Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(3); 2012 > Article
-
Case Report
Extranodal Follicular Dendritic Cell Sarcoma with Rapid Growth in Parapharynx: A Case Report - Jung-Soo Pyo, Guhyun Kang1, Sung-Im Do, Seoung Wan Chae, Kyungeun Kim, Sang Hyuk Lee2, Yoon-La Choi3, Joon Hyuk Choi4, Jin Hee Sohn, Dong-Hoon Kim
-
Korean Journal of Pathology 2012;46(3):306-310.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.3.306
Published online: June 22, 2012
Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
1Department of Pathology, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
2Department of Otorhinolaryngology-Head and Neck Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
4Department of Pathology, Yeungnam University College of Medicine, Daegu, Korea.
- Corresponding Author: Dong-Hoon Kim, M.D. Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 29 Saemunan-ro, Jongno-gu, Seoul 110-746, Korea. Tel: +82-2-2001-2392, Fax: +82-2-2001-2398, idavidkim@yahoo.co.kr
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Follicular dendritic cell sarcoma (FDCS) is a rare malignancy arising from the antigen-presenting cells in the lymph node and extranodal tissue. We describe a 31-year-old male patient who presented with a swelling of the left parapharynx. The radiologic findings showed a 4.7×4.5×1.9 cm-sized, ill-defined mass in the left parapharyngeal space. A fine-needle aspiration cytology was performed and it showed scattered, irregular, cohesive clusters of tumor cells with a spindle-to-ovoid shape with irregular contours in a background of lymphocytes. Based on these findings, a diagnosis of spindle cell neoplasm was made. The surgically resected tumor was composed of elongated, ovoid or polygonal cells showing positive immunohistochemistry for CD21, CD23, and CD35. Postoperatively, the residual tumor was observed to undergo a rapidly growth. There is an overlap in the cytologic and histologic findings between FDCS of the parapharynx and other tumors. Pathologists should therefore be aware of its characteristics not only to provide an accurate diagnosis but also to recommend the appropriate clinical management.
- A 31-year-old man presented with a swelling of the left parapharynx. Physical examination revealed a hard, non-tender mass with round shape in left posterior pharyngeal area with no enlarged lymph nodes in the neck.
- On initial computed tomography (CT) scans, there were an ill-defined, heterogeneous mass in the left parapharyngeal space but no remarkable enlarged lymph nodes in the neck (Fig. 1A). On magnetic resonance image scans, there were a 4.7×4.5×1.9 cm-sized lobulated enhancing mass with a hyperintensity on T2WI (Fig. 1B) and an isointensity on T1WI. The impression of radiologists was neurogenic tumor or pleomorphic adenoma. On positron emission tomography-CT scans, the mass of left parapharyngeal area showed a focal hypermetabolic lesion (SUV =6.1) (Fig. 1C).
- On the fine-needle aspiration cytology, there was a high cellular smear. The scattered, irregular, cohesive clusters of tumor cells showed irregular contours with mature lymphocytes scattered in the background (Fig. 2A). The spindle-to-ovoid tumor cells had an indistinctive cell border and a moderate amount of pale eosinophilic cytoplasm. In tumor cells, oval-shaped nuclei showed mild atypia with a fine chromatin pattern and they occasionally had small distinctive nucleoli (Fig. 2B). Nuclear pseudoinclusions were seen in some tumor cells (Fig. 2B inset). We made a diagnosis of a spindle cell neoplasm including paraganglioma.
- Grossly, the surgically resected specimen showed a fibrotic cut surface with a grayish white color (Fig. 3A). Histopathologically, there was a complete replacement of the normal tissue by the tumor. The tumor was composed of the elongated, ovoid or polygonal cells and it exhibited a fascicular growth pattern in certain areas. The tumor cells had more or less abundant eosinophilic cytoplasm with ill-defined cell borders. They had not only round-to-oval nuclei with a smooth nuclear membrane but also vesicular or granular chromatin and distinct nucleoli. In addition, they also had a nuclear pleomorphism with a sparse mitotic count (0-1/10 HPFs). Small lymphocytes were scattered throughout the tumor (Fig. 3B). Hemorrhages, but not necrosis, were detected in the peripheral area.
- On immunohistochemistry, the tumor cells were positive for CD21, CD23, and CD35, all of which are markers specific for follicular dendritic cell differentiation (Fig. 3C-E). However, the tumor cells were negative for pancytokeratin (AE1/3), cytokeratin 19, human melanoma black-45, chromogranin, synaptophysin, CD56, leukocyte common antigen, smooth muscle actin, desmin, and S-100 protein. The ki-67 labeling index was about 10%.
- In the current case, a diagnosis of FDCS of the parapharynx was therefore confirmed, based on the histologic and immunohistochemical findings.
- A follow-up CT scan was performed on postoperative day 19, and it revealed a peripheral enhancing lesion with an ill-defined margin on the inferior side of the primary lesion (Fig. 1D). These findings are suggestive of the residual tumor, that was rapidly grew. The tumor extend that its greatest dimension reached 3 cm in the short-term postoperative period. The patient underwent the postoperative adjuvant radiotherapy.
CASE REPORT
- FDCS typically arises in lymph nodes of the neck, axilla and mediastinum, and it also occurs less commonly in extranodal tissues from variable sites, including head and neck, liver, spleen, gastrointestinal tract, soft tissue, skin, lung, and breast.
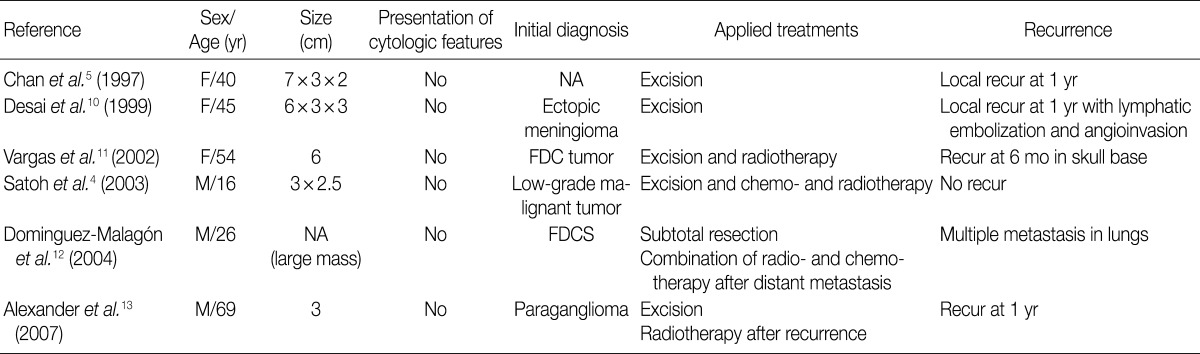
- According to a review of English literatures, six cases of FDCS arising in the parapharyngeal space have recently been described. But there is no case reported in Korea.4,5,10-13 The clinical data of previously reported six cases of FDCS of the parapharynx are summarized in Table 1.4,5,10-13 Of these six cases, two were initially diagnosed as FDCS but the remaining four were diagnosed as ectopic meningioma, paraganglioma or others. The tumors of the parapharynx are histopathologically characterized by the elongated, ovoid or polygonal cells with scattered mature lymphocytes. Based on these findings, they can be differentially diagnosed from carcinoma, malignant fibrous histiocytoma or schwannoma. Positive immunohistochemistry for CD21, CD23, and CD35 are helpful to make a differential diagnosis of FDCS from other neoplasm-showing similar morphology. We initially considered a diagnosis of paraganglioma, but established a diagnosis of FDCS on immunohistochemistry.
- Previous studies have shown that a fine-needle aspiration cytology of the FDCS the ovoid or spindle-shaped cells with intermediate-sized nuclei with a smooth border and small, indistinct nucleoli.9 These cytologic features are also seen in other neoplasms including undifferentiated carcinoma, ectopic meningioma and paraganglioma. It would therefore be mandatory to make a differential diagnosis of FDCS on a fine-needle aspiration cytology. In some cases of FDCS of the parapharynx, however, these cytological characteristics are not present.10 In addition, mature lymphocytes in the background are not useful to make a differential diagnosis of FDCS from neoplasms showing similar cytology. Surgical excision should therefore be performed to confirm a diagnosis of FDCS.
- Of the six cases of FDCS of the parapharynx, that had been reported previously, five showed both a local recurrence and a distant metastasis. There were two cases of FDCS of the paraphrynx with the greatest diameter of <5 cm, one of which underwent no adjuvant therapy and had a local recurrence.13 Most cases of FDCS of the parapharynx showed a more aggressive behavior with a local recurrence or a distant metastasis as compared with that of other regions.6,8 The current case showed a low mitotic count and a small-sized mass, indicating a better prognosis,8 but it did an aggressive behavior with a local recurrence and a rapid growth.
- It is therefore necessary to examine the pathogenesis of FDCS, which would be essential for predicting a prognosis and selecting the optional treatment modalities. There is an overlap in the cytological and histologic findings between FDCS and other tumors. Misdiagnosis can be avoided, however, if pathologists are more aware of its characteristic features.
DISCUSSION
- 1. Park CS, Choi YS. How do follicular dendritic cells interact intimately with B cells in the germinal centre? Immunology 2005; 114: 2-10. ArticlePubMedPMC
- 2. Monda L, Warnke R, Rosai J. A primary lymph node malignancy with features suggestive of dendritic reticulum cell differentiation: a report of 4 cases. Am J Pathol 1986; 122: 562-572. PubMedPMC
- 3. Duan GJ, Wu F, Zhu J, et al. Extranodal follicular dendritic cell sarcoma of the pharyngeal region: a potential diagnostic pitfall, with literature review. Am J Clin Pathol 2010; 133: 49-58. ArticlePubMed
- 4. Satoh K, Hibi G, Yamamoto Y, Urano M, Kuroda M, Nakamura S. Follicular dendritic cell tumor in the oro-pharyngeal region: report of a case and a review of the literature. Oral Oncol 2003; 39: 415-419. ArticlePubMed
- 5. Chan JK, Fletcher CD, Nayler SJ, Cooper K. Follicular dendritic cell sarcoma: clinicopathologic analysis of 17 cases suggesting a malignant potential higher than currently recognized. Cancer 1997; 79: 294-313. ArticlePubMed
- 6. Biddle DA, Ro JY, Yoon GS, et al. Extranodal follicular dendritic cell sarcoma of the head and neck region: three new cases, with a review of the literature. Mod Pathol 2002; 15: 50-58. ArticlePubMedPDF
- 7. De Pas T, Spitaleri G, Pruneri G, et al. Dendritic cell sarcoma: an analytic overview of the literature and presentation of original five cases. Crit Rev Oncol Hematol 2008; 65: 1-7. ArticlePubMed
- 8. Li L, Shi YH, Guo ZJ, et al. Clinicopathological features and prognosis assessment of extranodal follicular dendritic cell sarcoma. World J Gastroenterol 2010; 16: 2504-2519. ArticlePubMedPMC
- 9. Wright CA, Nayler SJ, Leiman G. Cytopathology of follicular dendritic cell tumors. Diagn Cytopathol 1997; 17: 138-142. ArticlePubMed
- 10. Desai S, Deshpande RB, Jambhekar N. Follicular dendritic cell tumor of the parapharyngeal region. Head Neck 1999; 21: 164-167. ArticlePubMed
- 11. Vargas H, Mouzakes J, Purdy SS, Cohn AS, Parnes SM. Follicular dendritic cell tumor: an aggressive head and neck tumor. Am J Otolaryngol 2002; 23: 93-98. ArticlePubMed
- 12. Domínguez-Malagón H, Cano-Valdez AM, Mosqueda-Taylor A, Hes O. Follicular dendritic cell sarcoma of the pharyngeal region: histologic, cytologic, immunohistochemical, and ultrastructural study of three cases. Ann Diagn Pathol 2004; 8: 325-332. ArticlePubMed
- 13. Alexander AA, Zapanta PE, Khan A. Diagnosis and recurrence of follicular dendritic cell sarcoma. Otolaryngol Head Neck Surg 2007; 137: 832-834. ArticlePubMedPDF
REFERENCES
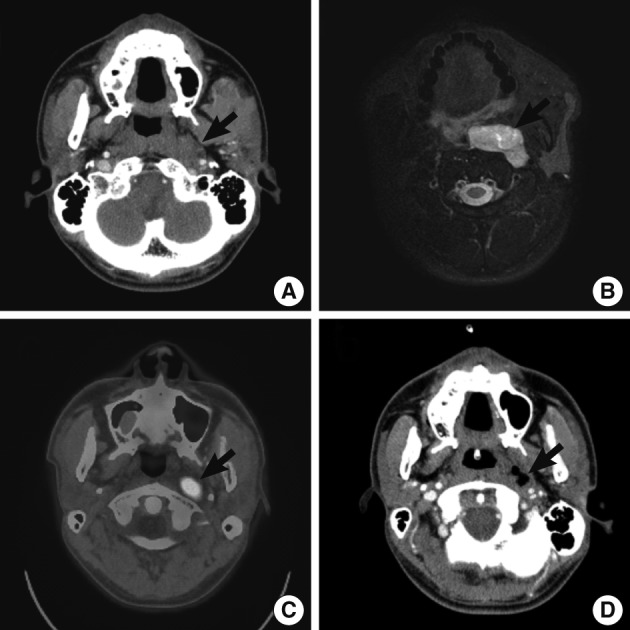
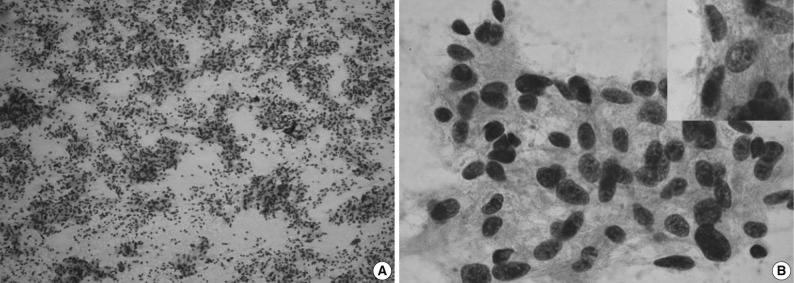

Figure & Data
References
Citations

- Extranodal Follicular Dendritic Cell Sarcoma of the Head and Neck Region: A Clinicopathological Study of 7 Cases
Nasir Ud Din, Zubair Ahmad, Shabina Rahim, Karen Fritchie, Muhammad Usman Tariq, Arsalan Ahmed
International Journal of Surgical Pathology.2023; 31(6): 1067. CrossRef - Cytomorphology of follicular dendritic cell sarcoma: a report of 7 cases with an emphasis on the diagnostic challenges
Cody Weimholt, Jalal B. Jalaly, Cedric Bailey
Journal of the American Society of Cytopathology.2023; 12(3): 229. CrossRef - Follicular dendritic cells
Seham A. Abd El‐Aleem, Entesar Ali Saber, Neven M. Aziz, Hani El‐Sherif, Asmaa M. Abdelraof, Laiche Djouhri
Journal of Cellular Physiology.2022; 237(4): 2019. CrossRef - Clinicopathological characteristics of extranodal follicular dendritic cell sarcoma: A report of two cases
Xing Zhao, Dayong Sun, Gang Zhang
Oncology Letters.2021;[Epub] CrossRef - Cytological diagnosis of follicular dendritic cell sarcoma: A case report and review of literature
A. Dutta, P. Arun, P. Roy, I. Arun
Cytopathology.2018; 29(5): 461. CrossRef - Follicular dendritic cells and related sarcoma
Fabio Facchetti, Luisa Lorenzi
Seminars in Diagnostic Pathology.2016; 33(5): 262. CrossRef - Extranodal follicular dendritic cell sarcoma: A clinicopathological report of four cases and a literature review
RUI-FEN WANG, WEI HAN, LEI QI, LI-HUI SHAN, ZHENG-CAI WANG, LI-FENG WANG
Oncology Letters.2015; 9(1): 391. CrossRef - Follicular Dendritic Cell Sarcoma of Parapharyngeal Space: A Case Report and Review of the Literature
Turki Al-Hussain, Muhammad Saleem, Suresh Babu Velagapudi, Mohammad Anas Dababo
Head and Neck Pathology.2015; 9(1): 135. CrossRef - Clinical and pathological features of head and neck follicular dendritic cell sarcoma
Ji Li, Min-Li Zhou, Shui-Hong Zhou
Hematology.2015; 20(10): 571. CrossRef



Fig. 1
Fig. 2
Fig. 3
FDCS, follicular dendritic cell sarcoma; F, female; NA, not available; FDC, follicular dendritic cell.

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article




