adela Saco, Lorena Marimon, Ricardo López del Campo, Carolina Manzotti, Oriol Ordi, Marta del Pino, Francisco M. Pérez, Naiara Vega, Silvia Alós, Antonio Martínez, Leonardo Rodriguez-Carunchio, Oscar Reig, Pedro Jares, Cristina Teixido, Tare
Cancers.2023; 15(10): 2719. CrossRef - p53/TP53 Status Assessment in Gastroesophageal Adenocarcinoma
Elisa Boldrin, Maria Assunta Piano, Francesco Bernaudo, Rita Alfieri, Maria Raffaella Biasin, Isabella Monia Montagner, Alice Volpato, Genny Mattara, Francesco Lamacchia, Giovanna Magni, Antonio Rosato, Antonio Scapinello, Pierluigi Pilati, Matteo Curtare
Cancers.2023; 15(10): 2783. CrossRef - Genomic profiling of dedifferentiated endometrial carcinomas arising in the background of high‐grade carcinoma: a targeted next‐generation sequencing study
Ekaterina Olkhov‐Mitsel, Aurelia Busca, Carlos Parra‐Herran, Yutaka Amemiya, Sharon Nofech‐Mozes, Bojana Djordjevic, Marisa R Nucci, Arun Seth, Jelena Mirkovic
Histopathology.2023; 83(3): 366. CrossRef -
Clinicopathologic Features and Prognostic Significance of Immunohistochemistry and In Situ Hybridization Based Molecular Classification in Gastric Carcinoma
Gizem Issin, İlyas Sayar, Fatih Demir, İrem Güvendir Bakkaloğlu, Mehmet Gamsizkan, Zeliha Yildiz, Ismail Yilmaz, Sevilay Akalp Özmen, Diren Vuslat Çağatay, Itır Ebru Zemheri, Murat Demiriz, Armağan Günal
Journal of Environmental Pathology, Toxicology and Oncology.2023; 42(4): 1. CrossRef - Clinicopathologic and Molecular Characterization of Anorectal Neuroendocrine Carcinomas Reveals Human Papillomavirus, p53, and c-Myc as Alternative Mechanisms of Carcinogenesis
Allison J. Cox, William E. Crowe, Qi Yang, Bin Zhang, Zoltán N. Oltvai, Xiaoyan Liao
Modern Pathology.2023; 36(11): 100295. CrossRef - Dedifferentiated Endometrial Carcinoma: A Rare Aggressive Neoplasm-Clinical, Morphological and Immunohistochemical Features
Giovanna Giordano, Elena Ferioli, Debora Guareschi, Alessandro Tafuni
Cancers.2023; 15(21): 5155. CrossRef - Characterization on the oncogenic effect of the missense mutations of p53 via machine learning
Qisheng Pan, Stephanie Portelli, Thanh Binh Nguyen, David B Ascher
Briefings in Bioinformatics.2023;[Epub] CrossRef - Adrenal Nodules Detected at Staging CT in Patients with Resectable Gastric Cancers Have a Low Incidence of Malignancy
Hae Young Kim, Won Chang, Yoon Jin Lee, Ji Hoon Park, Jungheum Cho, Hee Young Na, Hyungwoo Ahn, Sung Il Hwang, Hak Jong Lee, Young Hoon Kim, Kyoung Ho Lee
Radiology.2022; 302(1): 129. CrossRef - Intestinal-type gastric dysplasia in Helicobacter pylori-naïve patients
Kotaro Shibagaki, Ayako Itawaki, Yoichi Miyaoka, Kenichi Kishimoto, Yusuke Takahashi, Satoshi Kotani, Tsuyoshi Mishiro, Naoki Oshima, Kousaku Kawashima, Norihisa Ishimura, Hideyuki Onuma, Makoto Nagasaki, Mamiko Nagase, Asuka Araki, Kyuichi Kadota, Ryoji
Virchows Archiv.2022; 480(4): 783. CrossRef - Dedifferentiation-like tubular and solid carcinoma of the stomach shows phenotypic divergence and association with deficient SWI/SNF complex
Shih-Chiang Huang, Kuang-Hua Chen, Kwai-Fong Ng, I-Chieh Lin, Yi-Chun Chao, Ta-Sen Yeh, Huei-Chieh Chuang, Tse-Ching Chen
Virchows Archiv.2022; 480(4): 771. CrossRef - Distinct molecular phenotype and the potential prognostic value of immune prognostic index and tumor infiltrating lymphocytes in hepatoid adenocarcinoma of stomach
Muxing Kang, Xiaojing Ma, Jifei Shi, Guofeng Chen, Xiaoli Jin, Jun Wang, Lele Lin, Zhiwei Wu, Kaibo Chen, Jinghong Xu, Pintong Huang, Jian Chen
Translational Oncology.2022; 19: 101380. CrossRef - Evaluation of Tumor DNA Sequencing Results in Patients with Gastric and Gastroesophageal Junction Adenocarcinoma Stratified by TP53 Mutation Status
Anthony C Wood, Yonghong Zhang, Qianxing Mo, Ling Cen, Jacques Fontaine, Sarah E Hoffe, Jessica Frakes, Sean P Dineen, Jose M Pimiento, Christine M Walko, Rutika Mehta
The Oncologist.2022; 27(4): 307. CrossRef - Comprehensive Clinical Analysis of Gallbladder Neuroendocrine Neoplasms: A Large-Volume Multicenter Study During One Decade
Yangyang Wang, Bingfeng Huang, Qihan Fu, Jianing Wang, Mao Ye, Manyi Hu, Kai Qu, Kai Liu, Xiao Hu, Shumei Wei, Ke Sun, Wenbo Xiao, Bo Zhang, Haijun Li, Jingsong Li, Qi Zhang, Tingbo Liang
Annals of Surgical Oncology.2022; 29(12): 7619. CrossRef - Expression of SASP, DNA Damage Response, and Cell Proliferation Factors in Early Gastric Neoplastic Lesions: Correlations and Clinical Significance
Li Liang, Yijie Chai, Fei Chai, Haijing Liu, Ningning Ma, Hong Zhang, Shuang Zhang, Lin Nong, Ting Li, Bo Zhang
Pathology and Oncology Research.2022;[Epub] CrossRef - Systems biology and OMIC data integration to understand gastrointestinal cancers
Iasmin Moreira Costa Bispo, Henry Paul Granger, Palloma Porto Almeida, Patricia Belini Nishiyama, Leandro Martins de Freitas
World Journal of Clinical Oncology.2022; 13(10): 762. CrossRef - MicroRNA-552 expression in colorectal cancer and its clinicopathological significance
Joon Im, Soo Kyung Nam, Hye Seung Lee
Journal of Pathology and Translational Medicine.2021; 55(2): 125. CrossRef - Different effects of p53 protein overexpression on the survival of gastric cancer patients according to Lauren histologic classification: a retrospective study
Ki Wook Kim, Nayoung Kim, Yonghoon Choi, Won Seok Kim, Hyuk Yoon, Cheol Min Shin, Young Soo Park, Dong Ho Lee, Young Suk Park, Sang-Hoon Ahn, Do Joong Park, Hyung-Ho Kim, Hye Seung Lee, Ji-Won Kim, Jin Won Kim, Keun-Wook Lee, Won Chang, Ji Hoon Park, Yoon
Gastric Cancer.2021; 24(4): 844. CrossRef - The association between the expression of nuclear Yes-associated protein 1 (YAP1) and p53 protein expression profile in breast cancer patients
Yoon Jin Cha, Dooreh Kim, Soong June Bae, Sung Gwe Ahn, Joon Jeong, Min Kyung Cho, Pill Sun Paik, Tae-Kyung Yoo, Woo-Chan Park, Chang Ik Yoon, Elda Tagliabue
PLOS ONE.2021; 16(5): e0250986. CrossRef
- The future is now: advancing p53 immunohistochemistry in Barrett's oesophagus and its implication for the everyday pathologist
- Lymph node size and its association with nodal metastasis in ductal adenocarcinoma of the pancreas
- Jaehoon Shin, Seungbeom Shin, Jae Hoon Lee, Ki Byung Song, Dae Wook Hwang, Hyoung Jung Kim, Jae Ho Byun, HyungJun Cho, Song Cheol Kim, Seung-Mo Hong
- J Pathol Transl Med. 2020;54(5):387-395. Published online July 21, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.23
- 9,365 View
- 128 Download
- 13 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Although lymph node metastasis is a poor prognostic factor in patients with pancreatic ductal adenocarcinoma (PDAC), our understanding of lymph node size in association with PDAC is limited. Increased nodal size in preoperative imaging has been used to detect node metastasis. We evaluated whether lymph node size can be used as a surrogate preoperative marker of lymph node metastasis.
Methods
We assessed nodal size and compared it to the nodal metastatic status of 200 patients with surgically resected PDAC. The size of all lymph nodes and metastatic nodal foci were measured along the long and short axis, and the relationships between nodal size and metastatic status were compared at six cutoff points.
Results
A total of 4,525 lymph nodes were examined, 9.1% of which were metastatic. The mean size of the metastatic nodes (long axis, 6.9±5.0 mm; short axis, 4.3±3.1 mm) was significantly larger than that of the non-metastatic nodes (long axis, 5.0±4.0 mm; short axis, 3.0±2.0 mm; all p<.001). Using a 10 mm cutoff, the sensitivity, specificity, positive predictive value, overall accuracy, and area under curve was 24.8%, 88.0%, 17.1%, 82.3%, and 0.60 for the long axis and 7.0%, 99.0%, 40.3%, 90.6%, and 0.61 for the short axis, respectively.
Conclusions
The metastatic nodes are larger than the non-metastatic nodes in PDAC patients. However, the difference in nodal size was too small to be identified with preoperative imaging. The performance of preoperative radiologic imaging to predict lymph nodal metastasis was not good. Therefore, nodal size cannot be used a surrogate preoperative marker of lymph node metastasis. -
Citations
Citations to this article as recorded by- Long‐term outcomes of neoadjuvant gemcitabine, nab‐paclitaxel, and S1 (GAS) in borderline resectable pancreatic cancer with arterial contact: Results from a phase II trial
Kenichiro Uemura, Naru Kondo, Takeshi Sudo, Tatsuaki Sumiyoshi, Ryuta Shintakuya, Kenjiro Okada, Kenta Baba, Takumi Harada, Yoshiaki Murakami, Shinya Takahashi
Journal of Hepato-Biliary-Pancreatic Sciences.2024; 31(5): 351. CrossRef - Comparison of MRI and CT-based radiomics for preoperative prediction of lymph node metastasis in pancreatic ductal adenocarcinoma
Piaoe Zeng, Chao Qu, Jianfang Liu, Jingjing Cui, Xiaoming Liu, Dianrong Xiu, Huishu Yuan
Acta Radiologica.2023; 64(7): 2221. CrossRef - Prevalence of Adenopathy at Chest Computed Tomography After Vaccination for Severe Acute Respiratory Syndrome Coronavirus 2
Georgeann McGuinness, Jeffrey B. Alpert, Geraldine Brusca-Augello, Lea Azour, Jane P. Ko, Farah Tamizuddin, Elliott K. Gozansky, William H. Moore
Journal of Computer Assisted Tomography.2023; 47(1): 50. CrossRef - Predictive role of radiomics features extracted from preoperative cross-sectional imaging of pancreatic ductal adenocarcinoma in detecting lymph node metastasis: a systemic review and meta-analysis
Mohammad Mirza-Aghazadeh-Attari, Seyedeh Panid Madani, Haneyeh Shahbazian, Golnoosh Ansari, Alireza Mohseni, Ali Borhani, Shadi Afyouni, Ihab R. Kamel
Abdominal Radiology.2023; 48(8): 2570. CrossRef - Regional lymph node metastasis detected on preoperative CT and/or FDG-PET may predict early recurrence of pancreatic adenocarcinoma after curative resection
Ja Kyung Yoon, Mi-Suk Park, Seung-Seob Kim, Kyunghwa Han, Hee Seung Lee, Seungmin Bang, Ho Kyoung Hwang, Sang Hyun Hwang, Mijin Yun, Myeong-Jin Kim
Scientific Reports.2022;[Epub] CrossRef - Role of CA 19.9 in the Management of Resectable Pancreatic Cancer: State of the Art and Future Perspectives
Alessandro Coppola, Vincenzo La Vaccara, Tommaso Farolfi, Michele Fiore, Roberto Cammarata, Sara Ramella, Roberto Coppola, Damiano Caputo
Biomedicines.2022; 10(9): 2091. CrossRef - Evaluation of the 8th Edition AJCC Staging System for the Clinical Staging of Pancreatic Cancer
Huapyong Kang, Seung-seob Kim, Min Je Sung, Jung Hyun Jo, Hee Seung Lee, Moon Jae Chung, Jeong Youp Park, Seung Woo Park, Si Young Song, Mi-Suk Park, Seungmin Bang
Cancers.2022; 14(19): 4672. CrossRef - Does direct invasion of peripancreatic lymph nodes impact survival in patients with pancreatic ductal adenocarcinoma? A retrospective dual-center study
Daisuke Hashimoto, Sohei Satoi, Mitsuaki Ishida, Kenji Nakagawa, Masaya Kotsuka, Tadataka Takagi, Hironori Ryota, Taichi Terai, Tatsuma Sakaguchi, Minako Nagai, So Yamaki, Takahiro Akahori, Tomohisa Yamamoto, Mitsugu Sekimoto, Masayuki Sho
Pancreatology.2021; 21(5): 884. CrossRef - CA19.9 Serum Level Predicts Lymph-Nodes Status in Resectable Pancreatic Ductal Adenocarcinoma: A Retrospective Single-Center Analysis
Alessandro Coppola, Vincenzo La Vaccara, Michele Fiore, Tommaso Farolfi, Sara Ramella, Silvia Angeletti, Roberto Coppola, Damiano Caputo
Frontiers in Oncology.2021;[Epub] CrossRef
- Long‐term outcomes of neoadjuvant gemcitabine, nab‐paclitaxel, and S1 (GAS) in borderline resectable pancreatic cancer with arterial contact: Results from a phase II trial
- Indirect pathological indicators for cardiac sarcoidosis on endomyocardial biopsy
- Myung-Jin Cha, Jeong-Wook Seo, Seil Oh, Eun-Ah Park, Sang-Han Lee, Moon Young Kim, Jae-Young Park
- J Pathol Transl Med. 2020;54(5):396-410. Published online July 29, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.10
- 6,359 View
- 115 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The definitive pathologic diagnosis of cardiac sarcoidosis requires observation of a granuloma in the myocardial tissue. It is common, however, to receive a “negative” report for a clinically probable case. We would like to advise pathologists and clinicians on how to interpret “negative” biopsies.
Methods
Our study samples were 27 endomyocardial biopsies from 25 patients, three cardiac transplantation and an autopsied heart with suspected cardiac sarcoidosis. Pathologic, radiologic, and clinical features were compared.
Results
The presence of micro-granulomas or increased histiocytic infiltration was always (6/6 or 100%) associated with fatty infiltration and confluent fibrosis, and they showed radiological features of sarcoidosis. Three of five cases (60%) with fatty change and confluent fibrosis were probable for cardiac sarcoidosis on radiology. When either confluent fibrosis or fatty change was present, one-third (3/9) were radiologically probable for cardiac sarcoidosis. We interpreted cases with micro-granuloma as positive for cardiac sarcoidosis (five of 25, 20%). Cases with both confluent fibrosis and fatty change were interpreted as probable for cardiac sarcoidosis (seven of 25, 28%). Another 13 cases, including eight cases with either confluent fibrosis or fatty change, were interpreted as low probability based on endomyocardial biopsy.
Conclusions
The presence of micro-granuloma could be an evidence for positive diagnosis of cardiac sarcoidosis. Presence of both confluent fibrosis and fatty change is necessary for probable cardiac sarcoidosis in the absence of granuloma. Either of confluent fibrosis or fatty change may be an indirect pathological evidence but they are interpreted as nonspecific findings. -
Citations
Citations to this article as recorded by- Diagnostic Value of Comprehensive Echocardiographic Assessment Including Speckle-Tracking in Patients with Sarcoidosis Versus Healthy Controls: A Systematic Review and Meta-Analysis
Hritvik Jain, Maryam Shahzad, Muneeba Ahsan, Rahul Patel, Jagjot Singh, Ramez M. Odat, Aman Goyal, Raveena Kelkar, Nishad Barve, Hina Farrukh, Raheel Ahmed
Diagnostics.2025; 15(6): 708. CrossRef - Advances in cellular and tissue-based imaging techniques for sarcoid granulomas
Junwoo Kim, Girish Dwivedi, Berin A. Boughton, Ankur Sharma, Silvia Lee
American Journal of Physiology-Cell Physiology.2024; 326(1): C10. CrossRef - Lipomatous Metaplasia Is Associated With Ventricular Tachycardia Recurrence Following Ablation in Patients With Nonischemic Cardiomyopathy
Lingyu Xu, Mirmilad Khoshknab, Juwann Moss, Ronald D. Berger, Jonathan Chrispin, David Callans, Francis E. Marchlinski, Stefan L. Zimmerman, Yuchi Han, Natalia Trayanova, Benoit Desjardins, Saman Nazarian
JACC: Clinical Electrophysiology.2024; 10(6): 1135. CrossRef - Cardiac Sarcoidosis: A Comprehensive Clinical Review
András Vereckei, Zsuzsanna Besenyi, Viktória Nagy, Bence Radics, Hajnalka Vágó, Zsigmond Jenei, Gábor Katona, Róbert Sepp
Reviews in Cardiovascular Medicine.2024;[Epub] CrossRef - Cardiac sarcoidosis: phenotypes, diagnosis, treatment, and prognosis
Jukka Lehtonen, Valtteri Uusitalo, Pauli Pöyhönen, Mikko I Mäyränpää, Markku Kupari
European Heart Journal.2023; 44(17): 1495. CrossRef - Cardiac sarcoidosis: a comprehensive review of risk factors, pathogenesis, diagnosis, clinical manifestations, and treatment strategies
Hussain Haider Shah, Syeda Alishah Zehra, Aliza Shahrukh, Radeyah Waseem, Tooba Hussain, Muhammad Sheheryar Hussain, Fareeha Batool, Muhammad Jaffer
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Histology of Cardiac Sarcoidosis with Novel Considerations Arranged upon a Pathologic Basis
Shu Kato, Yasuhiro Sakai, Asako Okabe, Yoshiaki Kawashima, Kazuhiko Kuwahara, Kazuya Shiogama, Masato Abe, Hiroyasu Ito, Shin’ichiro Morimoto
Journal of Clinical Medicine.2022; 11(1): 251. CrossRef - Cardiac sarcoidosis: A multimodal approach to reach the diagnosis
Nicolas Piriou, Patrick Bruneval
International Journal of Cardiology.2021; 323: 264. CrossRef - Value of 3D mapping‐guided endomyocardial biopsy in cardiac sarcoidosis
Danielle M. Haanschoten, Ahmet Adiyaman, Nils A. ‘t Hart, Piet L. Jager, Arif Elvan
European Journal of Clinical Investigation.2021;[Epub] CrossRef - Cardiac Sarcoidosis: A Clinical Overview
Ana Carolina Alba, Shyla Gupta, Lakshmi Kugathasan, Andrew Ha, Alejandro Ochoa, Meyer Balter, Alvaro Sosa Liprandi, Maria Inés Sosa Liprandi
Current Problems in Cardiology.2021; 46(10): 100936. CrossRef
- Diagnostic Value of Comprehensive Echocardiographic Assessment Including Speckle-Tracking in Patients with Sarcoidosis Versus Healthy Controls: A Systematic Review and Meta-Analysis
- Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas
- Yuil Kim, Young-Hoon Joo, Min-Sik Kim, Youn Soo Lee
- J Pathol Transl Med. 2020;54(5):411-418. Published online July 21, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.22
- 8,463 View
- 181 Download
- 21 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
High-risk (HR) human papillomavirus (HPV) is found in a subset of head and neck (HN) squamous cell carcinomas (SCCs). For oropharyngeal SCCs, HR HPV positivity is known to be associated with good prognosis, and a separate staging system for HPV-associated carcinomas using p16 immunohistochemistry (IHC) as a surrogate test has been adopted in the 8th American Joint Committee on Cancer staging system. We examined the HR HPV status and the genotype distribution in five HN subsites.
Methods
Formalin-fixed paraffin-embedded tissue sections were used for p16 IHC and DNA extraction. HPV DNA detection and genotyping were done employing either a DNA chip-based or real-time polymerase chain reaction–based method.
Results
During 2011–2019, a total of 466 SCCs were tested for HPV DNA with 34.1% positivity for HR HPV. Among HN subsites, the oropharynx showed the highest HR HPV prevalence (149/205, 75.1%), followed by the sinonasal tract (3/14, 21.4%), larynx (5/43, 11.6%), hypopharynx (1/38, 2.6%), and oral cavity (1/166, 0.6%). The most common HPV genotype was HPV16 (84.3%) followed by HPV35 (6.9%) and HPV33 (4.4%). Compared with HR HPV status, the sensitivity and specificity of p16 IHC were 98.6% and 94.3% for the oropharynx, and 99.2% and 93.8% for the tonsil, respectively.
Conclusions
Using a Korean dataset, we confirmed that HR HPV is most frequently detected in oropharyngeal SCCs. p16 positivity showed a good concordance with HR HPV DNA for oropharyngeal and especially tonsillar carcinomas. The use of p16 IHC may further be extended to predict HR HPV positivity in sinonasal tract SCCs. -
Citations
Citations to this article as recorded by- Impact of histopathological parameters in prognosis of oral squamous cell carcinoma
R. P. Ekanayaka, W. M. Tilakaratne
Oral Diseases.2025; 31(5): 1420. CrossRef - Risk factors for cervical lymph node metastasis in oropharyngeal cancer and its impact on prognosis
Li Zhang, Zhilin Li, Jing Wang, Chen Wang, Shuxin Wen
Brazilian Journal of Otorhinolaryngology.2025; 91(2): 101520. CrossRef - Co-infection of human papillomavirus genotypes and Epstein-Barr virus in tumors of the oral cavity and oropharynx: a retrospective study in Northeastern Mexico
Gerardo del Carmen Palacios-Saucedo, Jose Manuel Vazquez-Guillen, Alondra Yamileth Alanis-Valdez, Leticia Lizeth Valdez-Treviño, Luis Roberto Galindo-Mendez, Angel Zavala-Pompa, Lydia Guadalupe Rivera-Morales, Ana Carolina Martinez-Torres, Roberto Lopez-V
IJID Regions.2025; 14: 100555. CrossRef - Rates of p16 and p53 expression in head and neck cutaneous squamous cell carcinoma vary according to human papillomavirus status
Rachid Ait Addi
World Journal of Clinical Cases.2025;[Epub] CrossRef - The epidemiological trends and survival of HPV-related oropharyngeal cancer other than tonsils and base of tongue − a systematic review and meta-analysis
Anas Mohammad Al Fadel, Kathrine Kronberg Jakobsen, Lasse Holmgaard Jensen, Amanda-Louise Fenger Carlander, Christian Grønhøj, Christian von Buchwald
Oral Oncology.2025; 165: 107311. CrossRef - Characteristics of human papillomavirus infection among oropharyngeal cancer patients: A systematic review and meta-analysis
Meimei Cui, Jinling Cheng, Huijuan Cheng, Ming Zhao, Dan Zhou, Min Zhang, Jingjing Jia, Limei Luo
Archives of Oral Biology.2024; 157: 105830. CrossRef - Longitudinal Screening for Oral High-Risk Non-HPV16 and Non-HPV18 Strains of Human Papillomavirus Reveals Increasing Prevalence among Adult and Pediatric Biorepository Samples: A Pilot Study
Jordan Jacobs, Eugene Chon, Karl Kingsley
Vaccines.2024; 12(8): 895. CrossRef - Position Statement about Gender-Neutral HPV Vaccination in Korea
Kyung-Jin Min, Yung-Taek Ouh, Sangrak Bae, Yong-Bae Ji, Jae-Kwan Lee, Jae-Weon Kim, Kwang-Jae Cho, Dong-Hun Im
Vaccines.2024; 12(10): 1110. CrossRef - Prevalence of human papilloma virus in head and neck mucous squamous cell carcinoma and genotypes by location: an observational study
Emilie Uhlrich, Jerzy Klijanienko, Joey Martin, Emmanuelle Jeannot, Anne Vincent-Salomon, Paul Freneaux, Christophe Le Tourneau, Olivier Choussy, Antoine Dubray-Vautrin
European Journal of Cancer Prevention.2024;[Epub] CrossRef - High-risk HPV Does not Appear to be an Important Risk Factor for Sinonasal Carcinomas in Turkish Population: A Tertiary Center Experience
Evsen Apaydin Arikan, Levent Aydemir, Murat Ulusan, Dilek Yilmazbayhan, Yasemin Ozluk
International Journal of Surgical Pathology.2023; 31(2): 124. CrossRef - Practical Application of Circulating Tumor-Related DNA of Human Papillomavirus in Liquid Biopsy to Evaluate the Molecular Response in Patients with Oropharyngeal Cancer
Agnieszka M. Mazurek, Tomasz W. Rutkowski
Cancers.2023; 15(4): 1047. CrossRef - The Prevalence of HPV in Oral Cavity Squamous Cell Carcinoma
Seyed Keybud Katirachi, Mathias Peter Grønlund, Kathrine Kronberg Jakobsen, Christian Grønhøj, Christian von Buchwald
Viruses.2023; 15(2): 451. CrossRef - The Protective Role of Cranberries and Blueberries in Oral Cancer
César Esquivel-Chirino, Mario Augusto Bolaños-Carrillo, Daniela Carmona-Ruiz, Ambar Lopéz-Macay, Fernando Hernández-Sánchez, Delina Montés-Sánchez, Montserrat Escuadra-Landeros, Luis Alberto Gaitán-Cepeda, Silvia Maldonado-Frías, Beatriz Raquel Yáñez-Ocam
Plants.2023; 12(12): 2330. CrossRef - Unusual cases of sinonasal malignancies: a letter to the editor on HPV-positive sinonasal squamous cell carcinomas
Benedicte Bitsch Lauritzen, Sannia Sjöstedt, Jakob Myllerup Jensen, Katalin Kiss, Christian von Buchwald
Acta Oncologica.2023; 62(6): 608. CrossRef - Prevalence of human Papillomavirus associated oropharyngeal and oral squamous cell carcinoma in Asian countries: A systematic review and large-scale meta-analysis
Yy Jean Tan, Ken Wong Siong Hou, Galvin Sim Siang Lin, Jasmine Lim Suk Wun, Wan Nor Amira Wan Ahmad Abdul Nasir, Lynn Wei Linn Ko
Acta Marisiensis - Seria Medica.2023; 69(2): 77. CrossRef - Top 100 most cited articles on human papillomavirus-induced head and neck squamous cell carcinoma: A bibliographic review
Rahul Mohandas, Subhashree Mohapatra, Mary Oshin, ShubhangiSambhaji Hajare
Journal of International Oral Health.2023; 15(3): 219. CrossRef - Intracellular Toll-Like Receptors Modulate Adaptive Immune Responses in Head and Neck Cancer
Sangeetha K. Nayanar, Deepak Roshan V.G., Shruthi Surendran, Göran Kjeller, Bengt Hasséus, Daniel Giglio
Viral Immunology.2023; 36(10): 659. CrossRef - Positive Rate of Human Papillomavirus and Its Trend in Head and Neck Cancer in South Korea
Hyun Woong Jun, Yong Bae Ji, Chang Myeon Song, Jae Kyung Myung, Hae Jin Park, Kyung Tae
Frontiers in Surgery.2022;[Epub] CrossRef - Transcriptionally active HPV in OPMD and OSCC: A systematic review following the CAP/ASCO guidelines
Laura Borges Kirschnick, Lauren Frenzel Schuch, Maria Eduarda Pérez‐de‐Oliveira, Ana Gabriela Costa Normando, Bruno Augusto Linhares Almeida Mariz, Eliete Neves Silva Guerra, Felipe Martins Silveira, Ana Carolina Uchoa Vasconcelos, Luciana Estevam Simonat
Oral Diseases.2022; 28(8): 2309. CrossRef - Effect of National Oral Health Screening Program on the Risk of Head and Neck Cancer: A Korean National Population-Based
Chan Woo Wee, Hyo-Jung Lee, Jae-Ryun Lee, Hyejin Lee, Min-Jeong Kwoen, Woo-Jin Jeong, Keun-Yong Eom
Cancer Research and Treatment.2022; 54(3): 709. CrossRef - Expression of p16, p53, and TLR9 in HPV-Associated Head and Neck Squamous Cell Carcinoma: Clinicopathological Correlations and Potential Prognostic Significance
Shu Wang, Xibing Zhuang, Caixia Gao, Tiankui Qiao
OncoTargets and Therapy.2021; Volume 14: 867. CrossRef - The Role of Human Papilloma Virus in Dictating Outcomes in Head and Neck Squamous Cell Carcinoma
Shane Brennan, Anne-Marie Baird, Esther O’Regan, Orla Sheils
Frontiers in Molecular Biosciences.2021;[Epub] CrossRef - A Contemporary Systematic Review on Repartition of HPV-Positivity in Oropharyngeal Cancer Worldwide
Amanda F. Carlander, Kathrine K. Jakobsen, Simone K. Bendtsen, Martin Garset-Zamani, Charlotte D. Lynggaard, Jakob Schmidt Jensen, Christian Grønhøj, Christian von Buchwald
Viruses.2021; 13(7): 1326. CrossRef - The Prevalence of High- and Low-Risk Types of HPV in Patients with Squamous Cell Carcinoma of the Head and Neck, Patients with Chronic Tonsillitis, and Healthy Individuals Living in Poland
Joanna Katarzyna Strzelczyk, Krzysztof Biernacki, Jadwiga Gaździcka, Elżbieta Chełmecka, Katarzyna Miśkiewicz-Orczyk, Natalia Zięba, Janusz Strzelczyk, Maciej Misiołek
Diagnostics.2021; 11(12): 2180. CrossRef
- Impact of histopathological parameters in prognosis of oral squamous cell carcinoma
- A retrospective cytohistological correlation of fine-needle aspiration cytology with classification by the Milan System for Reporting Salivary Gland Cytopathology
- Ji Hyun Park, Yoon Jin Cha, Ja Yeong Seo, Jae Yol Lim, Soon Won Hong
- J Pathol Transl Med. 2020;54(5):419-425. Published online July 8, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.09
- 5,847 View
- 194 Download
- 10 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Before publication of the new classification system named the Milan System for Reporting Salivary Gland Cytopathology (MSRSGC) in 2018, there was no standard classification for salivary gland lesions obtained by fine-needle aspiration (FNA). We therefore aimed to evaluate the diagnostic utility of this system by retrospectively reviewing FNA samples using the MSRSGC and to determine their risk of developing into neoplasms and becoming malignant.
Methods
Retrospective slide review and classification of salivary gland FNAs obtained over a 6-year period (2013–2018) at a single center were performed by two pathologists. The risks of neoplasm and malignancy for each category also were calculated.
Results
This study surveyed 374 FNAs (371 patients) performed over a six-year period and selected 148 cases that included documented surgical follow-up (39.6%). Among the surgically treated cases, the distributions of FNA categories were as follows: non-diagnostic (ND; 16.9%), non-neoplastic (NN; 2.7%), atypia of undetermined significance (AUS; 3.4%), benign (BN; 54.7%), salivary gland neoplasm of uncertain malignant potential (SUMP; 10.1%), suspicious for malignancy (SM; 6.8%), and malignant (M; 5.4%). The risk of malignancy (ROM) was 24.0% for ND, 0% for NN, 40.0% for AUS, 2.5% for BN, 46.7% for SUMP, 100% for SM, and 87.5% for M. The overall diagnostic accuracy was 95.9% (142/148 cases).
Conclusions
The newly proposed MSRSGC appears to be a reliable system for classification of salivary gland lesions according to the associated ROM. -
Citations
Citations to this article as recorded by- The Impact of Lesion-Specific and Sampling-Related Factors on Success of Salivary Gland Fine-Needle Aspiration Cytology
Marcel Mayer, Mohammad Marwan Alfarra, Kathrin Möllenhoff, Marianne Engels, Christoph Arolt, Alexander Quaas, Philipp Wolber, Louis Jansen, Lisa Nachtsheim, Maria Grosheva, Jens Peter Klussmann, Sami Shabli
Head and Neck Pathology.2025;[Epub] CrossRef - The Myriad Spectrum of Salivary Gland Lesions: Cytohistological Correlation on Fine Needle Aspiration Cytology, Core Needle Biopsy, and Resections in a 5‐Year Single Institutional Experience of North India
Zachariah Chowdhury, Pallavi Majumdar, Sumeet Narain, Komal Lamba
Diagnostic Cytopathology.2025; 53(8): 391. CrossRef - The Milan system for reporting salivary gland cytopathology – Assessment of utility and the risk of malignancy
Annu E. Prakash, Renu Sukumaran, Nileena Nayak, K. Lakshmi, Anitha Mathews, Jayasree Kattoor
Indian Journal of Cancer.2024; 61(3): 575. CrossRef - Salivary gland fine-needle aspiration biopsy: quality assurance results from a tertiary cancer center
Fanni Ratzon, Dominique L. Feliciano, Nora Katabi, Bin Xu, Oscar Lin, Xiao-Jun Wei
Journal of the American Society of Cytopathology.2023; 12(3): 206. CrossRef - Cytohistological correlation and risk stratification of salivary gland lesions using the Milan System for Reporting Salivary Gland Cytopathology: A tertiary care centre experience
Tarun Kumar, Prerna Tewari, Jitendra Singh Nigam, Shreekant Bharti, Surabhi, Ruchi Sinha, Punam Prasad Bhadani
Cytopathology.2023; 34(3): 225. CrossRef - Assessment of Risk of Malignancy of Fine-needle Aspiration Cytology in Salivary Gland Lesions Using the Milan System for Reporting Salivary Gland Cytopathology Categorization: A Systematic Review and Meta-analysis
Amit Kumar, Subhash Chandra, Bishnupati Singh, Swati Sharma, Ankita Tandon, Ajoy Kumar Shahi
The Journal of Contemporary Dental Practice.2023; 23(10): 1039. CrossRef - Milan Sınıflandırma Sistemi’ne Göre Değerlendirilen Tükürük Bezi İnce İğne Aspirasyon Sitolojilerinin Histopatolojik Tanı Uyumu
Özlem SARAYDAROĞLU, Selin YİRMİBEŞ
Uludağ Üniversitesi Tıp Fakültesi Dergisi.2023; 49(3): 285. CrossRef - Milan system for reporting salivary gland cytopathology: Adoption and outcomes in a community setting
Samih J. Nassif, Ali R. Sasani, Garrey T. Faller, Jennifer L. Harb, Jagdish K. Dhingra
Head & Neck.2022; 44(6): 1462. CrossRef - Nondiagnostic salivary gland FNAs are associated with decreased risk of malignancy compared with “all‐comer” patients: Analysis of the Milan System for Reporting Salivary Gland Cytopathology with a focus on Milan I: Nondiagnostic
Shu K. Lui, Troy Tenney, Patrick C. Mullane, Kartik Viswanathan, Daniel J. Lubin
Cancer Cytopathology.2022; 130(10): 800. CrossRef - Application of the Milan System for Reporting Salivary Gland Cytopathology: A systematic review and meta‐analysis
Zhaoyang Wang, Huan Zhao, Huiqin Guo, Changming An
Cancer Cytopathology.2022; 130(11): 849. CrossRef - Multiplexed single‐cell analysis of FNA allows accurate diagnosis of salivary gland tumors
Juhyun Oh, Tae Yeon Yoo, Talia M. Saal, Lisa Tsay, William C. Faquin, Jonathan C.T. Carlson, Daniel G. Deschler, Sara I. Pai, Ralph Weissleder
Cancer Cytopathology.2022; 130(8): 581. CrossRef - Cytologic analysis of vitreous fluids: A retrospective review of our 24 years of experience
Gabriel L. Collins, Elizabeth W. Hubbard, Christopher T. Clark, Lisa D. Duncan, Laurentia Nodit
Diagnostic Cytopathology.2021; 49(10): 1122. CrossRef
- The Impact of Lesion-Specific and Sampling-Related Factors on Success of Salivary Gland Fine-Needle Aspiration Cytology
Case Study
- Renal intravascular large B cell lymphoma: the first case report in Korea and a review of the literature
- Moonsik Kim, Haerim Chung, Woo Ick Yang, Hyeon Joo Jeong
- J Pathol Transl Med. 2020;54(5):426-431. Published online August 13, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.18
- 5,070 View
- 120 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Herein, we describe the first case of renal intravascular large B cell lymphoma in Korea occurring in a 66-year-old female. She presented with mild fever and dyspnea. On physical and laboratory evaluations, hemophagocytic lymphohistiocytosis was suspected, but the bone marrow biopsy results were unremarkable. During the work-up, massive proteinuria developed, which led to a renal biopsy. The renal architecture was relatively well-preserved, but the glomeruli were hypercellular with the infiltration of atypical, large lymphoid cells with increased nucleus-cytoplasm ratio and clumped chromatin. Similar cells were also present in the peritubular capillaries. The tumor cells exhibited membranous staining for CD20 and CD79a. After the diagnosis of intravascular large B cell lymphoma, the patient received rituximab-based chemotherapy under close follow-up.
-
Citations
Citations to this article as recorded by- Intravascular large B-cell lymphoma of the central nervous system with renal involvement: a case report and literature review
Jun Li, Zhaojiao Li, Yifeng Shi, Jiajie Chen, Heng Zhao, Xueye Mao, Shan Li, Huiying Wang, Qiang Meng, Lingchun Liu
Frontiers in Oncology.2025;[Epub] CrossRef - EBV-Positive Intravascular Large B-Cell Lymphoma of the Small Intestine: A Case Report and Literature Review
Chenglong Pan, Xiaoling Ma, Yanfei Yao, Chunyan Wang
International Journal of Surgical Pathology.2024; 32(3): 586. CrossRef - Intravascular large B‐cell lymphoma in renal cell carcinoma incidentally detected by robot‐assisted partial nephrectomy
Michio Noda, Yutaka Enomoto, Yukari Shirasugi, Sumiyo Ando, Yukimasa Matsuzawa, Haruki Kume
IJU Case Reports.2022; 5(3): 191. CrossRef - Case Report: Intravascular Large B-Cell Lymphoma: A Clinicopathologic Study of Four Cases With Review of Additional 331 Cases in the Literature
Yingying Han, Qingjiao Li, Dan Wang, Lushan Peng, Tao Huang, Chunlin Ou, Keda Yang, Junpu Wang
Frontiers in Oncology.2022;[Epub] CrossRef - Renal Involvement of CD20-Negative Intravascular Large B Cell Lymphoma with Neurological Manifestations
Faten Aqeel, Serena M. Bagnasco, Duvuru Geetha, Yoshihide Fujigaki
Case Reports in Nephrology.2022; 2022: 1. CrossRef
- Intravascular large B-cell lymphoma of the central nervous system with renal involvement: a case report and literature review
Brief Case Report
- Breast implant–associated anaplastic large cell lymphoma: the first South Korean case
- Jongwon Lee, Hyungwoo Cho, Dok Hyun Yoon, Eun Key Kim, Gyungyub Gong, Cheolwon Suh, Joo-ryung Huh
- J Pathol Transl Med. 2020;54(5):432-434. Published online August 18, 2020
- DOI: https://doi.org/10.4132/jptm.2020.07.01
- 4,832 View
- 136 Download
- 5 Web of Science
- 5 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Breast Reconstruction after Breast Implant-Associated Anaplastic Large Cell Lymphoma Treatment: A Case Report and Literature Review
Won-Seob Lee, Tae-Gon Kim, Jun-Ho Lee, Il-Kug Kim
Journal of Clinical Medicine.2023; 12(5): 1885. CrossRef - Breast filler granuloma mistaken for implant rupture: A case report
Yong Seon Hwang, Je Yeon Byeon, Jun Hyuk Kim, Hwan Jun Choi, Mee Hye Oh, Da Woon Lee
Medicine.2023; 102(22): e33785. CrossRef - Implant replacement and anaplastic large cell lymphoma associated with breast implants: a quantitative analysis
Martina Vittorietti, Sergio Mazzola, Claudio Costantino, Daniele Domenico De Bella, Santo Fruscione, Nicole Bonaccorso, Martina Sciortino, Davide Costanza, Miriam Belluzzo, Alessandra Savatteri, Fabio Tramuto, Paolo Contiero, Giovanna Tagliabue, Palmira I
Frontiers in Oncology.2023;[Epub] CrossRef - Breast implant-associated anaplastic large cell lymphoma: a case report with a history of spontaneously resolved late seroma
Do Yeon Kim, Joon Hur, Woo Yeon Han, Kyunghyun Min, Jong Won Lee, Jin Sup Eom, Hyun Ho Han, Eun Key Kim
Archives of Aesthetic Plastic Surgery.2021; 27(4): 143. CrossRef - Comment on “Breast implant-associated anaplastic large cell lymphoma: the first South Korean case”
Il-Kug Kim, Tae Gon Kim
Journal of Pathology and Translational Medicine.2021; 55(6): 419. CrossRef
- Breast Reconstruction after Breast Implant-Associated Anaplastic Large Cell Lymphoma Treatment: A Case Report and Literature Review
Corrigendum
- Correction of author’s name: Atypical femoral neck fracture after prolonged bisphosphonate therapy
- Kwang-kyoun Kim, Yong Wook Park, Tae-hyeong Kim, Kyung-deok Seo
- J Pathol Transl Med. 2020;54(5):435-435. Published online September 10, 2020
- DOI: https://doi.org/10.4132/jptm.2020.09.07
- Corrects: J Pathol Transl Med 2020;54(4):346
- 2,821 View
- 64 Download

 E-submission
E-submission












 First
First Prev
Prev



